eBook - ePub
Modern Techniques in Cytopathology
- 110 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Modern Techniques in Cytopathology
About this book
In the era of precision medicine, physicians are increasingly in need of more definitive diagnostic, prognostic, and predictive information derived from small biopsy specimens such as cytology samples in order to guide effective patient care. Cytopathology is well poised to meet this challenge. Whilst the traditional cytomorphologic component of cytology practice is still valid, enormous advances have been made in the field of cytopathology thanks to transformative technology and innovative individuals that have augmented the cytologists' ability to meet the demands of modern medicine. The purpose of this book is to describe, illustrate, and review many of the most recent developments regarding modern techniques employed in cytopathology. This latest monograph is intended for all cytologists including cytopathologists, cytotechnologists, cytology lab assistants, trainees, research scientists, and anyone who is interested in the field of cytopathology. We have invited pioneering experts in their respective fields to author these chapters. This book is not only the culmination of their groundbreaking work and effort but also presents a critical review of the current literature. We have attempted to provide readers with an informative and comprehensive aid so that they may better appreciate how emerging technology has been applied to cytology. Each chapter in this book presents a stand-alone contemporary review of emerging topics in cytopathology. We hope that you will find this monograph thought-provoking and a valuable reference for your practice.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Modern Techniques in Cytopathology by M.M. Bui,L. Pantanowitz,Marilyn M. Bui,Liron Pantanowitz,Marilyn M., Bui,Liron, Pantanowitz, Philippe Vielh,Philippe, Vielh,Liron, Pantanowitz,Marilyn M., Bui in PDF and/or ePUB format, as well as other popular books in Medicine & Gynecology, Obstetrics & Midwifery. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
Bui MM, Pantanowitz L (eds): Modern Techniques in Cytopathology.
Monogr Clin Cytol. Basel, Karger, 2020, vol 25, pp 1–5 (DOI: 10.1159/000455781)
Monogr Clin Cytol. Basel, Karger, 2020, vol 25, pp 1–5 (DOI: 10.1159/000455781)
______________________
The Interventional Cytopathologist and Ultrasound-Guided Fine-Needle Aspiration
Susan D. Rollins
ETSU Department of Pathology, Outpatient Cytopathology Center, Johnson City, TN, USA
______________________
Abstract
Ultrasound-guided fine-needle aspiration (FNA) biopsy allows for accurate sampling of mass lesions. The diagnostic information from this procedure is maximized when the pathologist is intimately involved with specimen procurement, specimen triage, and interpretation. This chapter discusses the role of the interventional cytopathologist, training opportunities, and basic information for starting a pathologist ultrasound-guided FNA clinic.
© 2020 S. Karger AG, Basel
In 2009, the College of American Pathologists began offering a course to cytologists in ultrasound-guided fine-needle aspiration (USFNA) biopsy entitled Ultrasound-Guided Fine-Needle Aspiration Advanced Practical Pathology Program (USFNA AP3). Prior to this, only a handful of cytopathologists were performing their own USFNA biopsies. In less than a decade, cytopathologists have realized the utility of learning and practicing USFNA. The technique is now taught in residency and fellowship programs. Highlighting the importance of USFNA in cytopathology training programs, the July 2015 ACGME and ABP Cytopathology Milestone Project (PC2) cited this skill as a level 4 milestone in cytopathology training. According to this milestone the cytology trainee should have the following competency: “Describes and discusses indications and/or performs ultrasound-guided FNAB and core-needle biopsy” [1].
The scope of practice for clinical cytologists is markedly expanded when USFNA is added to their repertoire. In addition to palpable masses, cytologists have the opportunity to sample non-palpable superficial targets. Sampling of palpable masses is also improved. The cytologist has control over needle gauge, number of passes, area of lesion sampled, and, based on rapid on-site cytologic evaluation (ROSE), specimens can be appropriately triaged for ancillary studies such as cell block, immunocytochemical stains, cultures, flow cytometry, molecular studies, and/or core-needle biopsy. With experience, the cytologist can learn how to correlate ultrasound (US) features of a mass with the cytologic findings and can integrate this information into the cytology report to better guide clinicians in appropriate follow-up care and specialist referral. The ability to link the cytology procedure and report to patient management algorithms is immensely valuable for the patient and can be personally gratifying for the clinical cytopathologist. Cytologist-centered USFNA offers patients streamlined, cost-effective, and personalized care.
