- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Adult Emergency Medicine at a Glance
About this book
Following the familiar, easy-to-use at a Glance format, and in full-colour, this brand new title provides an accessible introduction and revision aid for medical students and junior doctors. Reflecting the increased profile of Emergency Medicine in clinical practice and the medical school curriculum, Adult Emergency Medicine at a Glance provides a user-friendly overview of the key subjects that will enable any student or junior doctor to 'hit the ground running' when they enter one of the most exciting areas of clinical medicine.
Adult Emergency Medicine at a Glance is:
- A concise, visually orientated course in emergency medicine that is perfect for both study and revision
- Organised around symptoms: 'Short of Breath', rather than diagnoses: 'Pneumonia'
- Focused on the most common or dangerous conditions you will see in the Emergency Department and includes the latest cardiac resuscitation guidelines
- Comprehensively illustrated throughout with over 47 full-page colour illustrations
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Adult Emergency Medicine at a Glance by Thomas Hughes,Jaycen Cruickshank in PDF and/or ePUB format, as well as other popular books in Medicine & Internal Medicine & Diagnosis. We have over one million books available in our catalogue for you to explore.
Information
1
Life in the Emergency Department
This chapter describes the way the Emergency Department operates, and some of the unwritten rules. The prevalence of Emergency Department-based drama generates plenty of misconceptions about what occurs in the Emergency Department. For instance, it is generally inadvisable to say ‘stat’ at the end of one’s sentences, and neither of the authors has been mistaken for George Clooney!
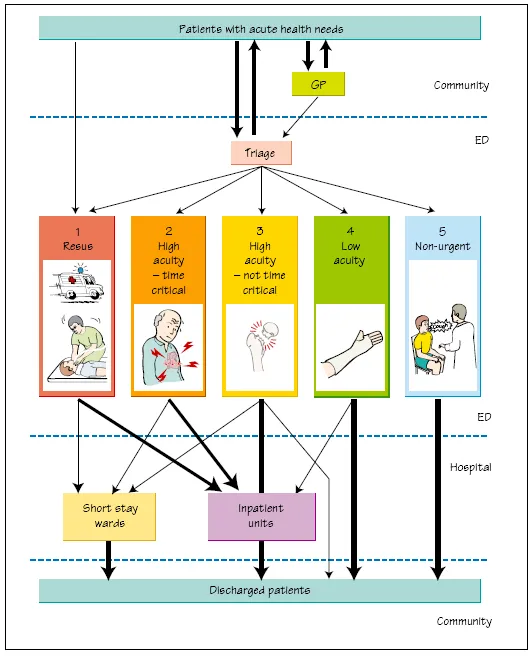
What happens when a patient arrives at the Emergency Department?
Alert phone
Also known as the ‘red phone’ or sometimes ‘the Bat-phone’ , this is the dedicated phone line that the ambulance service uses to prewarn the Emergency Department of incoming patients likely to need resuscitation.
Triage
The concept of triage comes from military medicine – doing the most good for the most people. This ensures the most effective use of limited resources, and that the most unwell patients are seen first.
Nurses rather than doctors are usually used to perform the triage because doctors tend to start treating patients. Systems of rapid assessment and early treatment by senior medical staff can be effective, but risk diverting attention from the most ill patients.
Reception/registration
The reception staff are essential to the function of the Emergency Department: they register patients on the hospital computer system, source old notes and keep an eye on the waiting room. They have to deal with difficult and demanding patients, and are good at spotting the sick or deteriorating patient in the waiting room.
Waiting room
Adult and paediatric patients should have separate waiting rooms, and some sort of entertainment is a good idea. Aggression and dissatisfaction in waiting patients has been largely eliminated in the UK by the 4-hour standard of care: all patients must be seen and discharged from the Emergency Department within 4 hours.
Treatment areas in the Emergency Department
Resuscitation bays
Resuscitation bays are used for critically ill and unstable patients with potentially life-threatening illness. They have advanced monitoring facilities, and plenty of space around the patient for clinical staff to perform procedures. X-rays can be performed within this area.
High acuity area
This is the area where patients who are unwell or injured, but who do not need a resuscitation bay, are managed. Medical conditions and elderly patients with falls are common presentations in this area.
Low acuity area
The ‘walking wounded’ – patients with non-life-threatening wounds and limb injuries – are seen here. Patients with minor illness are discouraged from coming to the Emergency Department, but continue to do so for a variety of reasons.
There is a common misconception that patients in this area are similar to general practice or family medicine patients. Numerous studies have found that there is an admission rate of about 5% and an appreciable mortality in low acuity patients, whereas only about 1% of GP consultations result in immediate hospital admission.
Other areas
Imaging
Imaging, such as X-rays and ultrasound, are integral to Emergency Department function. Larger Emergency Departments have their own CT scanner.
Relatives’ room
When dealing with the relatives of a critically ill patient and breaking bad news, doctors and relatives need a quiet area where information is communicated and digested. This room needs to be close to the resuscitation area.
