![]()
Section 1
Medical terminology
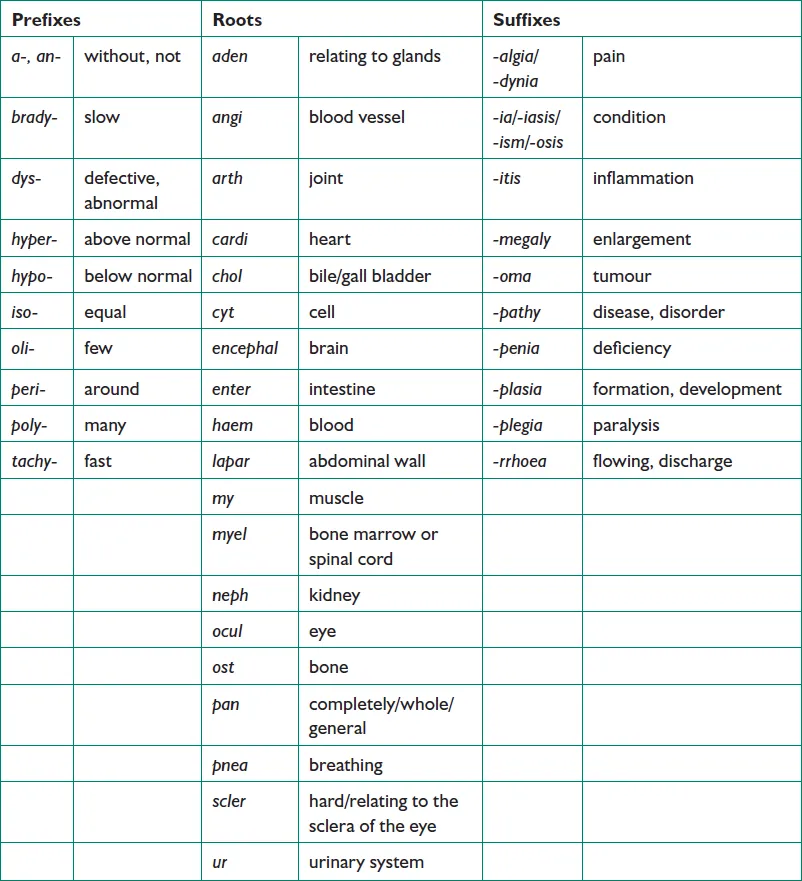
In order to interpret a patient’s medical notes accurately and with confidence, it is essential to have a good grasp of medical terminology. Some of the terms that are commonly encountered may appear to be very long and complicated but they are generally built up from smaller ‘building blocks’. Once the longer terms have been broken down into their constituent blocks, the meaning becomes much clearer.
Medical terms have three basic components: the root, which forms the basis of the word; a prefix – any syllables added in front of the root to modify it and a suffix – any syllables added after the root to modify it. Knowledge of the meanings of a few common roots, prefixes and suffixes enables the understanding of the majority of commonly encountered medical terms.
For example:
| (PSEUDO) |
(HYPO ) |
(PARA) |
(THYROID) |
(ISM) |
| (false) |
(under) |
(beside) |
(thyroid) |
(condition) |
i.e. a condition resembling underactivity of the parathyroid glands.
Tables 1.1 and 1.2, on page 2, contain some of the common roots, prefixes and suffixes that are encountered in clinical practice.
Table 1.1: Common medical prefixes, suffixes and roots
Table 1.2: Common surgical suffixes
| -centesis |
surgical puncture (used for aspiration) |
| -desis |
binding |
| -ectomy |
excision or removal of a body part |
| -plasty |
repair, reconstruction |
| -rrhapy |
surgical suturing |
| -scopy |
use of a viewing instrument |
| -stomy |
creation of an opening |
| -tomy |
the act of cutting, making an incision |
![]()
Section 2
Patient medical notes
To be involved effectively in the clinical decision-making process, it is important to be able to understand and utilise the information to be found in the patient medical notes. On occasions it is also necessary for the pharmacist to record their interventions in a patient’s medical notes.
The medical notes are a chronological record of all significant aspects, including drug treatment, of a patient’s care. These are completed for both inpatient stays and for outpatient clinic visits. As a clinical pharmacist you will frequently intervene directly in the care of patients to ensure the safety and efficacy of their treatment. If you do need to intervene in a patient’s drug treatment, there are a number of ways in which you can convey this information to the prescriber(s) concerned.
Face to face with the prescriber
This is much the best way to deal with any concerns you have. The modifications you wish to recommend to the prescriber can be discussed and you will all have the information you require to hand. The prescriber is unlikely to document your intervention in the patient’s medical notes.
Bleeping or phoning the doctor
If the prescriber is not available for a face to face discussion and the intervention you wish to make is urgent, this is the method used for contacting the prescriber. However, it may not be a convenient time for the prescriber to talk to you. Again, it is unlikely that the prescriber will document your intervention in the patient’s medical notes.
Leaving a note on the prescription
This is often used as a method of communication in the hospital environment, particularly if the prescriber is a surgeon, is in theatre and cannot be disturbed. However, such notes are easily lost and if your intervention is not addressed by the prescriber it is difficult to say whether the prescriber saw your note and chose to ignore it, or whether your note was seen at all. Again there is no permanent record of your intervention.
Leaving a message with another member of staff
Your message may not be passed on correctly, if at all. Again there is no permanent record of your intervention.
The following are examples of when you, as a clinical pharmacist, should document your interventions in a patient’s medical notes:
•When you recommend that a drug is initiated or discontinued
•When you have discovered that an adverse drug reaction has occurred
•When you discover that the patient is not, or has not been, compliant with their medication
•When your input has been requested by the medical team
•When a critical change to a dosage regimen has occurred
•When an important recommendation has not been followed
•When your written communication would facilitate a review of the patient’s drug treatment.
General Layout
The way in which patient medical notes are arranged varies from Trust to Trust. However, the following sections are usually present; it is the order in which they are presented that differs.
Inpatient admissions
The current admission may be found to the front or to the back of this section. All admission notes will contain the same information and previous admissions may be useful for obtaining certain information such as previous drug history (which may not be accurate!).
The current admission usually contains the following information: case history, systems enquiry and examination, differential diagnoses/provisional diagnosis, investigations, drug history, progress.
Outpatient notes
These are often less precise than a full admission, usually consisting of the specific problem, progress since last visit, any relevant measurements and test results, and drug therapy.
Investigations
This section contains, if printed, the clinical chemistry, haematology and microbiology reports, along with the results of X-rays, scans, biopsies, etc. Investigations may not always be recorded in the notes, but available electronically elsewhere.
Letters
Discharge, clinic and referral (from GPs and other consultants) letters will be included.
Other information
This will include copies of previous discharge prescriptions, drug treatment sheets, and nursing notes.
Breakdown of Medical Notes
Case history
The case history is the information obtained from the patient on admission. The process is known as ‘clerking’ and is usually performed by the on-call doctor (either the Foundation Year 1 (FY1) doctor or the Foundation Year 2 (FY2) doctor) or in some places in pre-admission clinics. A patient may be admitted to hospital via several routes, the most common being: elective (i.e. a planned, booked admission), acute via Accident and Emergency, acute via GP referral or acute self-referral.
Presenting complaint (PC)
These are the main symptoms that have led to the referral and admission to hospital. The PC may also be referred to as ‘CC’ (chief complaint) or ‘C/O’ (complains of).
History of presenting complaint (HPC)
This consists of the symptoms experienced in the recent past leading up to the referral, usually with reference to the presenting complaint, as...