![]()
Chapter 1
The New Reality: Multifarious Caseloads
The substance abuse therapist and the mental health therapist both have a similar problem. The substance abuse therapist has clients who, in addition to having a substance use disorder, also have symptoms of other mental health disorders. The mental health therapist, likewise, has clients with substance use problems as well as other mental health disorders. However, neither type of therapist is trained to treat both types of disorders, and they tend to work in agencies that are mandated to treat just one type of disorder. The purpose of this chapter is to describe the composition of multifarious caseloads and present treatment methods and intervention strategies that can be used with clients who have multiple disorders.
PREVALENCE OF CO-OCCURRING DISORDERS
Numerous studies of substance abuse and mental health treatment populations and two major studies of the general population document significant rates of co-occurrence of substance use with certain other mental disorders. Studies of substance abuse treatment populations have found 60 percent or greater co-occurrence rates when personality disorders are included (Nace, 1989; Powell et al., 1982; Ross, Glaser, and Germanson, 1988; Westerman, Myers, and Harding, 1980); studies of mental health treatment populations have found co-occurrence rates of 40 to 50 percent (Ananth, 1989; Caton et al., 1989; Drake and Wallach, 1989; Ridgely, Goldman, and Talbott, 1986). Regier et al. (1990) presented the first major study of co-occurrence of substance use and mental disorders in the general population. They examined the National Institute of Mental Health’s Epidemiologic Catchment Area (ECA) study and found that: 29 percent of individuals with a mental disorder also had a substance use disorder; 37 percent of individuals with an alcohol disorder also had a mental disorder; and 53 percent of individuals with a drug disorder other than alcohol also had a mental disorder. They also found that individuals with co-occurring disorders were twice as likely to be in treatment for at least one of their disorders. The National Longitudinal Alcohol Epidemiologic Survey (NLAES), sponsored by the National Institute of Alcohol Abuse and Alcoholism (NIAAA), also found that individuals with alcohol and co-occurring mental disorders were much more likely to be in treatment than individuals with just alcohol disorders (Onken et al., 1997). The results of the National Comorbidity Survey reported by Kessler et al. (1994) found that 51 percent of individuals with a mental disorder also experienced a substance use disorder during their lifetime, while 41 to 66 percent of individuals with a substance use disorder experienced a mental disorder sometime in their lives. Those with alcohol abuse disorders had the lowest level of co-occurrence, and individuals with drug dependency disorders experienced the greatest co-occurrence. This study also found that individuals with dependency and co-occurring mental disorders were much more likely to be in treatment than individuals with just one disorder.
TYPES OF CLIENTS FOUND IN A MULTIFARIOUS CASELOAD
Although the substance abuse therapist’s caseload normally consists of individuals with mental disorders that only somewhat impact their ability to function independently in the community (such as dysthymia, social anxiety, or antisocial personality disorder), an occasional case will present with a major mood or psychotic disorder. The mental health therapist, on the other hand, normally works with individuals with major mental illnesses who abuse substances, but she too will treat a client with a serious substance dependence disorder. Hence the first task for both the mental health therapist and the substance abuse therapist is to take a larger view of their varied caseloads for the purpose of developing similar treatment strategies for similar clients. Multifarious caseloads for substance abuse and mental health therapists can be divided into five broad categories:
1. Individuals with mental health (MH) disorders only
2. Individuals with substance abuse (SA) disorders only
3. Individuals with a substance abuse disorder and a mental disorder
4. Individuals with a substance use disorder and a personality disorder
5. Individuals with a substance use disorder, a mental disorder, and a personality disorder
ESSENTIAL PHILOSOPHICAL VIEW
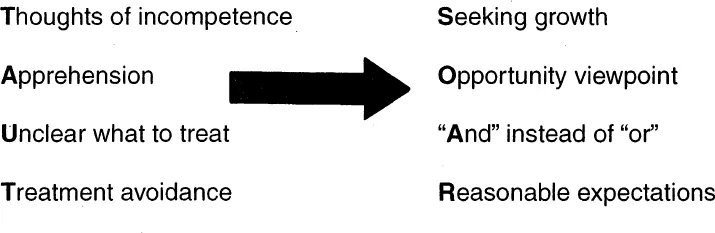
Once therapists identify the types of clients in their caseloads, they need to develop a philosophical base that allows them to work effectively with clients who have many needs. Their philosophy needs to be based on optimism and treatment flexibility. The TAUT-SOAR Model (see Figure 1.1) is useful in working with such diverse caseloads. It is based on the philosophy that the more difficult the issues that the client presents, the more growth opportunities for the therapist.
