eBook - ePub
Medical Care of the Liver Transplant Patient
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Medical Care of the Liver Transplant Patient
About this book
This book builds on the success of previous editions, once again providing hepatologists the most current clinical guide on how to best treat the liver transplant recipient. With an international mix of experienced contributors, this new edition highlights initial indication and selection of the potential recipient, management of the donor organ, post-operative complications in the patient through to acute recovery, long-term follow-up, and continued health. This provides the user a complete guide to the correct clinical management of both the recipient and the donor organ through all stages of transplantation.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Medical Care of the Liver Transplant Patient by Pierre-Alain Clavien, James F. Trotter, Pierre-Alain Clavien,James F. Trotter in PDF and/or ePUB format, as well as other popular books in Medicine & Gastroenterology & Hepatology. We have over one million books available in our catalogue for you to explore.
Information
PART ONE: Management of the Potential Transplant Recipient
1
Selection and evaluation of the recipient (including retransplantation)
Key Learning Points
- Patients should be considered for liver transplantation if they have evidence of life-threatening complications of liver disease including cirrhosis and acute liver failure.
- Indications and contraindications perpetually change with regard to an organ shortage and medical improvements.
- Prioritization for transplantation is now determined by the Model of End Stage Liver Disease (MELD), which lists patients with the greatest risk of short-term mortality.
- At the liver center, a detailed evaluation of the recipient is performed to ensure that transplantation is indicated and feasible.
- Despite a high mortality comparing primary liver transplantation, retransplantation is the only therapy suitable for patients with loss of graft function.
Introduction
Selection and evaluation of a recipient for liver transplantation (LT) has become a great challenge, in the best interest of both the patient and society. Actually, limited organ availability and an increasing demand for organ transplantation has extended transplant waiting times and thus increased morbidity and mortality for potential recipients on waiting lists.
Patients should be referred to transplant centers when a life-threatening complication of liver disease occurs. A detailed medical evaluation is performed to ensure the feasibility of LT. Priority for transplantation has been determined by the MELD score, identifying patients with the highest estimated short-term mortality.
Selection of the Recipient: Why Liver Transplantation Should Be Performed
Selection of the recipient is a main challenge for transplant physicians. LT is indicated in end-stage liver disease (ESLD). The most common indication in the adult is cirrhosis but the list of indications is growing. In contrast, the transplant community is currently faced with a major organ shortage; this has put extraordinary pressure on organ allocation programs. Since a successful outcome requires optimal patient selection and timing, the issue of which patients to list for LT and when to transplant cirrhotic patients has generated great interest as well as considerable controversy.
Main Indications for LT: Complications of ESLD
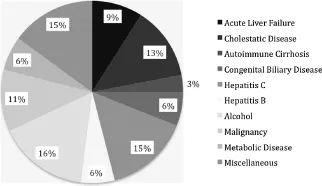
LT should be considered in any patient with liver disease in whom the procedure would extend life expectancy beyond what the natural history of underlying liver disease would predict or in whom LT is likely to improve quality of life. Patients should be selected if expected survival in the absence of transplantation is 1 year or less, or if the patient has an unacceptable quality of life because of liver disease. Indications for LT in Europe are summarized in Figure 1.1.
Figure 1.1 Indications for liver transplantation in Europe38
Gastroesophageal Variceal Bleeding
Gastroesophageal varices are found in 30% of patients with compensated cirrhosis and 60% of patients with decompensated cirrhosis. Variceal bleeding usually does not occur until the Hepatic Venous Pression Gradient (HVPG) is above 12 mmHg. Each episode of bleeding carries a 20% mortality rate. If the varices are left untreated, after survival from the first episode, the rebleeding risk can be up to 70% within 1 year and is a major cause of death in patients with cirrhosis. Medical treatments are endoscopic variceal ligation and nonselective beta-blockers. Transjugular intrahepatic portosystemic shunt (TIPS) involves establishment of a direct pathway between the hepatic veins and the portal veins to decompress the portal venous hypertension that is the source of the patient’s hemorrhage. The procedure is technically challenging, especially in critically ill patients, and has a mortality rate of 30–50% in the emergency setting, but has <90% effectiveness in controlling bleeding from gastroesophageal varices. LT remains the best way to decompress the portal system if other therapy has failed.1
Hepatic Encephalopathy
Hepatic encephalopathy (HE) is a neuropsychiatric complication of cirrhosis in which clinical manifestations range from subtle personality changes and sleep disorder to coma. Although treatments have emerged, such as rifaximin to improve recurrence of HE,2 LT remains the only effective therapy.
