- 304 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Zero Bone Loss Concepts
About this book
Bone loss is still a major issue that dentists encounter, but it is a complication that can be prevented. This book combines years of clinical experience with peer-reviewed scientific evidence to present the different strategies that can be used to achieve zero bone loss—not just months after prosthetic delivery but years after treatment. The book is divided into sections on surgical techniques and prosthetic techniques, and there are case studies with recommendations and procedures for many types of clinical situations, implant choices, and prosthetic solutions.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
SECTION II
PROSTHETIC CONCEPTS

11
PROSTHETIC FACTORS FOR MAINTAINING CRESTAL BONE STABILITY

Understanding surgical factors is important but is only the first step on a path to a zero bone loss treatment outcome. The concepts of zero bone loss include restorative factors, and because the success of an implant and the associated bone stability are measured in the long term, the prosthetic factors are just as important as the surgical factors.
Nothing destroys the work of a good surgeon as easily as a poor prosthodontist. In fact, the best outcomes might occur when the entire treatment remains in the hands of a single practitioner who performs surgery and prosthetic work. Rather than viewing the situation from a purely surgical perspective (ie, a patient needs implants), it can be viewed as a prosthodontic problem with a surgical solution (ie, a patient needs new teeth, and implants are used as a support for these teeth). Crestal bone stability can only be achieved if both the surgical and prosthetic factors are considered and respected. For example, the shape and the height of the titanium base seem to be important to preserving crestal bone stability; a design that is too wide and too short gingivally can compress the bone and result in resorption (Fig 11-1).
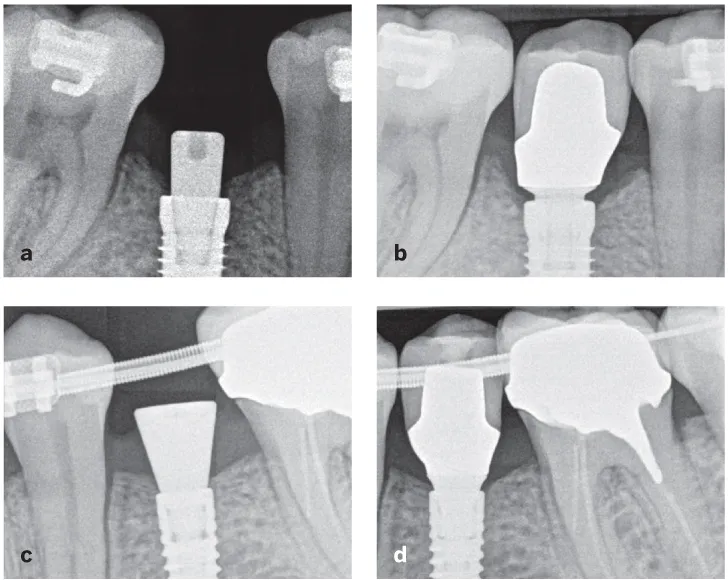
Fig 11-1 (a and b) Bone loss caused by improper selection of prosthetic components, including a restoration with an emergence profile that is too steep and too wide. This subcrestally placed implant should have been restored in a different manner. (c and d) When the prosthetic rules are respected, bone stability is maintained.
