![]()
Chapter 1
What is an OSCE?
‘Happiness comes when we test our skills towards some meaningful purpose.’
JOHN STOSSEL, Journalist (born 1947)
Aims
At the end of this chapter, you should:
- Understand what the acronym OSCE stands for
- Understand the key features of an OSCE
- Know how OSCEs can be used to assess clinical skill competency
- Recognise the different types of OSCEs used in nursing and midwifery education
This chapter aims to equip you with the knowledge and understanding of what an OSCE is, its key features, and how it might be used to assess your competency in a range of clinical skills relevant to nursing and midwifery practice.
So what is an OSCE?
Perhaps you have just discovered that the type of assessment for the course you are studying is an OSCE. Understandably, this may have left you feeling a little apprehensive or unsure of what to expect. By the very fact that you are reading this book, you will know that the course you are studying has a clinical component. For example, it may focus on the clinical aspects integral to the provision of care for a specific patient population, such as pregnant women, or those with a particular disease, such as diabetes or asthma. Alternatively, it may be closely linked to an area of practice that requires a specific set of skills such as wound care, tissue viability or orthopaedic nursing. As such, because of the clinical focus of the course, traditional, more conventional types of assessment, such as a written exam or essay, may not be appropriate.
You may have heard other students talking about OSCEs, but perhaps you are still unclear as to what the term ‘OSCE’ means or what it actually involves. To answer these questions, let’s start at the beginning.
Activity 1.1
Jot down some ideas about what you think an OSCE is. You may like to reflect on discussions you have had with other students or colleagues or on any information you have read about OSCEs.
The OSCE acronym
The term ‘OSCE’ is an acronym that stands for Objective Structured Clinical Examination and throughout the literature there are many different definitions. Perhaps one of the clearest is that proposed by Watson (2002, p. 424) who described the OSCE as an exam whereby ‘students demonstrate their competence under a variety of simulated conditions’.
In other words, OSCEs are examinations in which the student is required to perform specific skills and behaviours in a simulated clinical or patient care environment. During an OSCE the examiner will assess your performance with regard to four distinct elements. These include the knowledge and understanding underpinning the skill (K); the motor or technical aspects of the skill (M); the affective aspects (A), i.e., the professional attitude associated with the performance; and structure (S), i.e., how you approach the skill in terms of being systematic, logical and organised. A simple acronym that can help you to remember these components is KMAS (Knowledge, Motor skill, Attitude, Structure). We will be discussing each of these components in greater detail later in Chapter 4.
OSCEs are not a new type of assessment. In fact, they have been used in medical education for several decades and have now become a widely accepted method of assessing clinical competence in nursing and midwifery education in the UK and in many other countries throughout the world (Rushforth 2007).
To find out more about this unique type of assessment, we will now look at each component of the OSCE acronym.
Objective (O)
‘O’ in the word OSCE stands for objective and objectivity is a defining feature of this type of assessment.
By the nature of their role, assessors have the responsibility of making professional judgements about the performance of students whom they are assessing. Within the context of nursing and midwifery, the assessor is required to make decisions based on two key judgements:
- The extent to which a student has met the learning outcomes and standards of the particular course or subject that is being examined.
- Whether the student has demonstrated the level of competency that is expected (Stuart 2006) and, consequently, whether the student is able to practice safely in the clinical setting.
As with all other forms of assessments, the OSCE process needs to be as transparent as possible. The OSCE is designed to achieve transparency by minimising potential bias.
But this is not as simple as it might sound. If you think for a moment about clinical practice and what you have seen while working in the practice environment, you will recognise that most practitioners have a preferred way of doing something. For example, some nurses might like to set up a sterile field in preparation for a wound dressing in a particular way, while still making sure that the key principles of asepsis are maintained. Likewise, you may have seen a colleague make a hospital bed in a slightly different way to how you or other nurses like to make it. For example, they may like to position the pillows facing away from the door while another colleague may be concerned about folding the bedspread in a specific way. Regardless of this, it is almost certain that the key principles underlying both techniques used for bedmaking are the same.
Generally, such idiosyncrasies are not problematic. However, if an examiner had a specific way of assessing student performance in accordance with her own particular likes, dislikes or habits, this could cause difficulties in terms of equity and consistency, especially if there were more than one examiner assessing the same skill. Problems would arise if students were not assessed objectively on their competence but instead on how well their performance complied with the examiner’s likes and dislikes. You can see that if this were to happen, the assessment process would not be fair. In fact, it could be considered biased towards the examiner! Therefore, it is very important that the clinical exam is free from any prejudice or bias. In other words, it needs to be objective.
So how is this objectivity achieved in an OSCE?
Structured (S)
The letter ‘S’ stands for structure. To achieve objectivity in the assessment of competency, a clinical skill or procedure is typically broken down into component parts in a very structured way.
Imagine teaching someone how to bake a cake. Typically, you would follow a recipe and go through the various components step by step. Similarly, if you needed to teach a junior nurse or student midwife a clinical skill, it is likely that, as part of this process, you would break down the skill into its component parts. Not only would this help you to teach the skill, but it would also help the student to learn it. In fact, you may even do this without realising it.
Over to you!
Activity 1.2
Take a few minutes to reflect on how you would teach a student nurse or midwife to measure a radial pulse. Jot down some notes below.
Did your answer contain the following points?
- Explain the procedure to the student and check that they have the necessary equipment to take a radial pulse, including a watch with a second hand and an observation chart.
- Explain the importance of universal precautions and hand hygiene prior to performing any clinical skill, and ensure that the student’s hands have been decontaminated.
- Explain the importance of obtaining consent from the patient prior to measuring the pulse.
- Show the student where to feel for a radial pulse on the patient’s wrist, and how, by using the first and second fingers, to locate and feel the pulse.
- Demonstrate to the student how to count the number of beats for a full minute and take particular note of the rate, rhythm and strength of the pulse.
As you can see, the clinical skill of measuring a pulse has been broken down into key parts to facilitate both teaching and learning, to ensure that it is undertaken both safely and competently, and that nothing is missed.
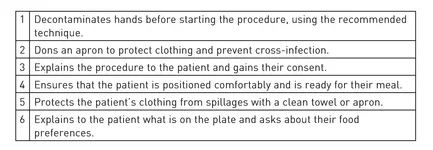
When planning for the OSCE, a team of course lecturers will spend time considering in detail each of the skills that will be examined. Each skill will be broken down into its component parts, and marking criteria, in the form of a checklist, will be developed. Essentially, this is a list of the key components of the skill that the student should perform in order to demonstrate that he is competent, safe and thorough. For example, in the following excerpt from a marking checklist, the key components inherent to the skill of feeding a dependent patient have been identified.
During the examination the assessor will use the checklist to mark each student’s performance. This is typically done by observing if each part of the skill ...