Ascites and Hepatorenal Syndrome
Refractory ascites occurs in 5–10% of cirrhotic patients and carries a mortality rate of >50% at 2 years. Patients are prone to develop gastrointestinal variceal bleeding, hepatorenal syndrome (HRS), spontaneous bacterial peritonitis (SBP) and HRS approximately 1 year after the development of ascites, reflecting the poor prognosis of patients with ascites. LT evaluation therefore should be instituted whenever refractory ascites develop.3
HRS is characterized by renal vasoconstriction in response to renal hypoperfusion from a low systemic effective circulating volume. The annual incidence of HRS in patients with cirrhosis and ascites is approximately 8%.4 Two types of HRS are described. Type 1 HRS is characterized by a rapidly progressive impairment of the circulatory and renal functions associated with a very poor prognosis (median survival rate <2 weeks). Type 2 HRS is characterized by a steady impairment of the circulatory and renal function with a median survival rate of 6 months. LT should be considered as soon as a HRS is diagnosed.
Pulmonary Complications
Hepatopulmonary syndrome (HPS) is found in 4–47% of patients with cirrhosis and is characterized by intrapulmonary vascular dilatations, especially in the basal parts of the lung. Liver injury and/or portal hypertension trigger the release of endothelin-l, TNF-alpha, cytokines and mediate vascular shear stress and release of nitric oxide and carbon monoxide, all contributing to intrapulmonary vasodilatation. This results in hypoxemia which may require oxygen therapy. Because it could reverse HPS, LT is the only curative treatment. HPS differs from portopulmonary hypertension (PPHTN) which occurs in 2–8% of patients with cirrhosis. Imbalance between vasodilating and vasoconstrictive agents may be responsible for misguided angiogenesis and pulmonary hypertension. It is associated with a higher risk for LT and increased post-transplantation mortality.
Specific Indications for LT
Some indications for LT are specific and vary depending on the underlying liver disease.
Cholestatic Diseases
Some criteria for primary biliary cirrhosis (PBC) are specific (see Chapter 10). As survival rate is considerably reduced when the bilirubin level is over 100 µmol/L for <1 year, this level is an indication of LT without any other complication. Uncontrolled and intolerable pruritus or major asthenia, even if isolated, are also indications for LT.
Primary sclerosing cholangitis (PSC) is a rare idiopathic cholestatic disease of unknown cause, characterized by a chronic fibrosing inflammation of the bile ducts (see Chapter 10). There is also an increased risk of cholangiocarcinoma, which is a difficult diagnosis with a prevalence over 30% after a 10-year disease course.5 Specific indications for PSC are longstanding severe jaundice (bilirubin level over 100 µmol/L), cholestasis and pruritus not related to an acute episode of cholangitis, repeated episodes of cholangitis not controlled by antibiotics, and any suspicion of cholangiocarcinoma.
Autoimmune Chronic Hepatitis
Autoimmune chronic hepatitis is more common in young women. The clinical presentation of the disease is variable; classically it presents as active chronic hepatitis, but it may also present as established cirrhosis and in few cases as a fulminant course without chronic hepatic disease. A main characteristic of this disease is a good response to immunosuppressive treatment including steroids.6
LT is indicated in autoimmune hepatitis for clinical decompensation, despite long-term adequate immunosuppressive treatment, or in fulminant hepatic failure, in which immunosuppressive treatment is usually ineffective and potentially deleterious.
