Minimally Invasive Surgery in Gynecological Practice
Practical Examples in Gynecology
- 332 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Minimally Invasive Surgery in Gynecological Practice
Practical Examples in Gynecology
About this book
Gynaecological practice has changed fundamentally in the last three decades and a large proportion of major pelvic operations has been replaced by minimally invasive approaches. This book will cover minimally invasive approaches in all aspects of gynaecology including general gynaecology, oncology, urogynaecology and reproductive medicine. The chapters are written at a level appropriate for trainees/residents and general gynaecology specialists but enough details and additional resources will be provided for those who require further information. Specific aim of the book is to provide direct to the point surgical pearls which can be adapted to the daily practice instantly by the target audience. The book includes chapters on relevant surgical anatomy, principles of MIS, management of camera systems, video/image editing, initiating a successful MIS practice, improving efficiency of current MIS program, how to develop successful teaching techniques in academic setting, avoiding & managing MIS related surgical complications and preoperative/postoperative care before covering MIS for individual conditions including intensive care managements. Chapters are written by world renown authorities.
ACOG guideline recently published a statement recommending vaginal hysterectomy and endoscopic hysterectomy should be considered as a first step of surgical choice. Current practice has been shifting from open cases to laparoscopic/ robotic assisted cases while vaginal cases stays steady. This shift has created an urge among gynaecologists to learn, improve or adapt laparoscopic/ robotic techniques in their practice.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1 Practical fundamentals of retroperitoneal spaces for safe pelvic surgery: possible answers to difficult questions
1.1 Does a general gynecologist need to know about retroperitoneal pelvic anatomy ?
1.2 What are the superficial anatomical landmarks of retroperitoneum?
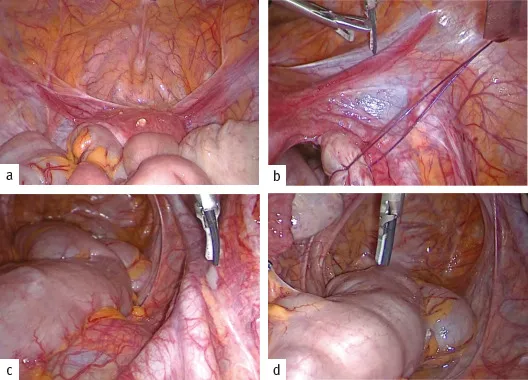
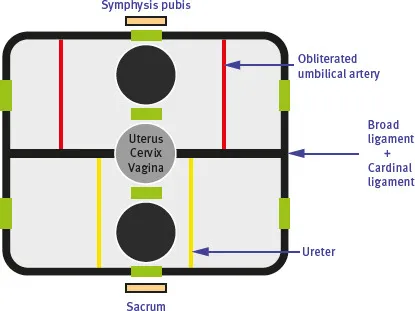
- The peritoneum on the lower anterior abdominal wall is raised into five folds (reported as “ligaments”), which diverge as they descend from the umbilicus. They are the median, right and left medial, and right and left lateral umbilical folds.The median umbilical fold extends from the apex of the bladder to the umbilicus and contains the urachus. The medial umbilical fold covers the obliterated umbilical artery. Under the lateral umbilical fold, the deep inferior epigastric vessels can be found, below their entry into the rectus sheath.
- Superior vesical arteries, on both sides, form the transverse vesical folds on the bladders dome.
- Uterine artery, on both sides, passes between the two peritoneal layers of the broad ligament, within the cardinal ligament (of Mackenrodt or lateral parametrium), and crossing over the ureter.
- Pelvic ureter enters the lesser pelvis at the level of the sacral promontory, anterior to the end of the common iliac vessels (more frequent on the left side) or at the origin of the external iliac vessels (more frequent on the right side).
- Uterosacral ligaments form the recto-uterine folds, containing some pelvic autonomic nerve fibers in its postero-lateral part. In some patients, it is also visible a more medial and caudal folder, enveloping the hypogastric nerves (HNs) and the inferior hypogastric plexus (or pelvic plexus) [8].
- Bifurcation of aorta (at the level of the fourth lumbar vertebra or the L4/5 intervertebral disc, to the left of the midline) and the left common iliac vein. Middle sacral vessels and the superior hypogastric plexus are located in the interiliac triangle (or Cotte triangle) at the level of sacral promontory, the starting point of pelvic cavity.
- Laterally, three somatic nerves from lumbar plexus: genitofemoral nerve lying on the psoas major muscle, and the iliohypogastric and the ilioinguinal nerves [9–11].
1.3 Is there a general scheme for the retroperitoneal space?
Membranous: parietal and visceral pelvic fasciae
Table of contents
- Title Page
- Copyright
- Contents
- Copyright page
- FOREWORD
- Preface
- Principal contributing authors
- 1 Practical fundamentals of retroperitoneal spaces for safe pelvic surgery: possible answers to difficult questions
- 2 Preoperative imaging for minimally invasive surgery in gynecology
- 3 Anesthetic considerations for minimally invasive surgery
- 4 Principles and safe use of electrosurgery in minimally invasive surgery
- 5 Laparoscopic entry techniques
- 6 Principles of laparoscopic suturing and alternatives
- 7 Challenges in minimally invasive surgery
- 8 Adhesions after laparoscopic and hysteroscopic surgery, prevention, and treatment
- 9 Laparoscopy/robotically assisted simple hysterectomy procedure
- 10 Abdominal approaches to uterine myomas (laparoscopic myomectomy) and morcellation
- 11 Surgical treatment of endometriosis
- 12 Management of benign adnexal masses
- 13 Surgery for fallopian tube disorders
- 14 Cesarean section scar defects and their management
- 15 Laparoscopic surgery for Müllerian anomalies
- 16 Minimally invasive techniques for urinary incontinence: laparoscopic/robotic-assisted Burch colposuspension (urethropexy)
- 17 Robotic procedures for management of apical compartment prolapse
- 18 Laparoscopic management of mesh complications
- 19 Laparoscopic surgery for cervical cancer
- 20 Minimal invasive surgery for endometrial cancer
- 21 Minimally invasive surgery (MIS) for epithelial ovarian cancer (EOC)
- 22 Neuropelveology—the medicine of the pathologies of the pelvic nerves and plexuses
- 23 Complications of laparoscopic surgery and their management
- 24 Hysteroscopy: instrumentation for diagnostic and operative hysteroscopy, distension media, and office hysteroscopy
- 25 Hysteroscopic surgery for submucosal fibroids
- 26 Hysteroscopic surgery for Mullerian anomalies
- 27 Avoiding complications in hysteroscopic surgery
- 28 Endometrial ablation techniques for heavy menstrual bleeding
- Subject Index