eBook - ePub
Hyperandrogenism in Women
Beyond Polycystic Ovary Syndrome
- 192 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Hyperandrogenism in Women
Beyond Polycystic Ovary Syndrome
About this book
Hyperandrogenism profoundly affects women's lives from lowering self-esteem to changing cognition and affective motivation. The polycystic ovary syndrome (PCOS) is the most common androgen excess disorder worldwide. While it is not the focus of this book, some aspects are discussed. The aim of this book is to improve understanding of androgen excess and its impact on several conditions. Topics include development of adipose tissue in females, insulin sensitivity, congenital adrenal hyperplasia, and Cushing's disease/syndrome. There is also a discussion of PCOS with emphasis on in utero origins and specific genetic and epigenetic factors. This book provides a wealth of relevant information for every endocrinologist and gynecologist who wants to broaden their knowledge of androgens in various conditions.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Hyperandrogenism in Women by R. Pasquali,D. Pignatelli,Renato Pasquali,Duarte Pignatelli,Renato, Pasquali,Duarte, Pignatelli, Federica Guaraldi,Giovanni Corona,Federica, Guaraldi,Giovanni, Corona in PDF and/or ePUB format, as well as other popular books in Medicine & Endocrinology & Metabolism. We have over one million books available in our catalogue for you to explore.
Information
Pasquali R, Pignatelli D (eds): Hyperandrogenism in Women. Beyond Polycystic Ovary Syndrome.
Front Horm Res. Basel, Karger, 2019, vol 53, pp 135–161 (DOI: 10.1159/000494909)
Front Horm Res. Basel, Karger, 2019, vol 53, pp 135–161 (DOI: 10.1159/000494909)
______________________
Androgens in Menopausal Women: Not Only Polycystic Ovary Syndrome
Ervin K. Kostakisa Lisonia N. Gkionia Djuro Macutb George Mastorakosa
aUnit of Endocrinology, Diabetes Mellitus and Metabolism, Aretaieion Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece; bClinic of Endocrinology, Diabetes and Metabolic Diseases, University of Belgrade, Belgrade, Serbia
______________________
Abstract
Menopause is the period of a woman’s life that is characterized by the permanent cessation of menses associated to hormonal changes, of which the most important is the decrease of estrogen levels. Following menopause, the concentrations of circulating androgens decrease. However, increased concentrations of luteinizing hormone induce androgens secretion from the ovaries and presumably from the adrenal glands. Peripheral conversion of androgens results to the circulating hormonal androgen profile. Some pathological conditions are associated with greater concentrations of androgens after menopause than in controls, with polycystic ovary syndrome (PCOS) being the commonest. These conditions can be distinguished in non-tumorous (adrenal or ovarian) or functional and tumorous (adrenal or ovarian benign or malignant) masses. Apart from PCOS, other non-tumorous (adrenal or ovarian) causes of hyperandrogenism in post-menopausal women are obesity, non-classic congenital adrenal hyperplasia (NCCAH), endocrinopathies, such as Cushing disease or acromegaly; ovarian hyperthecosis, drug use or abuse. Tumorous (adrenal or ovarian) causes include adrenal cortical cancers, adrenal benign adenomas and even incidentalomas, or ovarian tumors such as the sex-cord stromal ovarian tumors and metastases in the ovary. The diagnosis of hyperandrogenism is made through medical history, clinical examination, and laboratory tests. Total testosterone concentration of 150 ng/dL can be used at first to distinguish a malignant from a benign cause of hyperandrogenism. Dehydroepiandrosterone sulfate concentration may support adrenal source of androgens. Imaging techniques are used to localize the source of androgens: computed tomography and magnetic resonance imaging (MRI) for the adrenals and transvaginal ultrasound or MRI for the ovaries. Finally, treatment (etiologic and symptomatic) and long-term effects of hyperandrogenism are developed in this chapter.
© 2019 S. Karger AG, Basel
Introduction
Menopause is the period of a woman’s life that is characterized by the permanent cessation of menses due to the lowering of concentrations of ovarian estradiol below a certain threshold. This physiological phenomenon reflects a decrease in the number of oocytes in the ovaries and it is associated with the permanent cessation of ovulation. During the post-menopause period, the amount of androgens secreted by the ovary decreases gradually. In fact, the concentrations of circulating testosterone (T), as well as of androgen precursors, decrease with aging in post-menopausal women, even though transient increases have been reported, mostly during menopausal transition. This has been shown in the Study of Women’s Health Across the Nation, which focuses mainly on dehydroepiandrosterone (DHEA) sulfate, an androgen predominantly of adrenal origin [1].
