
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
This comprehensive resource for fellows/trainees and candidates for recertification in gastroenterology summarizes the field in a modern, fresh format. Prominent experts from around the globe write on their areas of expertise, and each chapter follows a uniform structure. The focus is on key knowledge, with the most important clinical facts highlighted in boxes. Color illustrations reinforce the text.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Practical Gastroenterology and Hepatology by in PDF and/or ePUB format, as well as other popular books in Medicina & Gastroenterología y hepatología. We have over one million books available in our catalogue for you to explore.
Information
PART 1
Pathobiology of the Intestine and Pancreas
CHAPTER 1
Clinical Anatomy, Embryology, and Congenital Anomalies
Summary
As clinicians and educators we update ourselves routinely with various aspects of our practicing field. Mainly, the focus is centered on the pathogenesis, diagnosis, and management aspects of the clinical problem. Rarely, we delve in to the anatomy of the organ system responsible for the presentation. However, some embryological anomalies can present in later decades of life and present unexpected and difficult challenges in both diagnosis and management. Hence, a practical working knowledge on this subject is critical for the clinical gastroenterologist.
We have compiled a chapter that deals succinctly with the clinical anatomy, embryology, and congenital anomalies of the gastrointestinal tract. The main body of the chapter is in line with the evolving division of the gastrointestinal tract of the embryo into foregut, midgut, and the hindgut. We briefly cover the anatomy, embryogenesis, and the congenital anomalies of each derivative of the germ layer starting from the foregut, and ending with the Hirschsprung disease (HSCR), a congenital anomaly of the ganglion cells of the hindgut. Some of the more commonly seen anomalies, such as pancreas divisum (PD), are dealt in detail wherever required.
Small and Large Intestine
Anatomy and Embryogenesis
At 4 weeks of gestation, the alimentary tract is divided into three parts: foregut, midgut, and hindgut. The duodenum originates from the terminal portion of the foregut and cephalic part of the midgut. With rotation of the stomach, the duodenum becomes C-shaped and rotates to the right. The midgut gives rise to the duodenum distal to the ampulla, to the entire small bowel, and to the cecum, appendix, ascending colon, and the proximal two-thirds of the transverse colon. The distal third of the transverse colon, the descending colon and sigmoid, the rectum, and the upper part of the anal canal originate from the hindgut. The anal canal’s proximal portion is formed from the hindgut endoderm whereas the distal portion arises from the ectoderm of the cloacal membrane.
The colon has a rich blood supply, with a specific vascular arcade formed by union of branches of superior mesenteric, inferior mesenteric, and internal iliac arteries. Despite its presence, the colon vasculature has two weak points: the splenic flexure and the rectosigmoid junction which are supplied by the narrow terminal branches of superior mesenteric artery (SMA) and inferior mesenteric artery (IMA), respectively. These two watershed areas are most vulnerable to ischemia during systemic hypotension.
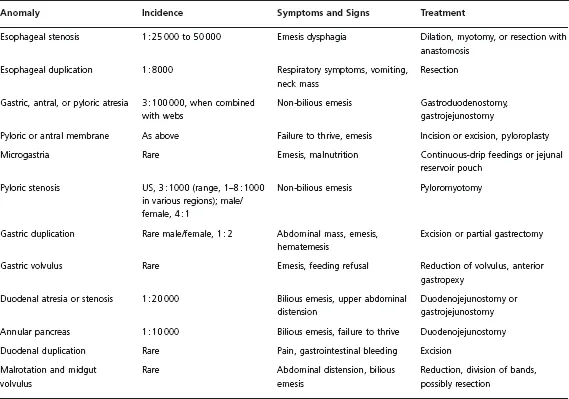
Aberrations in midgut development may result in a variety of anatomic anomalies (Table 1.1 ), and these are broadly classified as:
- Rotation and fixation
- Duplications
- Atresias and stenoses: these occur most frequently and are either due to failure of recanalization or a vascular accident. Atresias have a reported incidence rate of 1 in 300 to 1 in 1500 live births, and are more common than stenoses. Atresias are more common in black infants, low birth-weight infants, and twins. Clinically, the presentation is that of a proximal intestinal obstruction with bilious vomiting on the first day of life. Treatment is surgical correction.
