- 144 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Nurses' Clinical Decision Making
About this book
This work includes a foreword by Carl Thompson, Senior Research Fellow, Department of Health Sciences, University of York. This inspiring text offers guidance and innovative ideas for teaching and learning. It explains how nurses make clinical decisions through the development of narratives, and how, using narratives, nurses gain a far more intimate knowledge of the patient than doctors can. The book considers service delivery around patients, renegotiation of professional roles of medical staff and their boundaries of responsibility and authority. "Nurses' Clinical Decision Making" will appeal to all undergraduate and postgraduate students of nursing, registered nurses and nurse managers. Nurse educators, hospital managers, doctors and healthcare risk managers will also find the information contained here invaluable. 'If nurses are decision-makers how can their role and practice be explained? Can decision-making be taught and are there different levels of decision-making skill? If so, how can expert decision-makers be recognised? These are just some of the pertinent questions that need to be asked if we are to recognise and understand the centrality of clinical decision-making in nursing practice. Clinical work is complex and takes place in a complex environment that centres around individuals who themselves are physically, socially and spiritually complex. Clinical work also involves multiple participants (nurses, doctors, patients, physiotherapists, occupational therapists, pharmacists to name a few) who in the course of a days work can make scores of decisions.' - Russell Gurbutt, in the Preface.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Topic
MedicineChapter 1
Setting the scene: the clinical landscape of decision making
Introduction • Raising questions • Origins and developments • Knowledge and decision making • Rules and decision making • Assistants in medical decision making • Breakout: developing nurse decision making • Nursing models and decision making • Decision-making enquiry about different types of nurse • Decision-making enquiry about different types of decision • complexity and nursing • Decision-making enquiry about process • Decision-making enquiry and the use of different terminology • Decision making and problem solving • Decision-making outcomes • Decision-making process • Theoretical explanations • Decision-making context • The clinical landscape • Conclusion • Stop and think
Introduction
If nurses are decision makers, how can their role and practice be explained? Can decision making be taught and are there different levels of decision-making skill? If so, how can expert decision makers be recognised? These are just some of the pertinent questions that need to be asked if we are to recognise and understand the centrality of clinical decision making in nursing practice.
This chapter introduces nurses’ decision making. At the outset it considers two clinical incidents which highlight a range of questions that real-world practice raises about decision making. Then selected developments in nurses’ decision-making practice are introduced to highlight how the role has developed and subsequently moved away from its medically dominated origins. The contribution of nursing models to the construction of professional identity is used to mark a shift in focus towards nursing decisions. Different types of nurse and nursing decision are explored along with the processes that they use and the descriptive terminology employed. Links between decision making and problem solving are discussed along with explanations of decision outcomes. Different theoretical explanations of the whole process are identified before returning to contemporary accounts of the context of nurses’ decision making and its influence on the process.
Throughout the chapter the intention is to show that nurses have a decision-making role and that their practice includes a range of elements (e.g. information seeking, processing, knowledge, outcome). Although theoretical accounts draw these elements together, a unifying theory of decision making does not exist. Figure 1.1 shows how key areas of decision making can be drawn together as a reference to consider where decision-making enquiry has been and can be directed. It incorporates the decision maker(s), decision process, decision outcome and decision-making context. Now let us turn our attention to questions about decision making that can be generated through real-world practice.
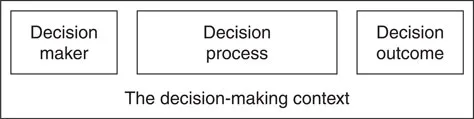
Figure 1.1 A model showing key areas of decision making. The model consists of a decision maker, a decision process, a decision outcome and a decision-making context.
Raising questions
Think about what it is like to go into hospital as a patient, to be drawn into the daily business of a complex service provided by numerous people. These include nurses, therapists, chaplains, doctors, porters, laboratory technicians, chefs, cleaning staff, administrators and managers, to name just a few. As a patient, you have expectations about the service that you think you need, an understanding of the extent of your participation in decision making, and a degree of trust in the decisions that healthcare staff make about your care and treatment. Incidents occur that raise concerns – perhaps a missed medication, overlooked requests or staff seeming to be too busy to stop and chat. A catalogue of small events can lead to a perception that decisions are being made about you but not with you. Some might actually contribute to harm rather than good. Why would this be and how can it be explained? Who is making decisions and, perhaps more importantly, are some decisions being overlooked? Clinical incidents occur in health service delivery. The two scenarios that follow raise interesting questions.1
During an evening shift on an understaffed 36-bed stroke rehabilitation ward the nurse in charge was commencing a drug round. She had two care assistants on duty who were busy attending to patients as they worked their way down the ward. The staff nurse glanced down the ward and saw a patient trying to roll over in his bed. She called to him to stop as she anticipated (correctly) that he would fall on to the floor. There was not time to get to his bed, and as he fell out of bed on to the floor, there was an audible crack. His femur had fractured. Three days later he died.