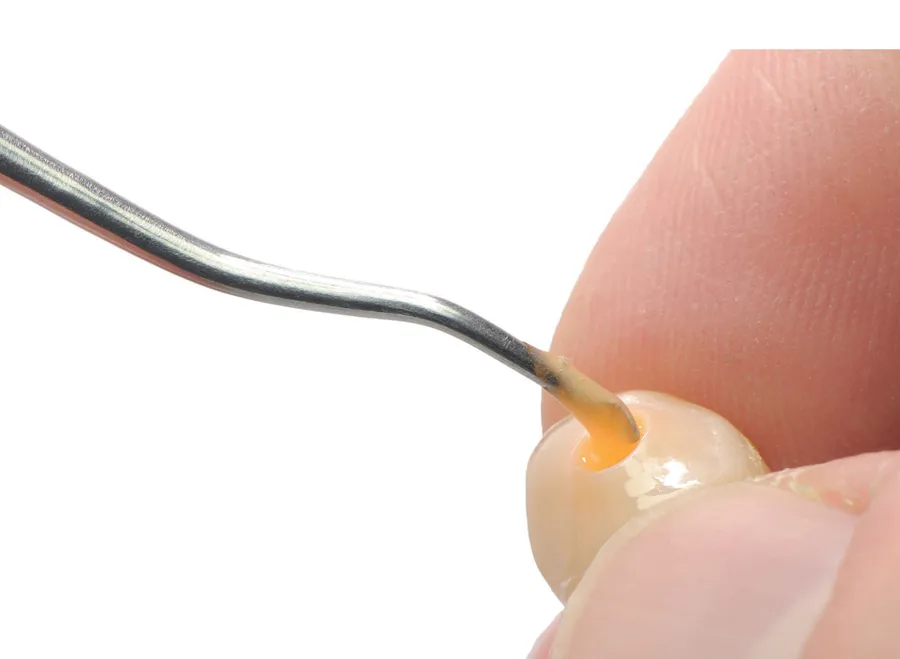
Another example of how prosthetic factors can ruin good surgical work is excess cement. For many years, dental cement used for retention of restorations was not considered a threat to crestal bone stability. However, recent research and clinical reality dictates that cement remnants should be taken very seriously.1,2 Cement has caused delayed peri-implant problems, even after many years of function (Fig 11-2).
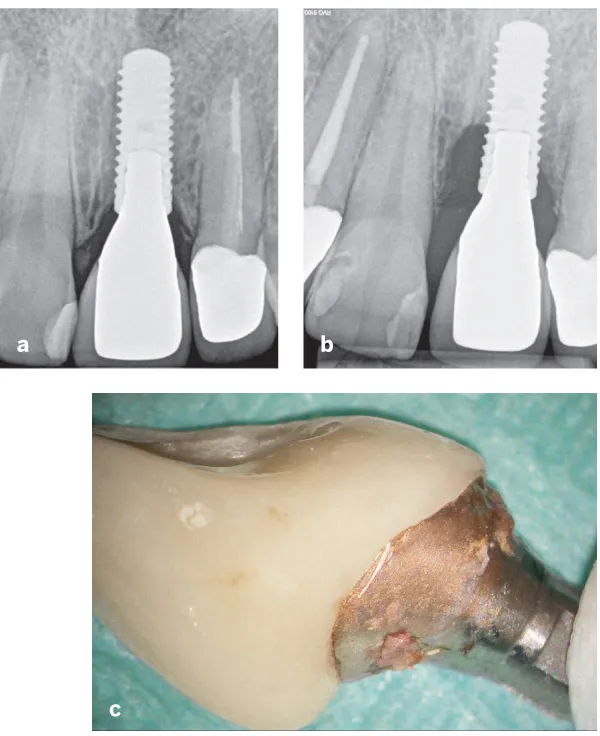
Fig 11-2 (a) Crestal bone stability of cemented implant restoration in 2009. (b) Bone stability in 2018. Bone loss is obvious, and initially the reasons for this were unknown because no cement remnants were visible on the radiograph. (c) Restoration following removal. Cement remnants not visible on the radiograph are visible on the abutment. It is also possible to see how oxidated and rough the gold abutment has become over time.
In addition, the abutment material can influence soft tissue adaptation. There have been clinical observations that tissues tend to adhere better to zirconia than to titanium or ceramics.3 This results in a better seal of peri-implant tissues and reduces the possibility of food impaction and tissue movement, which can cause unexpected inflammation or suppuration (Fig 11-3).
