![]()
PART ONE
THE BASICS
![]()
All About Fibroids
What Is a Fibroid Tumor?
No one really knows what causes fibroids, known in medical terms as leiomyomata. In fact, no one knows what causes any type of tumor at all. We do know that a fibroid is a smooth muscle tumor of the uterus that is composed of exactly the same tissue as that organ. But a fibroid is usually encapsulated by another band of tissue, and it grows independently Many holistic health practitioners view this rogue tissue growth as nature’s way of isolating and protecting the body from toxins caused by poor diet and environmental poisons that cannot be disposed of through the organs of elimination.
Practitioners of Chinese traditional medicine and other ancient Asian modalities blame blockages of “chi,” or life force energy, in the channels that lead to and course through the female organs and glands. In traditional eastern medicine, the free flow of chi through these channels, also known as meridians, is the essence of optimum health.
Along with other holistic medical practitioners, I suspect that long-standing disturbances that create hormonal imbalance may be at the root of this condition. Yet all we know for sure is that the female hormone estrogen stimulates fibroid growth. Some evidence suggests that progesterone might also stimulate fibroid growth. This theory is supported by the fact that fibroid tissue, just like uterine tissue, contains both estrogen and progesterone receptor sites. However, medical experts also know that these progesterone receptor sites may actually allow that hormone to favorably affect that tissue.
Some lucky women with fibroids have no symptoms. Others are not so fortunate. They suffer from a myriad of complaints, including lower abdominal pain and pressure, heavy menstrual bleeding, between-period bleeding, infertility, miscarriages, anemia (and associated weakness and dizziness), indigestion, chronic vaginal discharge, constipation, urinary frequency, and bladder irritation and infections.
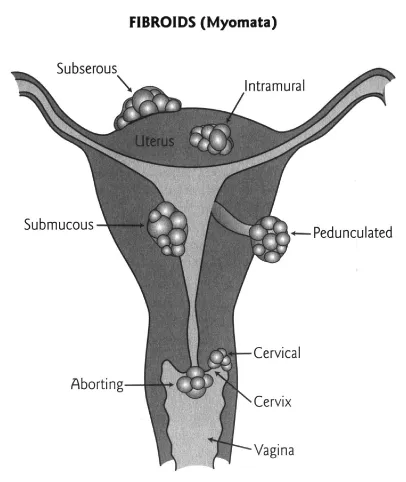
Fibroids can grow in many different locations around and in the uterus, and there are four different types. Each type can create its own set of problems, and most fibroid conditions include at least two kinds of fibroids.
Subserous fibroids appear on the outer wall of the uterus and commonly cause the uterus to grow This type of fibroid usually grows during menstrual periods because increased blood flow supplies it with more nutrients. Menstrual periods often cause greater abdominal bloating and worsening of all other symptoms. Subserous fibroids also typically cause painful intercourse and pain in the back and/or the groin that can even shoot down the legs. Fibroids, especially this type, can expand a uterus to the size of a watermelon or a seven-months pregnancy, which often puts pressure on adjacent organs. Pressure on the bladder or the bowels creates a whole set of problems, including constipation, incontinence, or the inability to urinate. I have even had to send some women to the emergency room in the middle of the night to be catheterized, because they were unable to urinate. This type of fibroid can cause kidney damage by pressing on the ureters, the tubes that connect the kidneys to the bladder.
Submucosal fibroid tumors develop inside the uterine cavity. They can cause severe abdominal cramping that simulates the pains associated with childbirth, because the fibroid is situated inside the uterus, where a baby would develop. The uterus cramps because it is trying to “deliver” it, just like a baby. In a condition called “an aborting submucous myoma (fibroid tumor),” the uterus actually does expel the fibroid through the cervix and vagina, causing severe abdominal cramping and heavy bleeding. Submucosal fibroids are also typically associated with major bleeding problems. Sufferers tend to hemorrhage during heavy, often lengthy periods. Women with this type of fibroid often feel weak from blood loss. They are anemic, anxious, and frightened. In fact, submucosal fibroids bring the most women to surgery, where, all too often, they are given complete hysterectomies. Unfortunately, this type of fibroid is the most difficult to heal through holistic means.