Observation/short stay ward
This is a ward area close to the Emergency Department, run by Emergency Department staff. This unit treats patients who would otherwise need hospital admission for a short time, to enable them to be fully stabilised and assessed. The function of these units is described in Chapter 28.
Hospital in the home
Some hospitals run a ‘hospital in the home’ programme for patients who do not need to be in hospital but who need certain therapy, e.g. intravenous antibiotics, anticoagulation. The Emergency Department is the natural interface between home and hospital.
Culture of the Emergency Department
There is a much flatter (less hierarchical) organisational structure in the Emergency Department than most other areas in the hospital. This occurs because all levels of medical, nursing and other staff work together all the time, and the department cannot function without their cooperation. Ensuring good teamwork requires good leadership, an atmosphere of mutual respect and a bit of patience and understanding.
The resulting atmosphere can be one of the most enjoyable and satisfying places to work in a hospital. A of this less hierarchical culture that surprises junior doctors is that nurses will question their decisions; this is a sign of a healthy culture in which errors are less likely to occur, and is actively encouraged.
Emergency Department rules
Being a doctor in the Emergency Department is different from elsewhere in the hospital. There is nowhere to hide and, for the first time in most medical careers, you are responsible for making the decisions. On the positive side, there are plenty of people around to help you, who have all been through the same process.
Some basic advice:
- Write legible, timed, dated notes.
- Show respect for other professional groups and be prepared to learn from them.
- Do not be late for your shifts; do not call in sick less than 6 hours before a shift.
- Patients who re-present are high risk and need senior review.
- Take your breaks. You need them.
- Keep calm.
- If in doubt, ask.
- Do not pick up so many patients that you cannot keep track of them.
- Do not avoid work or avoid seeing difficult patients. We do notice.
- The nurse in charge is usually right.
With so many people working closely together in a stressful atmosphere, it is inevitable that conflicts will occur. Do not let them fester; some ground rules for resolving such conflicts are:
- Resolve it now.
- Do it in private.
- Do it face to face.
- Focus on facts.
- Criticise action, not person.
- Agree why it is important.
- Agree on a remedy.
- Finish on a positive.
2
Diagnosis
The Emergency Department is a diagnosis machine, taking people with a wide variety of symptoms, labelling them with a diagnosis, treating and then discharging them whenever safe to do so. There are plenty of opportunities for this process to go wrong, and it is important to understand how this can occur.
‘If you listen carefully to the patient, they will tell you the diagnosis’ . W Osler
Despite a couple of thousand years of medical education, we are still not really sure how the diagnostic process works.
- Some people work forward from history, examination and a shortlist of differential diagnoses.
- Others work backwards from a list of likely diagnoses to weight these according to symptoms and examination.
- Experts make their diagnoses by pattern recognition.
It may be that expertise occurs with the development of cognitive flexibility to use multiple diagnostic strategies to integrate and test the result.
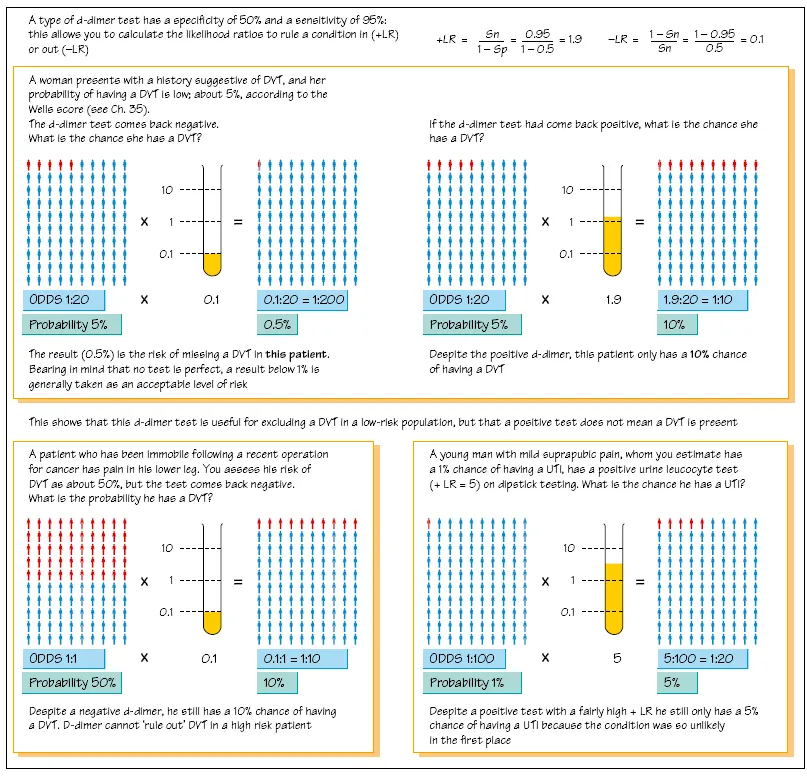
Using tests
In the past, the Emergency Department used a few simple tests to inform decision-making. An X-ray of an injured limb has a binary outcome: broken/not broken. As technology and the scope of Emergency Medicine has increased, the tests have become more numerous and less black and white, and there is a need to rationalise and manage the uncertainty generated.