ROSE of FNA biopsy specimens helps ensure adequate samples for cytologic interpretation. A downside of ROSE is that either a cytotechnologist or pathologist must be on site in radiology or a clinic where the biopsy is performed, which can be a time-intensive endeavor [2]. Even though reimbursement for ROSE is offered, the reimbursement is low and valuable pathologist time is lost [3]. Additionally, if ROSE is undertaken by a cytotechnologist, critical decisions about triage of the specimen may not be possible. Cytopathologist USFNA is preferred over traditional paradigms in which the biopsy is performed by a non-pathologist because the imaging physician assigned to do the biopsy may not be skilled in USFNA. The physician may not understand the importance of sampling masses in specific areas to optimize the sample and could be resistant to suggestions about where to biopsy for optimum sampling. When not under the purview of a cytopathologist, slide smearing and specimen preparation can be poor when it is done by a person not acutely aware of the fragility of cells. A poor smear can sabotage all other aspects of the FNA procedure; therefore, this seemingly simple part of the process is often undervalued by those not intimately involved with specimen interpretation [4].
Training
To date, several didactic and hands-on courses are available to cytopathologists to learn USFNA. The College of American Pathologists’ AP3 multiday course covers topics including the basic physics of US, criteria for stratifying risk of malignancy of a lesion based on US criteria, techniques of needle placement using US guidance, importance and practice of specimen preparation and smearing, and medical coding. If the participant passes two practical examinations and a written exam, a certificate valid for 5 years is awarded for this accomplishment. Other learning venues include courses offered by The American Association of Clinical Endocrinologists (AACE). USFNA courses and poster presentations are now a part of meetings sponsored by the ASC, USCAP, CAP, and ASCP.
Cytologists are eligible to apply for ECNU (Endocrine Certification in Neck Ultrasound) certification. For such certification, the candidate must pass the Comprehensive Certification Examination (CCE) and successfully complete the Validation of Competency Process (VCP). Cytologists who pass this rigorous curriculum may use the ECNU designation after their names.
Taking a course in USFNA is just the beginning of learning the art of US-guided needle placement and correlating mass image characteristics resulting in an integrated cytologic diagnosis. Dedicated practice is needed since every patient can present a slightly different challenge to the aspirating physician, whether that be an anxious or non-compliant patient, body habitus, or location of the mass. Part of what makes USFNA an interesting and challenging endeavor is having to tailor each FNA procedure to the needs of the individual patient. Learning to target specific areas in a mass to within a few millimeters is an art. This takes practice, but when accomplished is very satisfying. The prescription is practice, practice, practice!
US-Cytology Correlation
The “triple-test” concept in breast FNA is not new to cytopathologists. Physical examination, imaging, and cytology findings all need to be taken into account for clinical guidance. Cytologist USFNA is an expansion of the “triple test” concept. Much can be learned about a mass to be sampled from its US characteristics: mass shape, margins, echogenicity, blood flow pattern, presence or absence of posterior acoustic shadowing, and characteristics of echogenic foci.
US features of a mass impart a degree of “relative risk” which can be classified as favor benign, indeterminate, or suspicious for malignancy. The categorization of a mass based on US findings closely parallels what pathologists are already very familiar with based on experience with gross and microscopic pathology. Correlation of US images and cytology findings is of utmost importance. If the US findings are suspicious for malignancy but the cytology is benign, the cytologist needs to determine whether there is a sampling problem or why the US and cytology do not correlate. In the case of benign-appearing US features and malignant cytology, the same correlation needs to be done. For example, a well circumscribed mildly hypoechoic breast mass with posterior enhancement could be classified as favor benign or indeterminate by US criteria, but is a mucinous carcinoma by cytology; the cytologist knows that the results correlate. The cytologist is in the perfect position to understand why these processes have their particular US characteristics. With experience, the cytologist can even begin to predict what cytology will show based on the US features of the lesion. Radiologists, even with the availability of ROSE, do not get to so closely correlate US findings and cytology findings.
Credentialing
At the time of writing this chapter, there is no credentialing required in order for cytopathologists to perform and bill for USFNA. However, no one can predict the whims of insurers and thus this may change.

Fig. 1. USFNA exam room setup.
Cytopathologists may have to meet certain standards by their employers or institutions for whom they work [5, 6]. Institutional requirements may vary greatly, and it is hoped that the cytopathologist will be instrumental with helping to establish credentialing requirements.
Equipment
For a cytologist with an active FNA service, very little additional equipment is required when expanding their service to USFNA. There are numerous US machines available at various price points and features. Choice of a portable or floor model depends on personal preference. For USFNA of superficial masses, a linear high-frequency transducer is required. A small transducer footprint will allow for easier sampling of masses in the head and neck region. Unless a specialized feature such as elastography is desired, almost any modern US will meet the needs for a cytologist doing USFNA. When selecting an US machine, it is important that the buyer is comfortable with the image quality and ease of the user-machine interface. It is important to not only consider the purchase price of the unit, but also the warranty, cost of service contracts, use of a loaner unit if repair is required, and amount of time offered to train personnel in the use and setup of the machine.