Intramural fibroids grow within the actual uterine wall and cause many of the same symptoms as the other types. (This is the type of fibroid that brought Janet to my office.) Intramural fibroids can either grow toward the outside of the uterus and cause the same symptoms as the subserous fibroid, or grow in the direction of the inside wall, creating symptoms similar to the submucosal type.
Pedunculated fibroids are attached to the uterus by a stalk. Because of that appearance and position, they sometimes mimic ovarian tumors. This type can appear like a big ball on the outside of the uterus when imaged through ultrasound or other visual technologies. Even with modern radiological imaging techniques like CAT scans and MRIs, it is sometimes impossible to distinguish between this type of fibroid and an ovary or an ovarian cyst or tumor. For that reason, many women with pedunculated fibroids come to surgery simply to be diagnosed. If the surgeon is conservative, he or she will remove the fibroid only. But an aggressive doctor often removes the entire uterus and, sometimes, the ovaries as well. Typically, a woman with a pedunculated fibroid either feels nothing at all or, if the fibroid is pressing on another abdominal structure, she experiences cramping associated with nausea and vomiting. In cases where the pain is sharp, the pedunculated fibroid could be twisting on its stalk, causing severe abdominal pain similar to that associated with peritonitis or acute abdominal infection. Of course, this condition is a surgical emergency. As is the case with most fibroids, location is key in deciding whether or not a hysterectomy is truly indicated.
Fibroids and Cancer
Only about 1 percent of fibroids are malignant, but no one knows whether they are malignant to begin with or develop into malignancies. The only indication that a fibroid is malignant is unusually rapid growth. Even when it has been removed surgically, the pathologist must section the fibroid multiple times and count the number of cell divisions in order to detect a malignancy, because malignancy cannot be detected by the fibroid’s appearance. Another way to discover whether or not a rapidly growing fibroid is malignant is by the antimalignin antibody in serum (AMAS) or AMAS test, an FDA-approved test that detects malignancy anywhere in the body Cancer cells produce a protein called malignin. The body manufactures an antibody to malignin. If that antibody to malignin is detected by the AMAS test, we know that malignant cells are somewhere in the body. The AMAS is quite accurate, so I advise any doctor to do an AMAS test before treating a suspicious fibroid.
To Have a Hysterectomy or Not to Have a Hysterectomy?
When I was training to be a physician, if a woman over forty-five years old had any type of abdominal surgery whatsoever, the surgeon would just go ahead and remove the uterus and ovaries as well, “just in case.” Today, thirty years later, the ovaries and uterus are still considered unnecessary organs after the childbearing years. Many women tell me to this day that their gynecologist said they need a hysterectomy, and since they don’t plan to have more children, they “don’t need” their uterus any longer. Since they are removing the uterus, the doctor might add, “Let’s take out the ovaries while we’re in there, so we can eliminate the possibility of ovarian cancer.” When these women object that they don’t want to suffer the symptoms of sudden menopause associated with this surgery, they are told, “Oh, you can take Premarin, and you’ll be fine.”
Too many gynecologists continue to view hysterectomy with this cavalier approach, especially when treating women over the age of forty. In cases involving larger fibroids that create serious problems, hysterectomy is necessary Unless the fibroid condition is life threatening, though, hysterectomy should never be the first choice of treatment. Emerging evidence suggests that instead of resolving a woman’s health problems, a hysterectomy can turn a bad situation worse. We now know that both the uterus and ovaries continue to perform health-enhancing functions throughout a woman’s life. The ovaries produce at least four hormones that we know of: estrogen, progesterone, testosterone, and DHEA. The problem is that many doctors are unaware of the important role testosterone and DHEA have in maintaining hormonal balance, energy levels, and good health in a woman’s later years. Testosterone is not an exclusively male hormone, as is popularly believed. Everyone needs this anabolic, or “building up,” hormone to maintain and build muscle and bone and to tone the body’s structure as a whole. In women, testosterone specifically works to protect the libido, promote a sense of well-being, and increase muscle tone and strength. Recent evidence indicates that testosterone is also instrumental in preventing and treating osteoporosis. A deficiency of this essential hormone has been proven to make women feel weak and fatigued; uninterested in their lives, work, and relationships; even, at times, emotionally distraught.
