eBook - ePub
Delivering CBT for Insomnia in Psychosis
A Clinical Guide
- 294 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
Individuals with psychiatric disorders such as schizophrenia, bipolar disorder, and post-traumatic stress disorder often report Insomnia and difficulties sleeping which can significantly impede recovery, worsen symptoms, and reduce quality of life. This volume presents a detailed theoretical rationale and session-by-session outline for delivering Cognitive Behaviour Therapy for Insomnia to people with these mental health disorders.The treatment has been developed in close collaboration with people living with mental illness, as well as sleep specialists and psychosis experts. Information regarding the efficacy of the programme is presented, along with resources offering information on complicating factors, avoiding relapse, managing stress, and restoring lifestyle balance.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Delivering CBT for Insomnia in Psychosis by Flavie Waters,Melissa J. Ree,Vivian Chiu in PDF and/or ePUB format, as well as other popular books in Psychology & Cognitive Behavioral Therapy (CBT). We have over one million books available in our catalogue for you to explore.
Information
1 Introduction
The term ‘psychosis’ refers to a constellation of clinical symptoms such as hallucinations, delusions, and disorganised thinking, alongside negative symptoms such as reduced motivation and social withdrawal. People living with psychotic symptoms often suffer from disorders such as schizophrenia, schizoaffective disorder, bipolar disorder, substance-induced psychosis, and even major depression or post-traumatic stress disorder (PTSD).
Approximately half of these individuals have other co-occurring difficulties such as cognitive impairments, social and occupational difficulties, and other physical health concerns, many of which persist between psychotic episodes. There is increasing evidence that almost all individuals with psychotic disorders also experience difficulties with their sleep. Approximately half meet the criteria for Insomnia Disorder (from hereon in, also referred to as Insomnia) and/or co-morbid sleep complaints such as hypersomnia, circadian rhythm disturbances, and nightmares.
These disorders of sleep are often distressing and can directly impact on clinical symptoms and the clinical course of an individual’s mental health disorder, as well as their physical health, cognition, and quality of life (see Figure 1.1). Consequently, so that the health and functional recovery of people with psychotic disorders can be optimised, there is a critical need to address and provide effective treatment options for their disturbed sleep. To this end, cognitive behavioural therapy for Insomnia (CBT-I) offers great promise, and this book outlines the theory, evidence, and a detailed description of CBT-I for use in the context of psychotic disorders.
The Psychological Treatment of Psychotic Disorders
There is now robust evidence that psychological treatments can assist in the recovery of individuals with psychotic disorders. Clinical practice guidelines recommend that psychological interventions, such as cognitive behavioural therapy (CBT), should be routinely offered alongside antipsychotic medications as a first-line treatment option (e.g. National Collaborating Centre for Mental Health, 2014).
The use of CBT, in particular, has a 20-year history of treating symptoms of psychotic disorders, with more than 50 randomised controlled trials. Typically, effect sizes are robust, with reports ranging between 0.3 and 0.5 (e.g. Beck and Rector, 2000; Wykes et al., 2008; Grant et al., 2012). Furthermore, CBT has been found to promote a recovery-oriented approach to mental health practice (Bellack, 2006) and is a treatment option that people with psychosis express a desire to engage in (e.g. Kilbride et al., 2013; Waters et al., 2015).
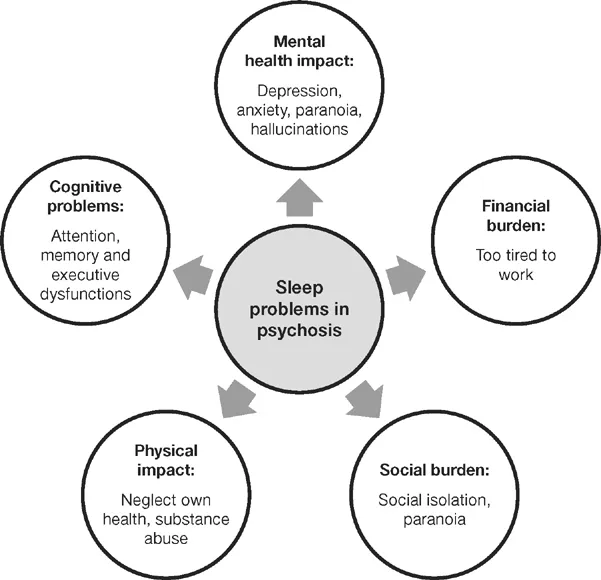
Figure 1.1 Impact of Sleep Problems in Psychotic Disorders
The Treatment of Insomnia and Other Sleep Disturbances Using CBT-I
There is extremely robust evidence for the effectiveness of CBT in addressing sleep disturbances in the general population (CBT-I). Findings show that CBT-I produces longer-lasting effects than pharmacological interventions alone and should be promoted as a first-line treatment option (Jacobs et al., 2004; Qaseem et al., 2016; Schutte-Rodin et al., 2008).