The procedure room requires a patient procedure table (Fig. 1). This can range from a simple bed to a hydraulic procedure table. It is helpful to have a bed that has the capability to raise or lower the head so that the patient can be sitting, semi-recumbent, or flat. A table that can be lowered to 20–24" from the floor helps enable the transfer of patients with poor mobility. A pillow is needed for neck extension for thyroid biopsies. Bolsters for stabilizing patients when rolled onto their side and for placement under their knees to relieve pressure in the lower back are also helpful and appreciated by patients. It is very useful to setup a second monitor projecting the US image on a screen on the opposite side of the bed from the US monitor. This allows for easier setup for biopsy needle guidance.
Consumable items include US probe covers, choice of skin preparation (alcohol, betadine), anesthesia options, US gel, needles, and syringes. Probe covers come in a variety of styles. Skin preparation can be done with alcohol, betadine, or another cleansing agent. Anesthesia ranges from none to cutaneous preparations to injectables (Fig. 2). Needle gauge choice is dependent on the site being sampled, vascularity of the mass, the patient’s coagulation status, type of lesion sampled, and personal preference. Slip-tip syringes are recommended over luer-lock syringes so that the needle can easily and quickly be removed from the syringe, allowing for more rapid smear preparation and less chance for smear artifacts. Standard needles used for drawing blood are sufficient for aspiration biopsies. It is helpful to have a variety of needle gauges and lengths available. This allows the aspirating physician to choose a needle gauge based on the lesion being sampled, patient coagulation status, and Doppler vascularity of the mass. Use of a syringe holder (gun) is at the discretion of the aspirating physician; several styles are commercially available. A needle-only technique can be used to sample many masses. Some clinicians like using an adaptor between the needle and the syringe so that the needle-only technique can be used for needle placement, while an assistant can apply suction on an attached syringe.
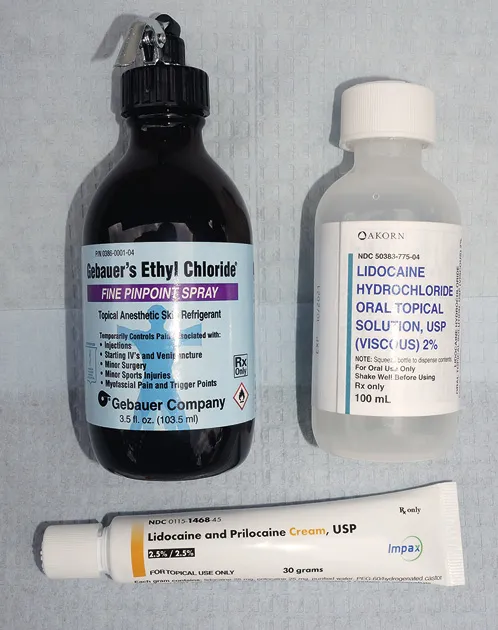
Fig. 2. Cutaneous anesthesia options.
Reporting
In September 1996, the National Cancer Institute (NCI) sponsored a consensus conference to define a uniform approach for reporting breast FNA biopsy cytology. Twenty years later, the executive of the International Academy of Cytology (IAC) named a Breast Group including cytopathologists, surgical pathologists, radiologists, surgeons, and oncologists to draft a standardized reporting system for breast FNA that could be employed widely in both developed and underdeveloped countries. The structured report includes management recommendations to enhance the clin...
Table of contents
- Cover Page
- Front Matter
- Chapter 1: The Interventional Cytopathologist and Ultrasound-Guided Fine-Needle Aspiration
- Chapter 2: Cell Blocks: Evolution, Modernization and Assimilation into Emerging Technologies
- Chapter 3: Fluorescence in-situ Hybridization in Cytopathology
- Chapter 4: Next-Generation Sequencing in Cytopathology
- Chapter 5: Liquid Biopsy: Recent Advances in the Detection of Circulating Tumor Cells and Their Clinical Applications
- Chapter 6: Computer-Assisted Pap Test Screening
- Chapter 7: Telecytology for Rapid On-Site Evaluation
- Chapter 8: Whole-Slide Imaging in Cytopathology
- Chapter 9: Image Analysis in Cytopathology
- Chapter 10: Other Cytology Applications: Clinical Trials, Checkpoint Inhibitors, and Cytobanking
- Author Index
- Subject Index
- Back Cover Page