Table 1.1 Congenital anomalies of upper gastrointestinal tract.
The other major congenital anomalies of the intestine and abdominal cavity are related to abnormalities with development of abdominal wall, the vitelline duct, and innervation of the gastrointestinal tract.
Abdominal Wall Congenital Anomalies
The congenital anomalies of the abdominal wall are:
- Gastrochisis: caused by an intact umbilical cord with evisceration of the bowel, but no covering membranes, through a defect in the abdominal wall [1] . Gastrochisis is commonly associated with intestinal atresia and cryptorchism.
- Omphalocele: characterized by herniation of the bowel, liver, and other organs into the intact umbilical cord; unlike gastrochisis, these tissues are covered by a membrane formed from fusion of the amnion and peritoneum.
Diagnosis
An abdominal wall defect may be diagnosed during routine prenatal ultrasonography. Both gastroschisis and omphalocele are associated with elevation of maternal serum α-fetoprotein.
Management
Recommended management for both these conditions is operative reduction of the contents back in to the abdominal cavity. The size of the omphalocele deter-mines whether a primary repair or delayed primary closure is selected as the surgical approach.
Vitelline Duct Congenital Anomalies
Persistence of the duct communication between the intestine and the yolk sac beyond the embryonic stage may result in several anomalies of the omphalomesen-teric or vitelline duct.
The most common congenital abnormality of the gastrointestinal tract is omphalomesenteric duct, or Meckel diverticulum, which results from the failure of the vitelline duct to obliterate during the fifth week of fetal development [2] .
Clinical presentation
Meckel diverticulum may remain completely asymptomatic or it may mimic such disorders as Crohn disease, appendicitis, and peptic ulcer disease. Bleeding is the most common complication of Meckel diverticulum, related to acid-induced ulceration of adjacent small intestine from the presence of ectopic gastric mucosa. Obstruction, intussusception, diverticulitis, and perforation may also occur, especially in adults, due to the active ectopic pancreatic tissue or gastric mucosa.
Diagnosis
The most useful method of detection of a Meckel diverticulum is technetium-99m pertechnetate scanning. Technetium uptake depends on the presence of hetero-topic gastric tissue. The test has 85% sensitivity and 95% specificity. The sensitivity of the scan can be increased minimally with use of cimetidine [3] . Other tests useful in diagnosis are superior mesenteric artery angiography, laparoscopy, and double balloon enteroscopy.
Management
Meckel diverticulectomy either by laparoscopy or open laparotomy approach is the procedure of choice for symptomatic diverticulum.
Less Common Vitelline Duct Abnormalities
Other, less common congenital abnormalities of vitelline duct include:
- Omphalomes-enteric or vitelline cyst: central cystic dilatation in which the duct is closed at both ends but patent in its center
- Umbilical-intestinal fistula: a patent duct throughout its length
- Omphalomesenteric band: complete obliteration of the duct, resulting in a fibrous cord or ligament extending from the ileum to the umbilicus.
Enteric Nervous System Anomalies
The most common enteric nervous system congenital anomaly is Hirschsprung (HSCR) disease; other associated anomalies include intestinal neuronal dysplasia (IND) and chronic intestinal pseudo-obstruction.
HSCR is characterized by the absence of ganglion cells in the submucosal (Meissner) and myenteric (Auerbach) plexuses along a variable length of the hindgut. It is classified as short-segment HSCR (80% of cases), when the aganglionic segment does not extend beyond the upper sigmoid, and long-segment HSCR when aganglionosis extends proximal to the sigmoid. Twelve percent of children with Hirschsprung disease have chromosomal abnormalities, 2 to 8% of which are trisomy 21 (Down syndrome) [4].
Clinical Presentation
In most cases, HSCR presents at birth as non-passage of meconium, abdominal distension, feeding difficulties, and/or bilious emesis. Some patients are diagnosed later in infancy or in adulthood with severe constipation, chronic abdominal distension, vomiting, and failure to thrive.
Diagnosis
The diagnosis in a symptomatic individual may be made by one or a combination of the following tests: barium enema, rectal biopsy, and anal manometry.
