eBook - ePub
Molecular Medicine for Clinicians
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Molecular Medicine for Clinicians
About this book
The insights following the wake of the Human Genome project are radically influencing our understanding of the molecular basis of life, health and disease. The improved accuracy and precision of clinical diagnostics is also beginning to have an impact on therapeutics in a fundamental way. This book is suitable for undergraduate medical students, as part of their basic sciences training, but is also relevant to interested under- and postgraduate science and engineering students. It serves as an introductory text for medical registrars in virtually all specialties, and is also of value to the General Practitioner wishing to keep up to date, especially in view of the growing, internet-assisted public knowledge of the field. There is a special focus on the application of molecular medicine in Africa and in developing countries elsewhere.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Molecular Medicine for Clinicians by Patrick Arbuthnot,Silke Arndt,Sahle Asfaha,Jacqueline Brown,Alexio Capovilla,Arnold Christianson,Gerrit Coetzee,Theresa Coetzer,Leandra Cronjé,Nigel Crowther,Chrisna Durandt,Adriano Duse,Lindsay Earlam,Debbie Glencross,Nerine Gregersen,Kate Hammond,Tabitha Haw,Nicole Holland,Penny Keene,Hendrik Koor, Barry Mendelow,Michèle Ramsay,Nanthakumarn Chetty,Wendy Stevens, Barry Mendelow, Michèle Ramsay, Nanthakumarn Chetty, Wendy Stevens in PDF and/or ePUB format, as well as other popular books in Biological Sciences & Genetics & Genomics. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
Introduction
Barry V Mendelow and Penny Keene
The explosion of public interest in the human genome, coupled with the revolution in information technology and widespread access to knowledge made possible by modern communication technologies, has created a public that is increasingly demanding that their medical professionals are experts in the diagnostic and therapeutic implications of applied molecular medicine. Moreover, the rampant march of HIV/AIDS, itself a quintessentially molecular disease that defies even rudimentary understanding without a firm foundation in the central paradigm of molecular biology, has reinforced the urgent need for reforms in medical student curricula. These changes are coming at a time when most medical schools in South Africa and abroad are adopting integrated problem-based learning for medical education. While such approaches are very effective in setting a relevant context for clinical medical education, there is the risk that basic sciences can be overlooked or under-emphasised. This introductory chapter reviews why it is necessary to devote special attention to the teaching and learning of molecular medicine in South African medical schools today.
The global explosion in molecular research
The history of scientific progress characteristically follows an uneven pathway, the pace and direction of which are very much dependent on the availability of technology appropriate to answer the questions of the time. Barriers to further progress are broken down by the development and deployment of new tools, which frequently do more than solve hitherto insoluble problems – they also tend to determine the character of the next generation of questions. An example of this principle in the history of biomedical science is the invention and deployment of the compound microscope in the seventeenth century. The revelation of tissues and cells that this tool enabled paved the way for a new pathology, spawning centuries of scientific endeavour characterised by an understanding of the cellular basis of disease and the whole science of microbiology. This new state of the art itself came to encounter impenetrable barriers to further progress towards the end of the twentieth century. Characteristically, further progress had to await widespread deployment of a new technology – that of molecular biology – before these barriers could be overcome and a new course set (Figure 1).
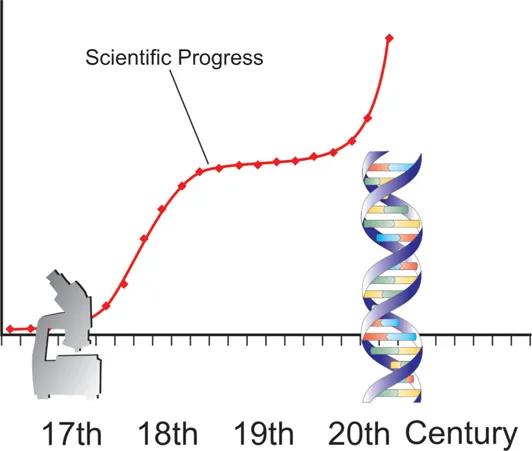
Fig. 1: Scientific progress is frequently punctuated by the development of new technologies. One such leap in medical science was enabled by the invention of the microscope in the 17th century. Another such opportunity emerged during the latter part of the 20th century, with the development of a range of extremely powerful molecular tools that are ideally poised to answer many of the questions medical science was previously unable to address adequately.