Hyperandrogenism is a clinical syndrome that accompanies various pathologic conditions encountered in girls and women [2]. In menopause, it expresses relative or absolute excess of circulating androgenic hormones (androgens) of adrenal or ovarian origin and it is characterized by dermatologic stigmata, such as acne, oily skin, seborrhea and skin inflammation, hidradenitis suppurativa, dystopic increase in terminal hair growth (hirsutism) or loss of hair (alopecia), virilization, as well as adverse metabolic phenomena. The latter are more intense when associated to insulin resistance. In some cases, although the circulating concentrations of androgens are found within normalcy, the increased sensitivity of androgen receptor at the hair follicle might result in idiopathic hirsutism [2].
Polycystic ovary syndrome (PCOS)-related hyperandrogenism is the most frequently encountered condition during the fertile life of women. It persists after menopause, still representing the most frequent cause of hyperandrogenism [3]. It often manifests in puberty and is characterized by specific clinical, biochemical and morphological criteria [4]. During menopause, circulating androgens decrease in women diagnosed with PCOS before menopause, although remaining greater than those of non-PCOS post-menopausal women (at least during the early post-menopausal years) [5]. Apparently stromal and thecal androgen production in post-menopausal PCOS women might still be responsive to the increased concentrations of luteinizing hormone (LH) for some time [6]. Other causes of hyperandrogenism in post-menopausal women can be of non-tumorous (functional) or of tumorous adrenal or ovarian origin (adenomas and carcinomas). The non-tumorous causes include obesity, which is associated with insulin resistance-linked conditions, endocrinopathies (Cushing disease, acromegaly, hyperprolactinemia, and hyperthyroidism), as well as pharmaceutical use- or abuse-associated conditions; while the tumorous are related to tumors, mainly of adrenal or ovarian origin [5].
This chapter will present the causes of hyperandrogenism (beyond PCOS) in post-menopausal women. The traditional didactic approach is followed, including physiology, presentation of clinical characteristics, causal pathophysiology (etiology) and diagnosis, and suggested methods of management and treatment. An algorithm of diagnosis is proposed.
Menopause and Staging of Menopause
Menopause marks the permanent end of fertility in women. Diagnosis is based on the absence of menstruation for at least 12 consecutive months. The average age of menopause is around 51 years depending on various factors, which include geographic area and lifestyle. The influence of genetic and environmental factors on menopause age is still under investigation. Earlier menopause is observed in women living in developing countries (e.g., Indonesia, Pakistan, and Chile) and in women living in rural areas compared to those living in developed countries [7–10]. Also, women living at higher altitudes experience earlier menopause [11, 12]. Smoking is associated with earlier menopause (1–2 years earlier) compared to the non-smoking habit [13, 14]. After menopause, an average life expectancy longer than 30 years is estimated for women in developed countries [15, 16].
The Stages of Reproductive Aging Workshop (STRAW) criteria of 2001, categorized, for the first time, the life of woman in 3 phases: reproductive, menopausal transition and post-menopause. These criteria were revised in September 2011, during the Annual Meeting of North American Menopause Society and they were renamed STRAW +10 [17]. The criteria in this system mostly depend on the characteristics of the menstrual cycle, as a key indicator of ovarian age. Nevertheless, the hormonal criteria of ovarian aging, such as elevated follicle-stimulating hormone (FSH), low anti-Müllerian hormone (AMH), and inhibin B concentrations are also taken into consideration (Fig. 1) [17]. Menstrual cyclicity and circulating concentrations of early follicular phase FSH were employed as primary determinants of this categorization. Stages –2 and –1 refer to early and late menopausal transition; stages +1 (+1a, +1b, +1c) and +2 refer to early and late post-menopause. Stages –2, –1, and +1a include a period defined also as peri-menopause. The increased variability in menstrual cycle duration (over 7 days) is persistent in women with elevated FSH concentrations, low AMH concentrations and low antral follicle count. The term “persistence” denotes the repeated occurrence (during 10 cycles starting from the first cycle) of variable cycle duration. Although duration of stage –1 differs among women, it generally lasts 1–3 years and is characterized by vasomotor symptoms and intervals of amenorrhea of 60 days or longer (Fig. 1). Concentrations of FSH greater than 25 IU/L in a random blood sample denote late menopausal transition. The menopausal transition ends with the final menstrual period (stage 0), which is recognized after 12 months of amenorrhea and corresponds to the end of stage +1a and peri-menopause. FSH continues to increase, as estradiol continues to decrease for approximately 2 years, in the end of stage +1b. The period of stabilization of high FSH and low estradiol represents stage +1c and it lasts approximately 3–6 years. In total, early post-menopause lasts approximately 5–8 years [17]. The criteria of STRAW +10 are applicable in most women, irrespective of age, body mass index (BMI), demographic characteristics or lifestyle, while age is not used as a criterion. They are not easily applicable in some cases such as premature ovarian insufficiency or PCOS, for which amenorrhea is part of the pathologic manifestations [17].