This incident raised many questions. Who had assessed the patient’s needs and planned his care? Had a care plan been devised that addressed the need to maintain a safe environment? Should rehabilitating patients be expected to take risks (as people in normal health do) and should it be accepted that falls can happen during the process of regaining independence? Had a decision not been made that ultimately contributed to the patient’s death? Sometimes examining practice generates far more questions than answers. Fortunately, not all clinical incidents are as serious as this one. The next story is about a complaint which implied that nurses were omitting to provide adequate care for a patient. At best it was an organisational or resource management problem and at worst an allegation of negligence.
A stroke patient had been convalescing for several weeks on a busy 28-bed rehabilitation ward. The ward was short staffed and the three or four staff on duty on each shift (registered nurses and care assistants) were involved in physically demanding work. The most that they could achieve with each patient during a shift was to attend to their daily needs (such as washing, dressing, feeding and toileting) and help with some physical therapy. A complaint was made by the patient’s relative in which it was claimed that the rehabilitation process was too slow. This was attributed to deficits in the nursing care provided. A local enquiry took place to investigate the complaint and provide a written response.
The investigation included discussions with the ward team about their care decisions and examination of their records. Neither of these sources of enquiry provided a satisfactory answer about what was planned and provided, nor did they explain how and why decisions had been made or, as was alleged, overlooked. However, this investigation did generate interest in proposing a study of how registered nurses made clinical decisions. The findings of that study (of nurses in four NHS general medical wards) are used to explain different features of decision making, decision makers and their practice in the chapters of this book. The aftermath of the response to the complaint generated several questions about nurses’ decision making. For example, could nurses recognise the range and volume of decisions made in the course of their practice? Could they recognise and explain their decision making? Furthermore, if this could be explained, why did their care records not clearly demonstrate this? Both scenarios require questioning to go beyond asking what happened and who made decisions. The decision-making processes, context, participants and their resources are just some of the factors that need to be considered when seeking to find out why and how decisions are made.
Back in the ward a learning opportunity was lost. The pace of work gave little respite to seriously examine practice that at times was on a merry-go-round of trying to match limited resources with ever-increasing demand. There is a saying that ‘if we do what we have always done then we will get what we have always got’. How apt – but we need to find a way of stepping aside for a while to examine what it is that nurses do and to learn about their clinical decision making. Why is this? It is so that nurses can know how central decision making is to their role and are able to articulate what it is that they do.
Given that there are often more questions than answers, any simple explanations of decision making seem inadequate. Indeed, as was intimated earlier, hospitals are complex organisations involving many people, many interactions, and different processes and information sources. It is not surprising that real world clinical decision making should be regarded as complex. Some scene setting follows about the development of nurses as decision makers and their decision-making practice.
Origins and developments
There are different claims about the origin of nurse decision-making enquiry. These have included the game theory,2 which dealt with decision making under uncertain conditions and has been linked to applications in economics and ...
Table of contents
- Cover
- Title Page
- Copyright Page
- Table of Contents
- Foreword
- Preface
- About the author
- Acknowledgements
- A guide to using this book
- 1 Setting the scene: the clinical landscape of decision making
- 2 Making clinical decisions: a model of nurses’ decision making
- 3 The narratives that nurses generate: ways of knowing the patient
- 4 Demonstrating narratives: differences between verbal and written narratives
- 5 The games nurses play: making narratives known to doctors
- 6 Narratives and expert decision makers: creating and using narratives
- 7 Nurses as decision makers: where next?
- Appendix: Suggested lesson plans
- Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Nurses' Clinical Decision Making by Russell Gurbutt in PDF and/or ePUB format, as well as other popular books in Medicine & Alternative & Complementary Medicine. We have over one million books available in our catalogue for you to explore.