In virtually all medical specialties, the lion’s share of publications with a molecular theme has been published since the beginning of the 1990s. Assuming a typical delay between the appearance of the primary reference and its subsequent reflection in reviews, textbooks and curricula to be of the order of a decade, it is therefore self-evident that any medical curriculum, in virtually any area of medicine, that has not been revised this millennium is probably unacceptably out of date, at least from a molecular perspective. The impact of any deficiency in the currency of a medical curriculum is even more apparent when it is borne in mind that medical schools have a duty to prepare their students for medical practice many years in the future.
It is not within the scope of this introduction to attempt to do more than outline the expanding role of molecular medicine in medical practice. It is, however, important to note that the pivotal role of molecular science and technology in pathology and diagnostics is no longer conjectural, but established. Moreover, there is a growing impact of molecular science in the refinement, application and design of therapeutic interventions. Suffice it to say for now that it is already clear that fields such as genomics are becoming to medicine what information technology generally became to everything else in society, and that the post-genome era and the study of functional genomics, using tools such as gene expression micro-arrays, proteomics and cytomics, are set to continue this revolution. A medical education curriculum that is unacceptable from a molecular perspective is today therefore unacceptable from any perspective.
What does the newly qualified doctor need to know about molecular medicine, and why?
The publication of the first draft of the human genome and other high-profile topics such as genetically modified organisms and mammalian cloning have generated unprecedented public interest in molecular biology, genetics and biotechnology, which in turn have become mainstream political issues. This has produced a public that is far more intensively aware of threats and opportunities presented by scientific progress than at any other time in human history. The Internet has fuelled the spread of this knowledge explosion, and the result is that patients, especially affluent patients with chronic diseases and access to the internet, are very often extremely well informed about the existence of some of the scientific minutiae underpinning their diseases, and one of the tasks they demand of their doctor is to put these details into some kind of perspective for them. Unlike the patient, who has only one disease on which to focus the Internet search, the doctor has to have a conceptual understanding of the molecular and cellular basis of hundreds of diseases. For instance, the doctor needs to know about the cell cycle, apoptosis and their molecular regulation, because the patient has learned that p53 is central to his/her disease process.
It is not just the affluent patient who is demanding new knowledge and skills from the doctor. HIV/AIDS has generated furious debate around the issue of antiretrovirals, for example, and this begs the question, why ‘retro’? Even to begin to answer this question demands a thorough acquaintance with the central paradigm of molecular biology – an understanding of transcription is an obvious prerequisite for any comprehension of the process of reverse transcription. Patients demand to know their CD4 counts, and action groups know about the costs of PCR for viral load determination. Doctors need to be at least one step ahead of patients in understanding the disease and its treatment and monitoring, and this is just not possible today without a firm grounding in the principles of molecular medicine. Moreover, medical practice in resource-poor settings demands a greater, rather than a lesser, understanding of the fundamentals of disease and therapy. A practitioner in such circumstances faced, for example, with unavailability of a specified drug, needs to understand the disease process to make rational decisions concerning the selection of alternatives.