Management
Definitive treatment of Hirschsprung disease is surgical, and the specific method of surgery is operator dependent
Pancreas
Anatomy and Embryogenesis
The pancreas first appears during the fourth week of gestation as ventral and dorsal outpouchings from the endodermal lining of the duodenum. The normal adult pancreas results from the fusion of these dorsal and ventral pancreatic buds during the second month of fetal development. The tail, body, and part of the head of the pancreas are formed by the dorsal component; the remainder of the head and the uncinate process derive from the ventral pancreas.
Figure 1.1 Schematic illustration of embryology of normal pancreas and pancreas divisum. (Reproduced with kind permission from Springer & Business Media. Kamisawa T. Clinical significance of the minor duodenal papilla and accessory pancreatic duct. Journal of Gastroenterology 2004; 39 : 606.)
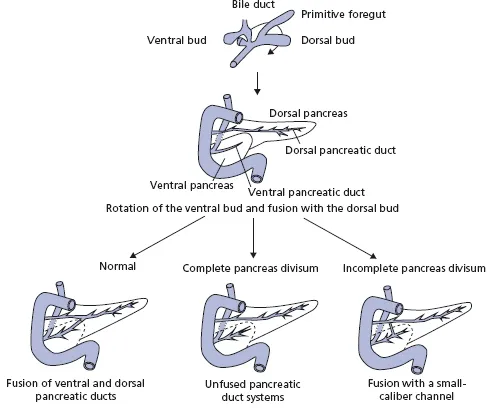
The dorsal duct arises directly from the duodenal wall, and the ventral duct arises from the common bile duct. On fusion of the ventral and dorsal components of the pancreas, the ventral duct anastomoses with the dorsal one, forming the main pancreatic duct of Wirsung (Figure 1.1 ). The proximal end of the dorsal duct becomes the accessory duct of Santorini in the adult [5] . The pancreatic acini appear in the third month of gestation as derivatives of the side ducts and termini of these primitive ducts.
Pancreas Divisum ( PD )
PD occurs when the dorsal and ventral ducts fail to fuse; the dorsal duct drains the majority of the pancreas via the minor papilla, while the short ventral duct drains the inferior portion of the head via the major papilla (Figure 1.1 ). Pancreas divisum has been observed in 5 to 10% of autopsy series and in about 2 to 7% of patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) [6] . Most patients with pancreas divisum are asymptomatic, and the diagnosis is made incidentally. However, some patients develop abdominal pain, recurrent acute pancreatitis, or chronic pancreatitis. The causal relationship between divisum and pancreatitis is still a matter of debate. PD is usually diagnosed by ERCP although endoscopic ultrasonography and magnetic resonance cholangiopancreatography (MRCP) may be useful for diagnosis [7] . Therapeutic intervention (either endoscopic sphincterotomy with placement of stents through the accessory papilla or surgical sphincteroplasty of the accessory papilla) may benefit some patients with PD and recurrent, acute pancreatitis associated with accessory papilla stenosis [8] .
Ectopic Pancreas
Ectopic pancreas is pancreatic tissue found outside the usual anatomic confines of the pancreas. Although it may occur throughout the gastrointestinal tract it is most commonly found in the stomach and small intestine. Usually an incidental finding, it may rarely become clinically evident when complicated by inflam-mation, bleeding, obstruction, or malignant transformation [9].
Pancreatic Agenesis
Agenesis of the pancreas is very rare and may be associated with other congenital disease states. In addition, isolated agenesis of the dorsal or, less commonly, the ventral pancreas can occur as silent anomalies [10] .
Congenital Cysts
Congenital cysts of the pancreas are rare and are distinguished from pseudocysts by the presence of an epithelial lining. True congenital cysts occur as a result of developmental anomalies related to the sequestration of primitive pancreatic ducts. They are generally asymptomatic, although abdominal distension, vomiting, jaundice, or pancreatitis can be observed requiring surgical removal.
Anomalous Pancreaticobiliary Ductal Union ( APBDU )
APBDU is a congenital malformation of the confluence of the pancreatic and bile ducts. A classification has been developed for APBDU: if the pancreatic duct appears to join the common bile duct, this is classified as a P–B type. If the common bile duct joins the main pancreatic duct, this is a B–P type. A long common channel is denoted Y type. The frequency of APBDU varies from 1.5 to 3 2%. APBDU is associated with pancreatitis (with long >21 mm and wide > 5 mm common channel), choledochal cysts, and neoplastic abnormalities like cholangiocarcinoma and pancreatic cancer in adults [11] .