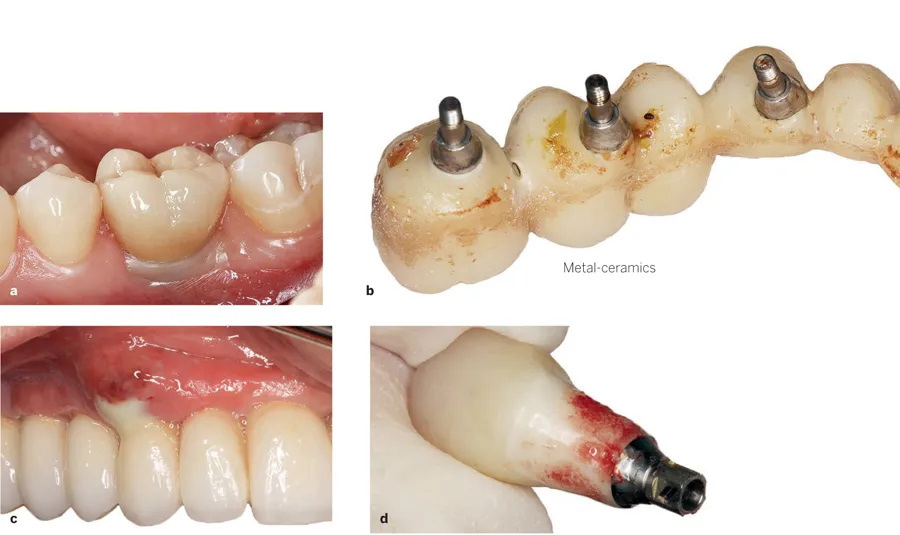
Fig 11-3 Adaptation of peri-implant tissues to different prosthetic materials. (a) Adhesion to zirconia guarantees good soft tissue conditions. (b and c) Poor adaptation of mucosa to feldspathic ceramics might result in food impaction, debris accumulation, and inflammation. (d) It is possible to observe how soft tissues adhere to the zirconia prosthetic surface as there are still remnants of soft tissue on the restoration after removal.
In fact, there are several important prosthetic factors that influence crestal bone stability, including abutment material, veneering material, and the choice of cement- or screw-retained restorations (Fig 11-4). Compared with surgical factors, there is an even greater variety of prosthetic factors that influence bone stability. For example, there are five different prosthetic material categories that can be used for implant restorations: metal, ceramics, zirconia, lithium disilicate, and others. All of these materials have their own effect on bone stability. Another example is the different types of cement that can be used for the implant crown; different cement types have diverse influences on maintaining bone stability.

Fig 11-4 (a) Abutment material. (b) Veneering material. (c) Type of retention (screw or cement). These comprise a small sample of the prosthetic factors that must be considered for zero bone loss concepts.
There are four distinct components to address to keep bone stable after the restoration process:
1. Cement- or screw-retained restoration
2. Emergence profile of the restoration
3. Subgingival implant restoration materials
4. Supragingival implant restoration materials
An important point to emphasize is that as with surgical factors, there is no single prosthetic factor that is most important for implant success: All of them are important.
For example, you can use a cemented restoration from a biocompatible material such as zirconium dioxide (Zr02) with an elegant and correct emergence profile, but if cement remnants are left, the result will not be successful. On the other hand, a metal-ceramic screw-retained restoration will eliminate the possibility of cement remnants, but lack of adhesion of soft tissues to ceramic may create a pocket that later leads to more bone loss. As with the previously described surgical factors, it is necessary to look at the whole picture.
References
1. Quaranta A, Lim ZW, Tang J, Perrotti V, Leichter J. The impact of residual subgingival cement on biological complications around dental implants: A systematic review. Implant Dent 2017;26:465–474.
2. Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of peri-implant disease: A systematic review. Clin Oral Implants Res 2017;28: 1278–1290.