Formal curricula for the training of medical doctors in South African medical schools
This changing scientific landscape is transforming medicine ‘from the world’s oldest art to the world’s youngest science’ (Lewis Thomas 1978), and the change is happening at precisely the same time as another revolution in medical education – that of integrated basic and clinical science education and problem-based learning. Reflecting international trends, virtually all of South Africa’s medical schools have moved, or are moving, from a traditional curriculum to one that is contextualised to the patient scenario from an early stage. It is not the intention of this preface to attempt to explore in any detail the pros and cons of this shift, beyond to summarise perhaps that the great appeal of problem-based learning is the notion that learning in context is more appealing than learning in isolation, and the context that appeals to the majority of medical students is the patient-orientated context. There can however be no denying the threats posed by the new curricula to the formal teaching of basic sciences, and this is perhaps especially so in respect of physiology, medical biochemistry and molecular medicine, the overarching broad principles of which may often be difficult to cover adequately within the narrow context imposed by a single case. A compromise to the dilemma exists, perhaps uniquely for the teaching of molecular medicine in Africa, because the clinical and social context of HIV/AIDS just happens to be an ideal context for the teaching of applied molecular biology.
What about specialist training?
The major clinical benefits derived from the molecular revolution so far have been diagnostic. This has by no means been confined to affluent patients demanding personalised medicine. Arguably the countries that have benefited most from the application of genomic knowledge have been those of the Mediterranean littoral region, whose socio-economic burden of managing thalassaemia major has been significantly reduced by the widespread deployment of antenatal diagnostic programmes, underpinned by molecular genomic technology. In Africa, molecular research and development programmes and molecular techniques are being deployed at an escalating pace in the diagnosis and monitoring of HIV/AIDS, and this is emerging as an irreplaceable component of any effective treatment campaign. Moreover, molecular diagnostics, which have long been recognised as pivotal in the diagnosis of inherited disease, are increasingly seen globally to be fundamental in diagnosis, drug selection and monitoring of other infectious diseases, and a growing number of cancers as well.
A relative deficiency in the supply of skilled staff in the developing, as opposed to the developed, world creates a challenge for developing country medical schools in the postgraduate arena. Realistically, it seems unlikely that the shortfall will ever be made up, and herein lies the real challenge – if developing countries cannot afford to catch up with those of the developed world, perhaps all they can afford is to jump ahead of them. A conceptual precedent for this concerns the deployment of cellular communications technologies in regions lacking landline infrastructure. Molecular medicine and its tools make this leapfrog philosophy a distinct possibility for medical diagnostics, and not just a pipe-dream. This is partly because the enormous diagnostic power of molecular technology lends itself to a systems approach, in which diagnostic capacity, previously available only to a select few highly trained and expensive personnel, can be reduced to a technological process, and partly because one of the major barriers to implementation of such processes is the very existence of the legacy technology. Thus the deficiency in obsolete methods constitutes a distinct advantage for a developing world country with the will to install state of the art solutions.
The major implications of molecular tools for medical practice have so far been largely diagnostic, including in that category a refined understanding of pathogenesis – the basic mechanisms of disease. This new awareness of disease mechanisms creates a new opportunity for rational therapeutic intervention, especially when coupled with the expanding power of the methods available to the investigation of functional genomics in the post-genome era. The study of proteins and their functions has been revolutionised by so-called proteomics methods, combining the powers of information processing with mass spectrometry, while the study of living cells has been facilitated by such methods as confocal microscopy and functional flow cytometry. Interventions targeted at specific genes have been made possible by designer interference at the RNA level, by a variety of exciting new methods. All this therapeutic potential appears to be poised at the crest of a new wave of molecular pharmacology, which seems set to revolutionise medical practice even more dramatically than the diagnostic revolution referred to above. There are already new drugs available that are specifically designed to counter the central pathological molecules at the heart of the disease process, and many more seem to be in the offing.
It is clearly vital not to fail to identify this new therapeutic phase in the practice of medicine, at least conceptually at this stage, in designing the new curricula for medical student education. It is also important that the concepts are contextualised to give them relevance to the medical practice that is currently topical. In South Africa, HIV/AIDS happens to be a fertile learning ground for medical students in need of instruction on how specific molecular interventions may be designed, partly because so much is known about the crystallographic molecular anatomy and pathophysiology of HIV proteins (Figure 2), and partly because the relevance of the disease to medical practice in South Africa is self-evident.