Take-home points
Small and large intestine:
- The colon vasculature has two weak points; the splenic flexure and the rectosigmoid junction which are supplied by the narrow terminal branches of SMA and IMA, respectively. These two watershed areas are most vulnerable to ischemia during systemic hypotension.
- The two common congenital anomalies of the abdominal wall presenting at birth are gastrochisis and omphalocele.
- The most common congenital abnormality of the gastrointestinal tract is omphalomesenteric duct, or Meckel diverticulum, which results from the failure of the vitelline duct to obliterate during fetal development.
- The most common enteric nervous system congenital anomaly is Hirschsprung (HSCR) disease, which is characterized by the absence of ganglion cells in the submucosal (Meissner) and myenteric (Auerbach) plexuses along a variable length of the hindgut.
Pancreas:
- Pancreas divisum occurs when the dorsal and ventral ducts fail to fuse; the dorsal duct drains the majority of the pancreas via the minor papilla, while the short ventral duct drains the inferior portion of the head via the major papilla.
References
1 Weber T, Au-Fliegner M, Downard C, Fishman S. Abdominal wall defects . Curr Opin Pediatr 2002; 14: 491–7.
2 Turgeon D , Barnett J . Meckel’s diverticulum . Am J Gastro-enterol 1990; 85: 777–81.
3 Petrokubi R, Baum S, Rohrer G. Cimetidine administration resulting in improved pertechnetate imaging of Meckel’s diverticulum. Clin Nucl Med 1978; 3: 385–8.
4 Skinner M. Hirschsprung’s disease. Curr Probl Surg 1996; 33: 389–460.
5 Kleitsch W . Anatomy of the pancreas; a study with special reference to the duct system . AMA Arch Surg 1955; 71: 795–802.
6 Delhaye M , Engelholm L , Cremer M . Pancrease divisum: congenital anatomic variant or anomaly? Contribution of endoscopic retrograde dorsal pancreatography . Gastroenter-ology 1985; 89: 951–8.
7 Bret P, Reinhold C, Taourel P, et al . Pancreas divisum: evaluation with MR cholangiopancreatography . Radiology 1996; 199: 99–103.
8 Lans J, Geenen J, Johanson J, Hogan W. Endoscopic therapy in patients with pancreas divisum and acute pancreatitis: a prospective, randomized, controlled clinical trial . Gastroin-test Endosc 1992; 38: 430–4.
9 Eisenberger C, Gocht A, Knoefel W, et al. Heterotopic pancreas—clinical presentation and pathology with review of the literature . Hepatogastroenterology 2004; 51: 854–8.
10 Fukuoka K, Ajiki T, Yamamoto M, et al. Complete agenesis of the dorsal pancreas . J Hepatobiliary Pancreat Surg 1999 ; 6: 94–7.
11 Wang H, Wu M, Lin C, et al. Pancreaticobiliary diseases associated with anomalous pancreaticobiliary ductal union . Gastrointest Endosc 1998; 48: 184–9.
CHAPTER 2
Physiology of Weight Regulation
Summary
The interest in the physiology of weight regulation has increased in recent years due to the major deleterious effects of the obesity epidemic on public health. A complex neuroendocrine network involving peripheral organs and the central nervous system is responsible for maintaining a balance between energy intake...
Table of contents
- Cover Page
- Front Page
- Title Page
- Copyright Page
- Contributors
- Preface
- Foreword
- Part 1: Pathobiology of the Intestine and Pancreas
- Part 2: Colonoscopy, Endoscopic Retrograde Cholangiopancreato graphy, and Endoscopic Ultrasound
- Part 3: Other Investigations of the Intestine and Pancreas
- Part 4: Problem-based Approach to Diagnosis and Differential Diagnosis
- Part 5: Diseases of the Small Intestine
- Part 6: Diseases of the Colon and Rectum
- Part 7: Diseases of the Pancreas
- Part 8: Functional Gastrointestinal Disorders
- Part 9: Transplantation
- Part 10: Peritoneal and Other Abdominal Disease
- Index