DHEA, popularly known as the anti-aging hormone, helps us cope with modern lives fraught with constant, heavy stress. Many busy women suffer from adrenal weakness caused by putting out too much cortisol, the hormone that is released by the adrenal glands in response to stress. This prevents the adrenals from producing enough DHEA, which leads to a deficiency. The symptoms of low DHEA levels include sleep disturbances, mood swings, and constant fatigue. Sound familiar? DHEA is also a precursor hormone, which means that your body needs it to produce other key hormones, including estrogen and testosterone. Since many of us are overstressed and therefore deficient in DHEA, we are consequently susceptible to multiple hormone deficiencies and imbalances and related health issues, such as fibroids. If a woman has a hysterectomy, she risks an even greater deficiency in DHEA.
We have learned that even the tiniest excess or deficiency of these life-sustaining natural chemicals that we call hormones can have a profoundly negative impact on our health, so you can imagine the effect on hormonal balance caused by the sudden disappearance of a woman’s uterus and/or ovaries.
And that’s all we know about the lifelong health-preserving functions of the ovaries and uterus so far! There may be other benefits of keeping these organs throughout a woman’s lifetime that we have yet to discover.
Of course, we cannot ignore the reality that hysterectomy is a major surgery, which requires up to one year for full recovery. Nor should we ignore its possible harmful effects and complications. Not only are women of childbearing age robbed of their ability to conceive and carry a child; a significant number of women die from surgical complications. In 1975, a study found that out of 787,000 hysterectomies performed in this country, 1,700 led to the patient’s death. There may be a few less hysterectomies performed these days (probably because of the influence of women’s advocacy groups), but the percentage of deaths caused by complications resulting from this serious procedure is most likely the same.
Possible complications are many, varied, and sometimes severe. Many women whose uteruses are removed because of fibroids also lose their ovaries at the same time. Even if they are not removed, blood flow to the ovaries is often reduced, so that these organs no longer function well. In fact, premenopausal women who undergo a hysterectomy without ovary removal still begin menopause on the average of five years earlier than women with intact uteruses. Lowered blood flow causes their ovaries to age prematurely. Removing the uterus and ovaries causes a sudden drop in estrogen and progesterone levels, which can lead to a host of health problems that mimic the symptoms of menopause. These include vaginal dryness and sudden and severe hot flashes. Some doctors even attribute adrenal and pancreatic problems, including diabetes, to the shock of removing the female organs. Studies also indicate that for a thirty-five-year-old woman who has undergone a hysterectomy, the risk of heart attack or angina is seven times greater. Ironically, women who undergo hysterectomies to cure their fibroids are often advised after the surgery to supplement estrogen, the very same hormone that fueled the growth of their fibroids—and possibly caused other health problems—in the first place.
Most gynecologists feel that only estrogen is necessary as a hormone replacement after the uterus has been removed, despite the fact that both estrogen and progesterone receptor sites are found in many other areas of the body, such as the breasts, colon, brain, muscles, and bones. In other words, hormone balance is not just key to gynecological health, it is also essential to the body’s overall health.
So why do a majority of doctors believe that a woman without a uterus needs only to take estrogen? In any case, hormone replacement therapy fails to address the underlying cause of the fibroid condition, which is hormone imbalance. In fact, hormone replacement therapy could aggravate an existing imbalance, setting up a woman for additional health problems, such as gallbladder disease, diabetes, breast disorders, and blood-clotting problems.
The list of post-hysterectomy complications goes on:
SEVERE BLEEDING. Severe bleeding can occur during the surgery and afterward. With today’s concerns about the dangers of blood transfusions, bleeding has become a more significant issue.
IMPAIRED BLADDER FUNCTION. Many women suffer from post-hysterectomy bladder-function problems. They can develop a fistula, which creates a connection between the vagina and other organs. For example, if the vagina and bladder are bridged by a fistula, urine can leak into the vagina.
BOWEL INJURY. The bowels can be injured during a hysterectomy procedure.