Viral Hepatitis
Chronic viral hepatitis due to the hepatitis virus B, C and/or D is one of the most common causes of ESLD worldwide and a frequent diagnosis in patients referred to transplant centers. Viral recurrence after LT is a major issue and graft damage secondary to viral re-infection may lead to graft failure, retransplantation or death.
Alcoholic Liver Disease
Alcoholic cirrhosis is a common liver disease and a significant number of patients with alcoholic liver disease receive LT. Several centers have developed an evaluation process based on medical and psychiatric criteria to better determine patients who would benefit most from the procedure. Abstinence from alcohol of at least 6 months is usually required to evaluate the need and timing of LT and to obtain better control of alcoholism. This interval is neither a consensus nor an absolute requirement. The risk of recidivism is estimated to be between 15–40% depending on the series, which seems to be related to the duration of follow up after LT and the duration of abstinence before transplantation. Whichever the case, this remains controversial.7
Acute alcoholic hepatitis has been considered an absolute contraindication to liver transplantation on the grounds that patients with this disorder have been drinking recently and that a period of abstinence will allow many to recover. Unfortunately, many patients die during this interval. Patients who do not recover within the first 3 months of abstinence are unlikely to survive.8 Consequently, liver transplantation centers face a dilemma when caring for a patient with alcoholism who has severe alcoholic hepatitis and whose condition deteriorates despite adherence to abstinence, nutritional support, corticosteroids, and other elements of medical management.9
Hepatobiliary Malignancy
In certain cases, hepatobiliary malignancy is an indication for LT.
Hepatocellular carcinoma (HCC) is the commonest primary malignancy of the liver. LT is a suitable therapeutic option for early, unresectable HCC, particularly in the setting of chronic liver disease. The study by Mazzaferro in 1996 established LT as a viable treatment for HCC.10 In this study, the “Milan criteria” were applied, achieving a 4-year survival rate similar to LT for benign disease. Since then various groups have attempted to expand these criteria11 (see Chapter 11).
Cholangiocarcinoma (CCA) is the second most common cancer among the primary hepatic neoplasm, accounting for 5–20% of liver malignancies.12 LT for CCA remains a controversial subject (see Chapter 12). A protocol combining neoadjuvant chemoradiation and LT was first used in patients with unresectable hilar CCA. Results have confirmed that this approach leads to significantly lower recurrence rates and higher long-term survival rates than other existing treatment modalities. Despite this, protocols to treat patients with CCA are not widespread, and are available at only a handful of transplant programs.
Other hepatobiliary malignancies may be successfully treated by LT, including without fibrolamellar carcinoma (without metastases), and hemangioendothelioma.
Classically, metastatic tumors of the liver have been considered a poor indication for LT, although some centers have performed this procedure associated with another therapy, such as chemotherapy and radiotherapy. In metastases from neuroendocrine tumors, liver transplantation could be indicated for patients with symptoms related to major hepatomegaly, hormone production, inavailability of effective therapeutic alternatives, diffuse metastases of the liver, slow-growing tumor and absence of extrahepatic disease.13 Transplant offers the main advantage of a significant improvement of the quality of life in many patients, an alternative to palliative therapy and a possible cure in some patients.
Non-Alcoholic Fatty Liver Disease and Non-Alcoholic SteatoHepatitis
In the setting of the metabolic or insulin resistance syndrome (IRS), non-alcoholic fatt...
Table of contents
- Cover
- Title page
- Copyright page
- Contributors
- Preface
- PART ONE: Management of the Potential Transplant Recipient
- PART TWO: Donor Issues and Management in the Perioperative Period
- PART THREE: Chronic Problems in the Transplant Recipient
- PART FOUR: Pediatric Liver Transplantation
- Multiple choice questions
- Answers
- Index