3. van Brakel R, Cune MS, van Winkelhoff AJ, de Putter C, Verhoeven JW, van der Reijden W. Early bacterial colonization and soft tissue health around zirconia and titanium abutments: An in vivo study in man. Clin Oral Implants Res 2011;22:571–577.
12
CONSIDERATIONS FOR CEMENT-RETAINED RESTORATIONS
It is still unclear which option for restoring implants— cement or screw retention—is better for the patient. A systematic review conducted by Sailer et al1 in 2012 demonstrated significantly more bone loss around cemented restorations compared with screw-retained restorations. In contrast, Nissan et al2 published an article about long-term outcomes of cementversus screw-retained implant-supported partial dentures that showed a better outcome for cement-retained crowns. When there is conflicting evidence, how do you decide who is right?
One of the best answers to this question can be found in the author’s clinical experience with a split-mouth treatment situation. The patient in Fig 12-1 was treated with two dental implants, and both types of restorations were used: screw-retained in the mandible and cemented crown in the anterior maxilla. The patient was recalled for follow-up after 9 years, and the screw-retained restorations were much more successful. A breakthrough lending further credence to this finding is a 2011 study showing that it is not possible to remove cement remnants from the subgingival margins of abutments.3 Until this study was published, the position of the cementation margin was not considered a factor in the success or failure of cemented restorations. This study opened new doors for research: Before 2011, there were only a couple of studies discussing the influence of the cementation margin position on excess cement4,5; from 2011 to 2018, there have been more than 30 different papers published describing this issue. This means that the last 8 years witnessed 10 times as many studies about cement as previous decades. Clearly, the interest in this issue is quickly growing.
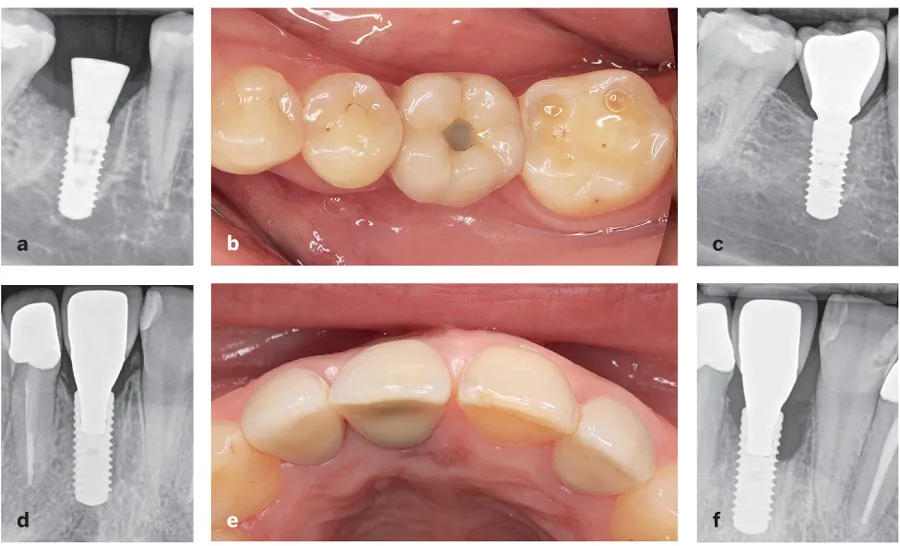
Fig 12-1 (a to c) Excellent outcome with screw-retained restorations after 9 years in function. (d to f) Peri-implantitis at a cemented restoration after the same amoun...
Table of contents
- Cover
- Half Title
- Title Page
- Dedication
- Copyright Page
- Contents
- Preface
- Acknowledgments
- Contributors
- Introduction to Zero Bone Loss Concepts
- SECTION I: Surgical Concepts
- SECTION II: Prosthetic Concepts
- Epilogue
- Index
- Backcover
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Zero Bone Loss Concepts by Tomas Linkevičius in PDF and/or ePUB format, as well as other popular books in Medicine & Dentistry. We have over one million books available in our catalogue for you to explore.