TAUT stands for Thoughts of incompetence; Apprehension; Unclear what and how to treat; and Treatment avoidance. These are thoughts, feelings, and behaviors that therapists may experience or demonstrate when encountering problems that they believe they are unequipped to treat effectively. For example, the substance abuse therapist might have these reactions to a young adult male client who presents with a history of alcohol and cocaine dependence but also reports hearing voices occasionally and believes that the FBI is following him with helicopters and has bugged his home and car. The mental health therapist might react with TAUT in treating a young female with a history of bipolar disorder who reports drinking excessively and smoking marijuana on a daily basis. When therapists’ anxious thoughts and feelings combine with their confusion concerning a treatment approach, there is a temptation to avoid treating the client. They may either refer the client to another agency based on the excuse that the client has a principle diagnosis that they are not mandated to treat, or make treatment demands that a client cannot achieve. The first method, if successful, simply results in either the mental health therapist treating the substance abuse therapist’s client or the substance abuse therapist treating the mental health therapist’s client, leaving both therapists still feeling only capable of treating part of the client’s problem. The second method—such as the mental health therapist requiring her client to stop all alcohol and drug use before offering medication or other services, or the substance abuse therapist requiring his very paranoid client to attend ninety Alcoholics Anonymous meetings in ninety days—inevitably leads to clients dropping out of treatment. Though the therapist has achieved his or her goal not to treat the individual, the client remains untreated.
FIGURE 1.1. TAUT-SOAR Model
To engage and maintain such clients in treatment, both the substance abuse and the mental health therapist must approach treatment from a different perspective. The second part of our model, SOAR, stands for Seeking growth, Opportunity viewpoint, “And” instead of “or,” and Reasonable expectations. This approach allows therapists to view their clients with less anxiety, more optimism, and more flexibility. Treating these clients becomes an opportunity for the therapists to expand their knowledge about mental disorders and treatment techniques. The client often comes with a history of many treatment failures, so the therapist can feel free to try various techniques with hopes of finding one that works. Each client becomes a research project with an opportunity for that client to obtain something that they had not yet achieved: a treatment success. Furthermore, therapists never have to forget what they already know; however, they now have the opportunity to expand that knowledge and integrate the new and old knowledge into a broader paradigm, which ultimately makes them more effective.
Finally, once a therapist decides to treat a dual diagnosis case, he can establish more reasonable expectations. For example, the mental health therapist can help her client attend an alcohol and drug education class as a first step in addressing the substance abuse disorders; the substance abuse therapist may introduce the concept of schizophrenia to the client, and slowly move him toward a medication evaluation while probing to understand how the psychiatric symptoms impact the client’s substance use. Approaching treatment from a SOAR viewpoint increases the chances that the client will remain in treatment and helps therapists gain confidence in their ability to promote change in clients who have complex problems.
ESSENTIAL KNOWLEDGE AND SKILLS
In addition to having a philosophy that supports working with a multifarious caseload, therapists also need to expand their knowledge and skill bases. Table 1.1 outlines the additional knowledge and skills that both mental health and substance abuse therapists need to work effectively with their diverse caseloads.
The mental health therapist needs to learn about the different types of drugs that her clients may be using and what short- and long-term effects the drugs may have on her clients. She also needs to learn how to monitor urine screens or administer breath tests in a manner that does not interfere with her therapeutic relationship with clients. In addition, she must come to understand the power and the nature of addiction and not be surprised or offended when clients say they want to abstain but then give in to cravings and compulsions. The substance abuse therapist, on the other hand, needs to learn how to identify the various mental disorders that cluster frequently with substance use, and gain an appreciation of how these disorders affect a person’s social skills and ability to function independently in the community.