The most common way of describing a test’s performance is to use sensitivity and specificity.
Confusion matrix
| Actual patient status (truth) | ||
| Test result | Disease present | Disease absent |
| Positive | True positive (A) | False positive (B) |
| Negative | False negative (C) | True negative (D) |
| Total no. patients | With disorder (A + C) | Without disorder (B + D) |
| Sensitivity = A/(A + C) and Specificity = D/(B + D) | ||
For example, if a very specific test, e.g. Troponin I, is positive, we know that myocardial damage has occurred, because the number of false positives (B) is very low. Similarly, if a very sensitive test, e.g. CT scan for abdominal aortic aneurysm (AAA), comes back as negative, we know that it is very unlikely that the patient has an AAA as the number of false negatives (C) will be very low.
SpIN – a very Specific test rules a condition IN .
SnOUT – a very Sensitive test rules a condition OUT .
However, Emergency Departments use many tests that are not 100% sensitive or specific, and therefore a more powerful, but less intuitive, model is necessary to understand these tests: likelihood ratios, which are calculated from the specificity and sensitivity.
Treatment orders
Once the likely diagnosis has been made, a set of treatment orders needs to be decided and documented. A good acronym for this is DAVID, e.g., for an elderly patient with an open fracture of the tibia:
- Diet – nil by mouth
- Activities – elevate limb
- Vital signs monitoring – hourly limb observations
- Investigations – CXR, FBC, U + E
- Drugs/treatment – immediate i.v. antibiotics
Bayes’ theorem
The chance of something being true or false depends not only on the quality of the test that one is performing, but importantly, how likely the event is in the first place.
Thomas Bayes, an eighteenth-century English priest, deduced the principles that underpin the way we use tests in medicine:
pre-test probability x likelihood ratio = post-test probability
To calculate this, we use odds (like horse racing odds) rather than probability, but the two are obviously very closely related.
The likelihood ratio is calculated from the test’s sensitivity (Sn) and specificity (Sp) and is a much better measure of a test’s clinical usefulness in ruling a disease in (positive LR) or out (negative LR).

How do I define pre-test probability?
The triage process uses an expert nurse to assess clinical status and is an assessment of the probability of serious illness. The fact that a patient has arrived at the Emergency Department at all, rather than going to their own doctor, automatically means the probability of significant disease is relatively high.
Clinical decision rules are widespread in Emergency Medicine and help codify knowledge and explicitly define pretest probability. However, unthinking application of such decision-support tools by clinicians without an appreciation of their flaws and limitations results in bad decisions and/or over-investigation.
A history and examination taken by an experienced clinician remains a very good predictor of pre-test probability of disease. As can be seen opposite, a test applied in an inappropriate population group, i.e. with a pre-test probability that is very high or very low, will give misleading results...
Table of contents
- Cover
- Table of Contents
- Preface
- 1 Life in the Emergency Department
- 2 Diagnosis
- 3 Shock and intravenous fluids
- 4 Imaging in the Emergency Department
- 5 Analgesia
- 6 Airway management and sedation
- 7 Blood gas analysis
- 8 Trauma: primary survey
- 9 Trauma: secondary survey
- 10 Major head and neck injury
- 11 Minor head and neck injury
- 12 Wounds
- 13 Burns
- 14 Hand injuries
- 15 Wrist and forearm injuries
- 16 Shoulder and elbow injuries
- 17 Back pain, hip and knee injuries
- 18 Tibia, ankle and foot injuries
- 19 Abdominal pain
- 20 Urology problems
- 21 Ear, nose, throat and dental problems
- 22 Eye problems
- 23 Obstetrics and gynaecology problems
- 24 Toxicology: general principles
- 25 Toxicology: specificpoisons
- 26 Psychiatry: self-harm and capacity
- 27 Psychiatry: the disturbed patient
- 28 Observational medicine
- 29 Loss of function and independence
- 30 Syncope, collapse and falls
- 31 Slow heart rate
- 32 Fast heart rate
- 33 Cardiac arrest
- 34 Chest pain: cardiovascular
- 35 Chest pain: non-cardiovascular
- 36 Shortness of breath
- 37 Anaphylaxis
- 38 Sepsis
- 39 Endocrine emergencies
- 40 Gastroenterology
- 41 Headache
- 42 Stroke and transient ischaemic attack
- 43 Seizures
- 44 Hypothermia and hyperthermia
- 45 Pre-hospital medicine
- 46 Major incident
- 47 Chemical, biological, radiation, nuclear and explosive incidents
- Case studies: questions
- Case studies: answers
- Index
- End User License Agreement