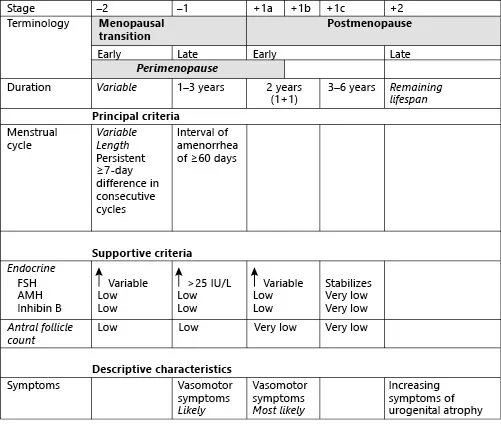
Fig. 1. Schematic representation of the stages from menopausal transition to post-menopause according to the Stages of Reproductive Aging Workshop +10 staging system for reproductive aging in women (modified from [17]).
Physiology of Androgen Production in Menopause
Major Androgens in Menopause
The major androgens found in circulation are T, androstenedione (A4), DHEA and their sulfated forms, DHEA sulfate (DHEAS). They are produced from the ovaries, the adrenals and peripheral tissues (hair follicles, sebaceous glands, external genitalia; Fig. 2).
Testosterone: During the reproductive life of a woman, T is derived approximately at equal quantities from adrenals and ovaries. These glands contribute about 50% of the plasma T concentration, with the remaining 50% coming from peripheral conversion of androgen precursors produced again at equal quantities from the adrenals and the ovaries (Fig. 2) [18]. Total T concentrations decline with aging showing a 50% decrease and loss of mid-cycle peak in pre-menopausal women compared to 21-year-old women. At post-menopause T concentrations decrease by 15% [19, 20]. Certain studies did not find changes of T concentrations during menopausal transition. Although T concentrations decrease at post-menopause, a state of relative hyperandrogenism is expressed clinically, due to the marked decline of estrogen concentrations at the same time [21].
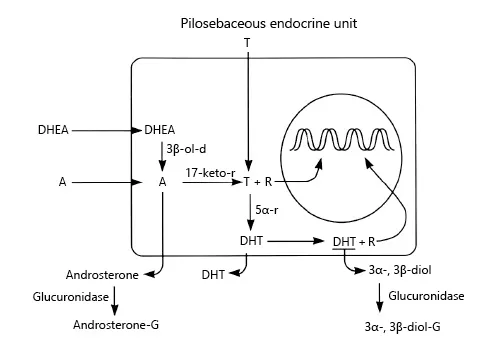
Fig. 2. Pilosebaceous endocrine unit. DHEA, dehydroepiandrosterone; A, androstenedione; T, testosterone; R, androgen receptor; DHT, dihydrotestosterone; 3α- and 3β-diol, alpha- and be...
Table of contents
- Cover Page
- Front Matter
- In utero Androgen Excess: A Developmental Commonality Preceding Polycystic Ovary Syndrome?
- Androgens, Body Composition, and Their Metabolism Based on Sex
- Understanding the Role of Androgen Action in Female Adipose Tissue
- The Role of Androgen Excess on Insulin Sensitivity in Women
- Androgens in Congenital Adrenal Hyperplasia
- Androgens in Cushing’s Syndrome
- Hyperandrogenism and Adrenocortical Tumors
- Androgen-Secreting Ovarian Tumors
- Endocrinology of Hirsutism: From Androgens to Androgen Excess Disorders
- Obesity and Androgens in Women
- Androgens in Menopausal Women: Not Only Polycystic Ovary Syndrome
- Androgen Excess in Women: Proteomic and Metabolomic Approaches
- Androgens and Severe Insulin Resistance States: Basic and Clinical Aspects
- Author Index
- Subject Index
- Back Cover Page