VAGINAL VAULT PROLAPSE. During most hysterectomies, the cervix is removed, which involves cutting into the back of the vagina. This procedure sometimes leads in later years to vaginal vault prolapse, a condition in which the back of the vagina (known as the vault) falls out through the front, necessitating yet another risky surgical procedure.
LOWERED SEXUAL RESPONSE. Removing the cervix can lower a woman’s sexual excitement during intercourse, because the cervix is key to sexual response in many women. In addition, many women experience the waves of orgasmic contraction and release within their uteruses. A hysterectomy robs them of that pleasure.
NEGATIVE PSYCHOLOGICAL EFFECTS. Finally, the psychological effects of a hysterectomy can be devastating. Some observers have equated hysterectomy to male castration, especially if the need for that surgery is later judged questionable. Few male physicians will accept that analogy, but the loss of a woman’s womb and ovaries can be experienced as a deep psychic wound that shatters her very identity.
Despite these serious complications and outcomes, many doctors believe that the sooner and more aggresively a serious fibroid condition is addressed, the better. Medical schools do not offer their students training in holistic medicine, so many of the treatments I recommend seem to most doctors like brand-new, unproven ground. This is one reason why so many physicians are still telling their patients that hysterectomy and the newer aggressive treatments are their only options.
I wrote Healing Fibroids to tell you why that’s just not true!
Fibroids and Hormones
Let us take a moment to sum up. You learned that no one knows all that much about why fibroid tumors develop, and few conventional doctors agree on the most effective treatments. Yet nearly all doctors—conventional and holistic practitioners alike—agree on one undeniable fact: fibroids are a serious, perhaps even escalating, threat to the health of too many American women. We have also learned that mounting evidence suggests fibroids are responsive to hormones because fibroid tissue is known to have receptor sites for both progesterone and estrogen. Other proof of the hormone connection is that women in estrogen-dominant states also tend to have large and rapidly growing fibroids. Fibroids are known to grow excessively during periods of high or excessive estrogen levels, such as pregnancy or the estrogen dominance that often occurs during perimenopause (the early stage that leads up to menopause). Once a woman is menopausal (which begins after one year of no periods) and her hormone levels become low, fibroid size often shrinks. Of course, if she is treating menopause with hormone replacement therapy, the fibroids usually do not shrink.
Some doctors try to reduce fibroid size by prescribing medications such as Synarel or Lupron to lower hormone levels; these are known as gonadotropin-releasing hormone (GnRH) agonists. But these GnRH agonists carry a risk of negative effects. One major negative effect is that GnRH agonists induce a sudden and severe menopausal state, with all the related symptoms—severe hot flashes, vaginal dryness, mood and mental changes, and increased risk for osteoporosis. Studies are being conducted on a new drug called tibolone, which is used in Europe instead of hormone replacement therapy. Tibolone is a synthetic hormone with estrogen-like and progesterone-like properties. It exerts only one-tenth the strength of the body’s natural estrogen and progesterone. It can be used with GnRH agonists to reduce those negative menopausal symptoms.
Studies on the relationship between progesterone levels and fibroid growth are less than clear, because they have yielded conflicting results. Some studies suggest that high levels of progesterone reduce, even stop, fibroid growth. Other studies show just the opposite: high blood levels of progesterone lead to increased fibroid growth. One problem with these studies is that they are performed on fibroid cells in tissue cultures that are outside of the body. Studies using the anti-progesterone medication RU-486 seem to indicate that when progesterone levels are low, fibroid size reduces. But we do not know at this time what other antifibroid effects RU-486 might have. Other studies have been conducted to evaluate the effects on fibroids of the group of synthetic progesterones commonly known as progestins (Provera is one brand name). One group of women scheduled for hysterectomies took progestins for a week before surgery in order to evaluate the effect on their fibroids. After the fibroids were surgically removed, researchers noted cellular changes within the fibroids that indicated reduction in growth. All these studies and clinical results suggest to me that what really counts is not the blood level of estrogen or progesterone but the balance between these complementary hormones. Rather than teasing out one hormone and looking for its particular effect on fibroid growth, I believe that the balance between estr...