eBook - ePub
An Atlas of Gynecologic Oncology
Investigation and Surgery, Fourth Edition
- 347 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
An Atlas of Gynecologic Oncology
Investigation and Surgery, Fourth Edition
About this book
The latest edition of An Atlas of Gynecologic Oncology continues its coverage of the innovative techniques in investigation and surgery on the brink of becoming established as part of the gynecologic surgeon's repertoire, now including the exciting developments in uterine transplantation.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access An Atlas of Gynecologic Oncology by J. Richard Smith, Giuseppe Del Priore, Robert L. Coleman, John M. Monaghan, J. Richard Smith,Giuseppe Del Priore,Robert L. Coleman,John M. Monaghan in PDF and/or ePUB format, as well as other popular books in Medicine & Gynecology, Obstetrics & Midwifery. We have over one million books available in our catalogue for you to explore.
Information
1Introduction: Preparing a patient for surgery
Srdjan Saso, Benjamin P. Jones, J. Richard Smith, and Giuseppe Del Priore
Introduction
This chapter reviews three specific areas relevant to virtually all surgical procedures and surgeons: infection prophylaxis; deep venous thrombosis (DVT) prophylaxis; and universal precautions. Universal precautions facilitate the protection of surgeons and their assistants, medical and nursing, and patients. Preoperative and postoperative checklists now form a vital part of risk reduction. James Reason, PhD, formulated the “Swiss cheese theory” of risk. This is based on a piece of Swiss cheese with holes in it. The more slices one puts in the cheese, the less likely it is that an arrow could fly through the holes, and thus the holes are less likely to tally with each other. Therefore the more layers of checking that one puts in pre- and postoperatively, the less likely it is that the antibiotic prophylaxis will be forgotten or the postoperative DVT prophylaxis will not be given. A simple checklist is shown in Figure 1.1. The purpose of any such checklist is to systematically and efficiently ensure that all operative conditions are optimal with respect to patient safety. The hope is that by completing such a checklist, the lives and well-being of surgical and thus gynecological patients will be minimized as errors in patient identity, site, and type of procedure are avoided completely.
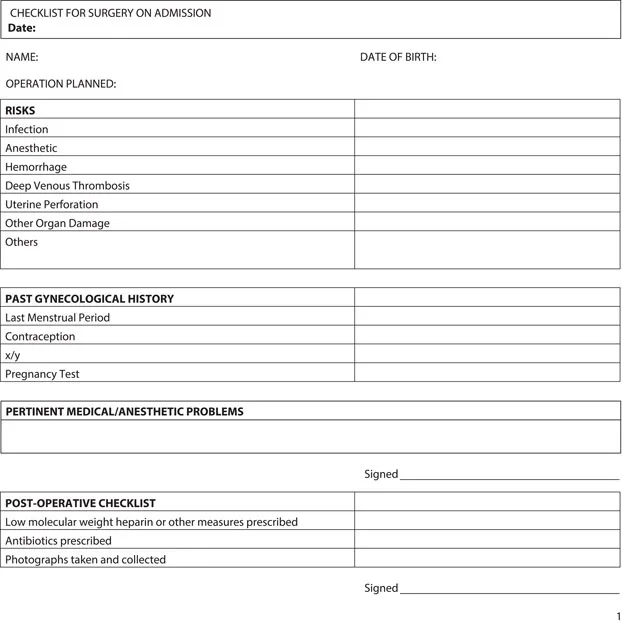
Figure 1.1Checklist for surgery on admission.
More well known is the surgical checklist published by the World Health Organization (WHO) in 2008 in order to increase the safety of patients undergoing surgery. It is officially known as the WHO Surgical Safety Checklist and Implementation Manual. It is now used in general surgery, orthopedics, and obstetrics and gynecology. The operation is divided into three distinct phases by the checklist. Each phase corresponds to one of the following periods: (a) before the induction of anesthesia, (b) before the skin incision (known as “time out”), and (c) before the patient leaves the operating facility (known as “sign out”). A “checklist coordinator” must confirm that the surgical team has completed a phase before moving on to the next. Only when all three phases have been completed can the procedure commence.
Phase I: Before Induction of Anesthesia. The following must be confirmed first: patient identity, site of operation, procedure to be carried out, and consent. Type of anesthetic required, allergies (if any), and expected blood loss should be discussed. Phase I is to be completed by the anesthetist.
Phase II: Time Out. This refers to a process before the first incision where all present in the room must introduce themselves by name and role. The patient name and the planned procedure are then confirmed as well as any surgical or anesthetic critical events that may occur. The need for antibiotics, DVT prophylaxis, and imaging is highlighted. Phase II is to be completed by the surgeon and anesthetist.
Phase III: Sign Out. The final phase is performed before the patient leaves the operating room. Swabs, instruments, and needle counts are done, the equipment is checked (including disposables), and the specimens are checked as properly labeled. The postoperative recovery process is discussed. Phase III is to be completed by the surgeon or nursing staff.
Figure 1.1 shows the checklist on admission for surgery.
