- 627 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Imaging of the Cardiovascular System, Thorax, and Abdomen
About this book
Magnetic resonance imaging (MRI) is a technique used in biomedical imaging and radiology to visualize internal structures of the body. Because MRI provides excellent contrast between different soft tissues, the technique is especially useful for diagnostic imaging of the brain, muscles, and heart.
In the past 20 years, MRI technology has improved significantly with the introduction of systems up to 7 Tesla (7 T) and with the development of numerous post-processing algorithms such as diffusion tensor imaging (DTI), functional MRI (fMRI), and spectroscopic imaging. From these developments, the diagnostic potentialities of MRI have improved impressively with an exceptional spatial resolution and the possibility of analyzing the morphology and function of several kinds of pathology.
Given these exciting developments, the Magnetic Resonance Imaging Handbook: Imaging of the Cardiovascular System, Thorax, and Abdomen is a timely addition to the growing body of literature in the field. Offering comprehensive coverage of cutting-edge imaging modalities, this book:
- Discusses MRI of the heart, blood vessels, lungs, breasts, diaphragm, liver, gallbladder, spleen, pancreas, adrenal glands, and gastrointestinal tract
- Explains how MRI can be used in vascular, posttraumatic, postsurgical, and computer-aided diagnostic (CAD) applications
- Highlights each organ's anatomy and pathological processes with high-quality images
- Examines the protocols and potentialities of advanced MRI scanners such as 7 T systems
- Includes extensive references at the end of each chapter to enhance further study
Thus, the Magnetic Resonance Imaging Handbook: Imaging of the Cardiovascular System, Thorax, and Abdomen provides radiologists and imaging specialists with a valuable, state-of-the-art reference on MRI.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1
Coronary and Perfusion Imaging with Cardiovascular Magnetic Resonance: Current State of the Art
CONTENTS
1.1 Introduction
1.2 Technical Challenges and General Imaging Strategies for Coronary CMR
1.2.1 Compensation of Cardiac Motion: ECG Triggering
1.2.2 Compensation of Respiratory Motion: Navigator
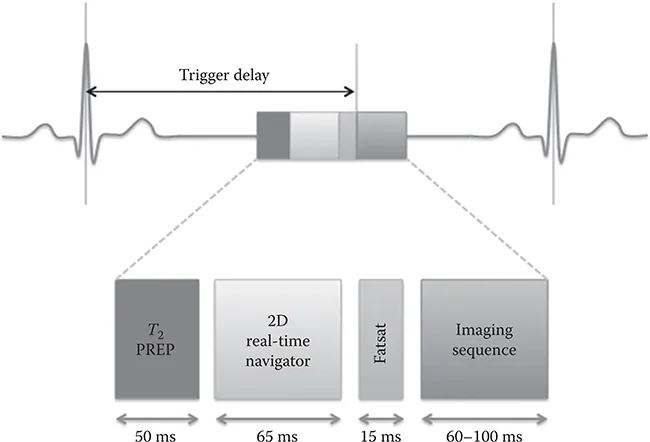
Schematic representation of pulse sequence elements for MRA. Image acquisition is performed in mid-diastole after a trigger delay from the R wave of the ECG. The imaging block is preceded by a contrast-enhancing spin preparation (T2 PREP), a 2D selective real-time navigator pulse for respiratory motion compensation, and a frequency-selective fat-suppression prepulse (FATSAT). These sequence blocks are repeated with every heart cycle. (Adapted from Botnar, R.M. et al., Circulation, 99, 3139–3148, 1999. With permission.)
Comparison between Systolic and Diastolic Coronary CMR
Diastolic Resting Period | Systolic Resting Period |
Advantages Longer acquisition window (~100–125 ms/heartbeat) Higher blood flow (higher signal in gradient echo sequences) | Advantages Less sensitive to heart rate variability Larger diameter of the venous vessels |
Disadvantage Higher sensitivity to heart rate variability | Disadvantage Shorter acquisition window (~50 ms/heartbeat) |
1.2.3 Coronary Artery Imaging
1.2.3.1 Sequences
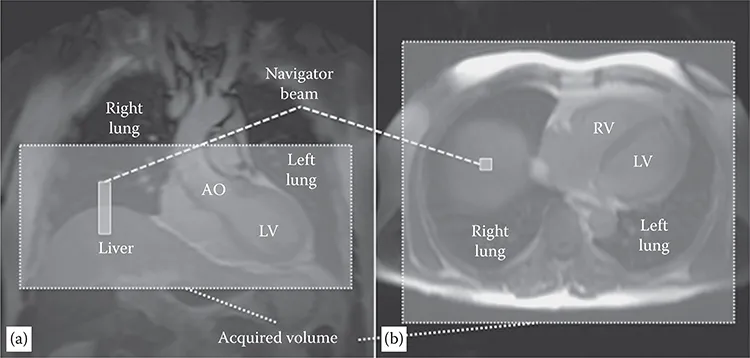
Planning of the navigator and of the whole heart imaging volume from coronal (a) and axial (b) scout images. A pencil beam one-dimensional navigator is posit...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Dedication
- Table of Contents
- Preface
- Acknowledgments
- Editor
- Contributors
- 1. Coronary and Perfusion Imaging with Cardiovascular Magnetic Resonance: Current State of the Art
- 2. Imaging of the Heart: Myocardial Imaging
- 3. Computed Topography/Magnetic Resonance Imaging of Pericardial Disease
- 4. Vascular Imaging of the Head and Neck
- 5. Magnetic Resonance Imaging: Aorta and Splanchnic Vessels
- 6. Peripheral Magnetic Resonance Angiography
- 7. Magnetic Resonance Venography
- 8. Vascular Malformations
- 9. Four-Dimensional Flow Imaging
- 10. Magnetic Resonance Imaging for Trachea, Bronchi, and Lung
- 11. Clinical Magnetic Resonance Imaging Applications for the Lung
- 12. Pleura and Diaphragm
- 13. Functional Magnetic Resonance Imaging of the Lung and Pulmonary Vasculature
- 14. Breast MRI
- 15. Liver: Technique and Diffuse Pathology
- 16. Liver: Focal Pathology
- 17. Gallbladder
- 18. Magnetic Resonance Imaging of Biliary Tract
- 19. Update in Magnetic Resonance Imaging of the Spleen
- 20. Pancreas
- 21. The Adrenal Gland
- 22. Diseases of the Upper Gastrointestinal Tract and Small Bowel
- 23. MRI of the Retroperitoneum
- 24. Abdominal Wall and Hernias
- 25. Diseases of the Colon and Rectum
- 26. Posttraumatic and Postsurgical Abdomen
- Index