More recently, CBT-I alongside usual treatment (i.e. pharmacological) has emerged as an intervention that has the potential to provide long-term solutions for sleep problems in people with a psychotic disorder (e.g. Freeman et al., 2015; Harvey et al., 2015). Despite the benefits of evidence-based psychological interventions, however, people living with severe and persistent psychotic symptoms often have limited access to these treatment options. This is partly because standard CBT-I programmes need to be adapted to address the additional challenges and circumstances of people with psychotic disorders. When they are adapted appropriately, there is emerging evidence that such programmes can be highly effective for this population.
The aim of this book is to provide a CBT-I framework for clinicians working to address and treat the disorders of sleep in individuals with a psychotic illness. In particular, the manual provides strategies to address Insomnia and related sleep problems in people with chronic psychotic disorders whose levels of functioning and psychopathology are at the severe end of the continuum, and who have previously been considered too low-functioning for traditional CBT-I treatment options. We hope that this book presents a strong argument that clinically meaningful gains can be made with a CBT-I approach for individuals with psychosis.
The development of the manual
We have developed and evaluated a manualised, four-session CBT-I intervention that specifically addresses sleep complaints and related daytime sleepiness in low-functioning individuals with psychotic disorders. Client resource packs and additional materials are also provided to assist the therapeutic process and to encourage clients to self-manage their difficulties. The intervention manual can be administered in either a group or individual format.
The development of this manual and its resources arose from close collaboration with people living with psychotic disorders and Insomnia. Between 2011 and 2014, surveys and focus groups were conducted with representatives from this clinical group to elicit detailed information regarding their personal experience of sleep problems, antecedent factors, and the subsequent impact of these difficulties (Waters et al., 2011, 2012, 2013; Chiu et al., 2016). This preliminary research also identified the knowledge gaps and cognitive styles of these individuals (Chiu et al., 2015), as well as the symptoms they most wanted treated and their preferred method of treatment (Waters et al., 2015).
These findings, together with in-depth enquiries during the development and piloting of the intervention, have ensured that the manual and its resources meet the needs and particular treatment challenges of people with psychotic disorders. Our research indicated that adaptations to standard CBT-I were required so that the specific challenges faced by those with a psychotic disorder were addressed.
Adaptations to CBT-I in this population should ideally accommodate:
• hypersomnia, circadian (sleep–wake) rhythm disruptions, and nightmares because these commonly co-occur with Insomnia;
• the intrusive thoughts, hallucinations, and paranoia that contribute to difficulties in falling asleep and night-time arousal;
• the common use of nicotine, caffeine, alcohol, illicit drugs, and psychotropic medications that impact on sleep onset and quality;
• the lack of daytime structure (e.g. due to low mood, avoidance, unemployment, social isolation) that disrupts sleep routines and circadian rhythms;
• the presence of learning difficulties and other cognitive deficits in domains such as attention and concentration;
• negative symptoms (see Box 2.1), low mood and anxiety;
• low motivation and low self-efficacy.
It is extremely encouraging to see that independent international research appears to be converging on a similar set of adaptations to standard CBT-I for use in individuals with a psychotic disorder. In particular, the work of Freeman and colleagues, in the UK, and Harvey and colleagues, in the USA, have suggested consistent adaptations in their CBT-I protocols.
The specific objectives for our adapted CBT-I intervention for psychosis ensure that it:
• can be delivered to clients with complex needs, varied capacity, and multiple comorbidities;
• provides content that encourages choice and action and that stimulates motivation in order to promote enduring changes in sleep and daytime function;
• is sufficiently practical to be delivered in different clinical settings (inpatient, forensic, community, private);
• can be delivered either in small groups, to facilitate empowerment through peer learning and sharing and to maximise cost-effectiveness, or in an individual format when this is more appropriate;
• is suitable for various health practitioners, including front-line clinicians who have (a) some prior experience in delivering psychological therapies, and (b) a basic understanding of sleep and its regulation (see Chapter 5);
• is based on empirical evidence of beneficial effects on sleep, symptoms, and daytime functioning, and is sufficiently detailed to be independently researched under controlled conditions.
The efficacy of this intervention was evaluated in 72 individuals diagnosed with a psychotic disorder, who presented with a range of psychopathology and functional capacity. Participants received outpatient sessions of adapted CBT-I plus usual treatment or usual treatment alone. Analyses demonstrated significant improvements in sleep and daytime sleepiness, as well as reductions in psychotic symptom severity and psychological distress. None of these benefits was reported by control individuals who received their usual treatment alone (see Chapter 9 for further detail). One of our participants described her experience of CBT-I as follows:
I gave it all I have, because I’ve grown to understand that I have to break the bad sleeping habits really. Psychological therapies probably work better in the long term than medications, I think, because what you learn stays with you.
The collective evidence demonstrates that individuals across the spectrum of psychopathology are capable of engaging with modified CBT-I interventions to make the behavioural and cognitive changes required to improve their sleep and daytime functionin...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Figures, Tables, and Text Boxes
- Preface
- Acknowledgements
- Abbreviations
- 1 Introduction
- Part I Conceptual Frameworks and Evidence Base
- Part II Therapist Manual
- Part III Client Resource Packs
- Part IV Appendices
- Index