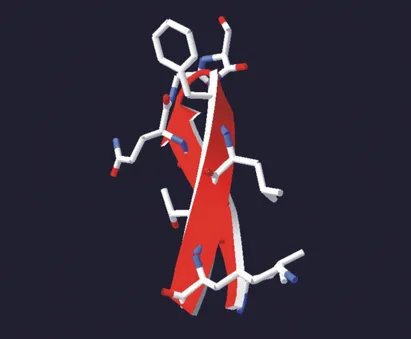
Fig. 2: ‘Residues 37-46 of the human CD4 molecule. Virion or macrophage-associated HIV envelope glycoprotein gp120 binds this site with high affinity, displacing the physiological CD4-MHCII interaction and hypothetically thereby causing death of the activated T cell by apoptosis. It is through this interaction that the virus is able to infect CD4 bearing cells, including macrophages. Curiously, unmodified depiction of the secondary structure reveals an antiparallel beta sheet with a remarkable resemblance to the AIDS ribbon.’ (Nutrition, HIV/AIDS and TB: scientific enquiry into nutritional influences on human immunity with special reference to HIV infection and active TB in South Africa. (2007) ASSAf report cover picture, Swiss PDB file 1G9M, from Kwong et al. and Berman et al., see p 495)
CONCLUSIONS
There is a growing recognition worldwide of the critically important nature of the molecular dimension of medical practice, and space and time is being allocated to medical student curricula to ensure satisfactory coverage of the basic principles. This is offered as a formal comprehensive course during the foundation-building phase of the undergraduate curriculum, and reinforced by a spiral curriculum, in which concepts are revisited and extended in differing contexts. In order that molecular medicine is perceived by clinical teachers and students to be relevant to current medical practice, teaching and learning should be contextualised to important clinical problems, and these should not be restricted to inherited diseases, but should include the molecular dimension of infectious diseases and cancer as well. HIV/AIDS is an eminently suitable context for the teaching and learning of molecular principles for medical practitioners and students.
With regard to postgraduate training, in view of the established role of molecular techniques in the diagnostic process, pathology programmes are arguably those most in need of intensive, formal molecular diagnostics courses. Such courses are already offered in many schools. As molecular technology transcends the traditional interdisciplinary barriers, and mindful of the deficiencies in numbers of pathologists with reference to First-World standards, a full year of integrated multidisciplinary diagnostic molecular pathology appears to be a desirable component of postgraduate registrar training.
SUMMARY
•Progress in medicine has always been driven by advances in science and technology.
•Recent advances in the scientific understanding of the molecular dimension of biology have seen widespread deployment in medicine.
•Under- and postgraduate curricula in medical education are urgently in need of major reform so as to enable major recent advances in medical practice to be communicated to current and future medical practitioners.
•Molecular insights into medical practice are eroding traditional barriers between medical specialties, paving the way for a more holistic approach to patient care, especially in terms of practical diagnostics, but also with growing therapeutic implications.
KEYNOTE ESSAY 1
Defining Who We Are: DNA in Forensics, Genealogy and Human Origins
Himla Soodyall
INTRODUCTION
Humans are fascina...
Table of contents
- Cover
- Title
- Copyright
- Contents
- Foreword
- Acknowledgements
- Chapter 1 Introduction
- KEYNOTE ESSAY 1: Defining Who We Are: DNA in Forensics, Genealogy and Human Origins
- SECTION 1 PRINCIPLES OF CELLULAR AND MOLECULAR BIOLOGY
- SECTION 2 MOLECULAR PATHOLOGY
- SECTION 3 MOLECULAR THERAPEUTICS
- SECTION 4 RESEARCH AND THE CONTINUING EVOLUTION OF MOLECULAR MEDICINE
- GLOSSARY
- CONTRIBUTORS’ BIOGRAPHIES
- SOURCE MATERIAL AND RECOMMENDED READING
- PERMISSIONS AND CREDITS
- INDEX