Thromboembolic Disease
Venous thromboembolic disease (VTE) is a significant cause of morbidity and mortality in gynecologic oncology patients. If sensitive methods of detection are employed and no preventive measures are taken, at least 20% and as many as 70% of gynecologic cancer patients may have some evidence of thrombosis. In certain situations, such as with a long-term indwelling venous catheter of the upper extremity, nearly all patients will have some degree of VTE, though it may not be clinically significant. On the other hand, lower extremity VTE has a much more certain and clinically significant natural history. Venous thromboses below the knee may spread to the upper leg in approximately 10% to 30% of cases or resolve spontaneously in approximately 30%. Once the disease has reached the proximal leg, the risk of pulmonary embolism (PE) increases from less than 5% for isolated below-the-knee VTE to up to 50% for proximal VTE. The mortality rate for an undiagnosed PE is high. Up to two-thirds of patients who die from PE do so in the first 30 minutes after diagnosis.
Early recognition and effective treatment can reduce this mortality. However, postoperative VTE is still a leading cause of death in gynecologic oncology patients. In the past, it was clear that only one-third of hospitalized high-risk patients received appropriate prophylaxis; this figure has now much improved, particularly with the use of checklists. Risk factors are listed in Table 1.1 (NICE 2015).
Table 1.1Risk Factors for VTE (NICE 2015)
|
Prevention and Risk Assessment
Patients may be considered for prevention of VTE based on their clinical risk category. Laboratory tests such as euglobulin lysis time do correlate with the risk of VTE but are no more helpful than clinical risk assessment in selecting patients for prophylaxis. Low-risk patients are young (less than 40 years old), undergoing short operative procedures (less than 1 hour), and do not have coexisting morbid conditions such as malignancy or obesity that would elevate the risk of VTE. Moderate-risk patients include those undergoing longer procedures, older or obese patients, and patients having pelvic surgery. High-risk patients include otherwise moderate-risk patients who have cancer and those with a previous history of VTE. Positioning for vaginal surgery lowers the risk of VTE when compared with the abdominal approach.
All patients should be assessed for risk of bleeding before being offered pharmacological VTE prophylaxis. This should not be offered to patients with any of the risk factors for bleeding shown in Table 1.2, unless the risk of VTE outweighs the risk of bleeding. Patients should be advised to consider stopping estrogen-containing oral contraceptives or hormone replacement therapy 4 weeks before elective surgery. If stopped, advice must be provided on alternative contraceptive methods (NICE 2015). All patients should have some form of VTE prevention. This first begins with risk reduction. Patients should not become dehydrated unless clinically indicated. They must mobilize as soon as possible. Aspirin or other antiplatelet agents should not be considered as adequate prophylaxis for VTE. Finally, temporary inferior vena caval filters should be offered to patients who are at very high risk of VTE (such as patients with a previous VTE event or an active malignancy) and for whom mechanical and pharmacological VTE prophylaxis are contraindicated (NICE 2015).
Table 1.2Risk of Bleeding (NICE 2015)
|
Table of contents
- Cover
- Half Title Page
- Title Page
- Copyright Page
- Dedication
- Contents
- Contributors
- Preface
- Acknowledgments
- In Memoriam: Andrew D. Lawson
- Chapter 1 Introduction: Preparing a patient for surgery
- Chapter 2 Preoperative workup
- Chapter 3 Complications
- Chapter 4 Anatomy
- Chapter 5 Cross-sectional and molecular imaging
- Chapter 6 Sigmoidoscopy, cystoscopy, and stenting
- Chapter 7 Tumor markers
- Chapter 8 Cone biopsy
- Chapter 9 Radical abdominal hysterectomy
- Chapter 10 Laparoscopically assisted vaginal radical hysterectomy
- Chapter 11 Radical vaginal trachelectomy
- Chapter 12 Radical abdominal trachelectomy
- Chapter 13 Central recurrent cervical cancer: The role of exenterative surgery
- Chapter 14 Total mesometrial resection
- Chapter 15 Laterally extended endopelvic resection
- Chapter 16 Vaginectomy
- Chapter 17 Radical vulvar surgery
- Chapter 18 Sentinel lymph node biopsy
- Chapter 19 Ovarian tissue cryopreservation and transplantation
- Chapter 20 Uterine transplantation and lessons from transplant surgery
- Chapter 21 Epithelial ovarian cancer
- Chapter 22 Upper abdominal cytoreduction for advanced ovarian cancers
- Chapter 23 Extraperitoneal approach to infrarenal, inframesenteric, and pelvic lymphadenectomies
- Chapter 24 Vascular access and implantable vascular and peritoneal access devices
- Chapter 25 Surgical management of trophoblastic disease
- Chapter 26 Laparoscopy
- Chapter 27 Humidification during surgery: Benefits of using humidified gas during laparoscopic and open surgery
- Chapter 28 Robotic surgery
- Chapter 29 Gastrointestinal surgery in gynecologic oncology
- Chapter 30 Urologic procedures
- Chapter 31 Fistula repair
- Chapter 32 Treatment of vascular defects and injuries
- Chapter 33 Plastic reconstructive procedures
- Chapter 34 Additional plastic surgery procedures
- Chapter 35 Fat transfer: Applications in gynecology
- Chapter 36 Surgical management of postpartum hemorrhage
- Chapter 37 Brachytherapy
- Chapter 38 Innovative methods to teach and train minimally invasive surgery
- Chapter 39 Meta-analysis of survival data
- Chapter 40 Pain management
- Chapter 41 Palliative care
- Chapter 42 Doctor–patient communication
- Index