The substance abuse therapist also needs to understand the different types of medications used to treat these disorders and be able to identify their side effects. He also must learn how to promote medication compliance and deal with any negative values or attitudes that his clients, members of their families, self-help groups, or other substance abuse professionals may have concerning the use of medications. The mental health therapist will have to gain the understanding that abstinence is necessary for individuals with substance dependency disorders or major mental illnesses if they are to achieve and maintain stability. She will need to learn about the purpose, culture, and traditions of twelve-step self-help groups, such as Alcoholics Anonymous and Narcotics Anonymous, and become comfortable promoting clients’ participation in these groups. The substance abuse therapist who is used to requiring his clients to go to these meetings will have to learn that for some individuals, such as those who have social phobias or paranoid thoughts, attendance at these meetings may have to be a long-term goal. He will first need to help them manage their fears about attending such meetings, teach them what to talk about and what not to talk about, and help them understand that some meetings may be open to discussing psychiatric symptoms and others may not. With so many different types of self-help recovery groups now available for both substance use and mental health disorders, both types of therapists need to understand the principles of each in order to help clients select the type of group that is most effective for them.
TABLE 1.1. Additional Knowledge and Skill Needs
Mental Health Therapists | Substance Abuse Therapists |
Nature and effects of psychoactive drugs and the importance of drug testing | Nature and effects of mental disorders |
Nature of addiction | Importance of functioning level |
Importance of abstinence | Importance of medication |
Importance of self-help involvement | Long-term view of self-help involvement |
Working with court-referred clients | Engaging self-referred clients |
Being more concrete, directive, and confrontive | Being less directive, more flexible, and confronting more gently |
Use of self-disclosure | Maintaining clear boundaries |
The substance abuse therapist who is used to having court-ordered clients must learn how to engage self-referred clients, or individuals with whom the court has little leverage. The mental health therapist, on the other hand, must learn to work with clients whose only perceived problem is getting the court system off their backs. Thus the substance abuse therapist will have to learn to be less directive, more flexible, and gentler during confrontations in an effort to engage and keep clients who are not court ordered. The mental health therapist, meanwhile, must learn to be more concrete and directive in setting treatment contracts. She needs to learn to use psychoeducation and confrontational feedback techniques to motivate some clients to address their substance use; such techniques also may help these clients in controlling some of their psychiatric symptoms.
The mental health therapist whose professional training may have taught her never to self-disclose, must learn that some clients need self-disclosure to help them differentiate normal feelings and behaviors from those generated by their mental health or substance use disorders. Take the case of a client whose mother has recently died and is experiencing significantly more depressive symptoms but attributes it all to her medication no longer working. The mental health therapist can assure the client by telling her that’s exactly how she or her friends felt when a parent died and that such feelings are normal and will pass with time. The substance abuse therapist, on the other hand, must learn that maintaining clear boundaries is essential when interacting with some clients. The recovering substance abuse therapist is used to sharing with clients his history of dependency and may in fact encounter clients when he attends his own self-help meetings. However, for clients with certain psychotic, anxiety, and personality disorders, too much self-disclosure or even a simple touch of a shoulder can trigger confusion concerning what is intended or really meant. Thus the substance abuse therapist must learn to be much more withholding with certain clients than he has been in the past.
Finally, both mental health and substance abuse therapists must learn that words they use in their everyday work may have very different meanings for professionals in another field. For example, when the mental health therapist uses the term “defense mechanisms,” she means a psychological process that protects individuals from pain and thus helps them function effectively in the community. The substance abuse therapist, of course, sees defense mechanisms as a negative process that prevents clients from recognizing and acknowledging the fact that they have a substance use disorder. When the substance abuse therapist uses the term “enabling,” he is referring to a behavior that protects individuals from the consequences of their substance use and thus contributes to continue...