Cardiac Pacing and ICDs
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Cardiac Pacing and ICDs
About this book
The consummate guide to cardiac pacing and defibrillator therapy in a clinical setting
Designed to provide clinicians and fellows with a complete, up-to-date breakdown of current device therapies for pacing and defibrillation, Cardiac Pacing and ICDs reflects the latest developments in the device treatment of heart rhythm abnormalities. Topics ranging from essential principals to new and innovative techniques are explored in focused chapters, illustrated with full-color images, charts, and diagrams. Addressing every aspect of permanent and temporary pacing and defibrillation therapy, this invaluable resource covers patient indications, pacing mode selection, implantation and removal techniques, troubleshooting, and much more.
The seventh edition has been expanded and revised to enable clear and practical understanding of the field as it exists today. Drawing upon real-world experience and cutting-edge research, it offers accessible, systematic guidance with a clinical focus, as well as a wealth of bitesize tips and tricks. Access to a new companion website provides insightful supplementary material, complete with downloadable images and video clips of key techniques. This essential book:
- Provides an intuitive, easy-to-navigate guide to cardiac pacing techniques and devices
- Explains pacing hemodynamics in practical, clinically relevant terms
- Features simple algorithms for mode selection and device programming
- Offers details of novel pacing systems and techniques, such as leadless pacemaker and His bundle pacing.
- Covers pacemaker timing cycles, special features, and evaluation and management of pacing system malfunctions
- Summarizes indications and details implantation techniques of ICDs, including transvenous and subcutaneous systems
- Includes best practices in MRI safety, patient consultation, and remote patient follow-up
Cardiac Pacing and ICDs is an ideal resource for clinicians and fellows in cardiology and electrophysiology, those preparing for the IHRBE Examination in Devices, and any nurses, technicians, and other professionals caring for patients with implantable cardiac devices.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
CHAPTER 1
Indications for permanent cardiac pacing
Introduction
Anatomy and physiology of the conduction system
Sinus node
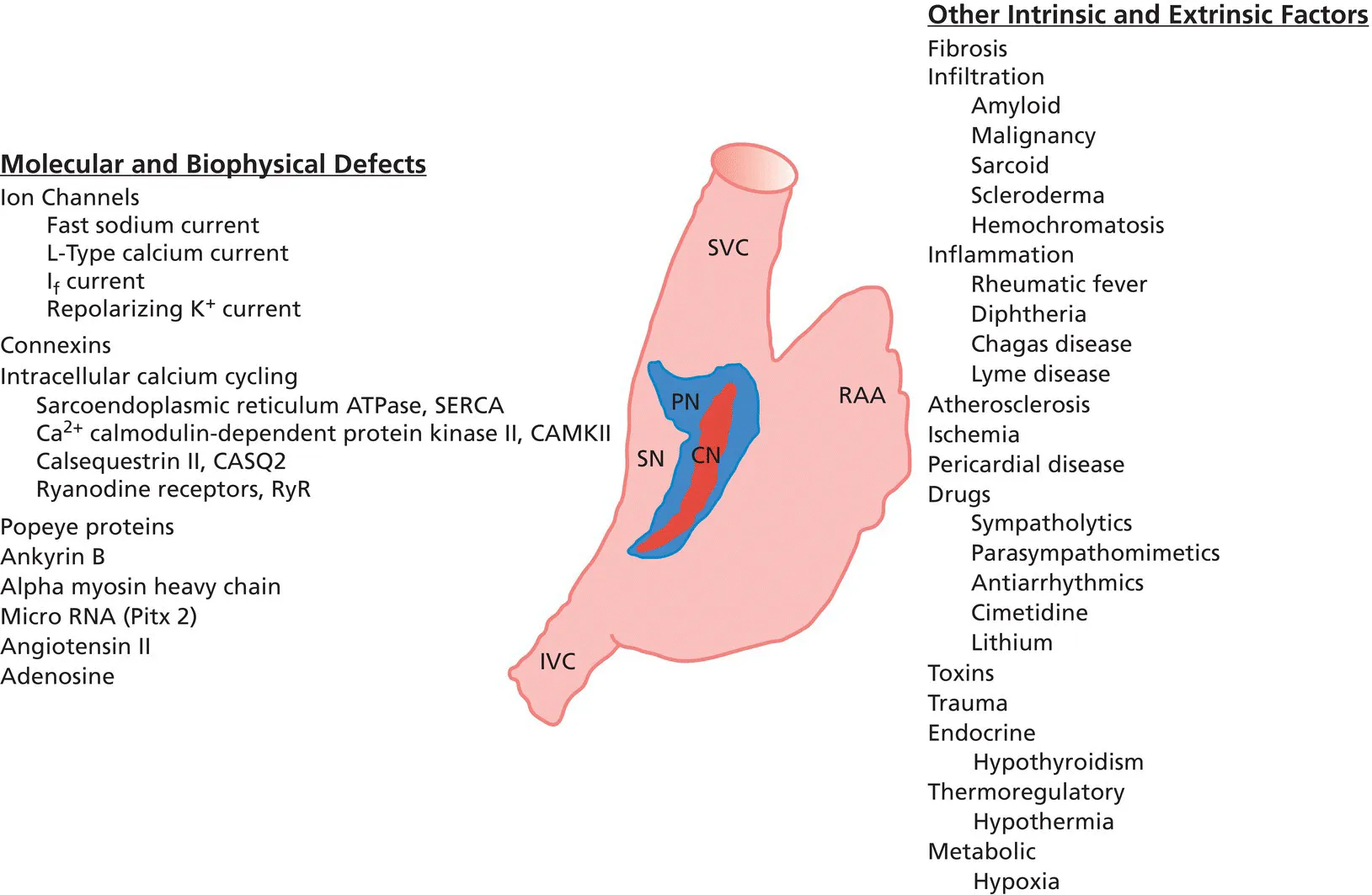
Atrioventricular node
Table of contents
- Cover
- Table of Contents
- List of Contributors
- Preface
- Acknowledgments
- CHAPTER 1: Indications for permanent cardiac pacing
- CHAPTER 2: Basics of cardiac pacing: components of pacing, defibrillation, and resynchronization therapy systems
- CHAPTER 3: Hemodynamics of cardiac pacing and pacing mode selection
- CHAPTER 4: Temporary cardiac pacing
- CHAPTER 5: Techniques of pacemaker and ICD implantation and removal
- CHAPTER 6: Pacemaker timing cycles and special features
- CHAPTER 7: Evaluation, troubleshooting, and management of pacing system malfunctions
- CHAPTER 8: The implantable cardioverter–defibrillator
- CHAPTER 9: Cardiac resynchronization therapy
- CHAPTER 10: ICD follow‐up and troubleshooting
- CHAPTER 11: Follow‐up of the patient with a CIED
- Index
- End User License Agreement
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app