![]()
Chapter 1
The Context for Improving Healthcare Team Communication
Christopher P. Nemeth
It is not unusual to find communication failure cited as a “root cause” of healthcare accidents. Single factor solutions, such as standards for how to conduct hand-offs, are recommended in reaction to such conclusions. James Reason’s (1997) description of the factors that contribute to adverse events makes it clear that changing a single factor such as communication cannot overcome the multiple threats to safety in complex systems. This text, then, is not about whether improvement to communications between and among clinicians and patients can solve issues related to healthcare safety. It is: “How can healthcare information be shared better?” and “What can we expect from its improvement, and how do we get there?”
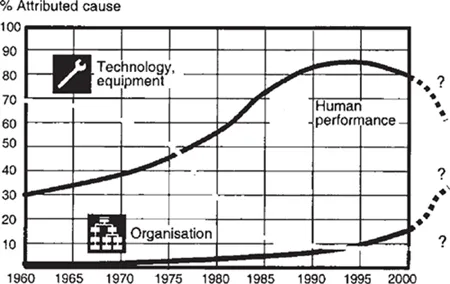
Erik Hollnagel (2004) suggests in Figure 1.1 how understanding adverse events and their causes evolves through time as we develop and use established ways of thinking about how an accident happens. Among technology and equipment, organizations, and human performance, attributions to the latter have peaked over the past 40 years. By implication, attributions to the organization are on the upswing. Among sequential, epidemiologic, and systemic accident models, the systemic model suggests that adverse as well as positive results emerge from daily operations. The research in this text largely follows the systemic model to account for the interactions of clinicians with technology and equipment as well as organizations. The traits of healthcare systems mold the properties, needs, and strategies that require team communication.
Like its high hazard sector counterparts such as aviation, nuclear power generation, ground transportation, and the military, healthcare is typically risky, complex, uncertain, and time-pressured. Staff resources are constrained in a number of ways including availability, qualifications, shift, and rank. Decisions can, and do, have severe consequences. However, healthcare has additional characteristics that make it unique from other high hazard sectors. Guidelines for clinical practice are not consistent and in some instances actually conflict with each other. Demands for care are uncertain, vary widely, and are in a continual state of change. Work is performed on compromised systems (patients) whose affliction and response to treatment is not predictable, can be difficult to assess, and may vary widely. Patients may, or may not, comply with therapeutic regimens. Patient condition, diagnoses, and the procedures to treat them are highly context-specific and individualized. In order to meet these characteristics of the demand for care, equipment and supplies are configured ad hoc—assembled and adapted to fit the individual patient and specific procedure. Decisions on the acquisition of highly sophisticated clinical equipment are routinely made by staff members who have no clinical experience and are advised by clinicians who have no experience in the technical evaluation of complex products or systems.
Figure 1.1 Trends in causes attributed to “accidents”
Source: Hollnagel 2004: 46.
Medical care for patients requires substantial cognitive work. Technical work (Cook, Woods and Miller 1998), which is the many practical and essential activities that are needed to perform medical care, also requires cognitive work. This is because what is needed for an individual patient depends on the timely synchronization of people, equipment, tools, and facilities. The planning and management of procedures for an entire suite of operating rooms (ORs) or an intensive care unit (ICU) require a similar kind of coordination. Both the individual level and the collective unit level require the performance of cognitive tasks that include the assessment of resource availability, resource allocation, the anticipation and prediction of future events, speculation about the best courses of action, negotiation to develop consensus, and trade-off decisions.
Characteristics of work in an organization can be compared to a wedge that has both sharp and blunt ends. At the sharp end, practitioners perform work applying expertise and actions using the resources at hand to generate results. Care providers work in various kinds of groups than can be ill-defined, fluid, and may overlap. They must negotiate multiple constraints in their work domains as they perform complex activities that routinely have significant consequences. The blunt (management) end develops policies, procedures, resources, and constraints that support and shape work at the sharp end (Cook, Woods and Miller 1998: 13, 36). While blunt end cognitive work is more evident, cognition is more difficult to discern the closer one gets to the sharp end. This is because sharp end knowledge is dense, complex, changes rapidly, and is embedded in a complex social setting that resists exposure to those who are considered to be “outsiders.” Clinicians deliberately set the thresholds for access to this setting higher in order to thwart scrutiny and each facility imposes additional controls to protect patient privacy.
Why This Text Matters
One of the reasons behind the popularity of “fixing” healthcare communications is that it is an available target. After all, facilities are costly to build and take a long time. Equipment is complex and requires specialized knowledge to develop and manufacture. Arduous certification procedures take time, money, and effort. People, though, are available and adaptable. The presumption is that if clinicians can be made to behave differently, the difficulties that are brought on by all manner of contributing factors might be eliminated or at least reduced. This view flows from the notion of iatrogenic medical malpractice, which is based on a traditional model that emphasizes individual practitioner agency and accountability. It also stems from hindsight bias (Agans and Shaffer 1994), which leads those who know what happened after the fact to consistently overestimate what others who lacked that knowledge could have known. In reality, practitioners act in concert, collectively coping with system defects that were “created by poor design, incorrect installation, faulty maintenance and bad management decisions” (Reason 1990: 173). Multiple causes of an adverse outcome are usually present in a system as a characteristic of its routine operation. It is poor system design, poor job design, and failed systems that “contribute significantly to harmful error by providing the conditions under which error will thrive” (Sharpe and Faden 1998: 61–77, 138, 234). If failure occurs, it is a “consequence and not a cause” because failures are “shaped and provoked by upstream, workplace and organizational factors” (Reason 1997: 126) such as limited or declining resources.
Healthcare communication must necessarily be as complex as the domain that it is intended to control (Ashby 1956; Conant and Ashby 1970). Contributions by Jens Rasmussen, James Reason, Erik Hollnagel, David Woods, Richard Cook, Yan Xiao and others have demonstrated how healthcare is a variable high stakes sector that is molded by a complex array of factors. “Team” encompasses more than a few individuals, from shifts, clinics, and departments, to clinicians, managers, technicians, suppliers, patients, consultants, and other transferring or receiving care organizations. Healthcare teams can also be fluid, shifting, can overlap, and include strangers as well as colleagues. “Communication” encompasses verbal exchange, but also includes other means to transfer information that include physical artifacts (for example, lists, status boards, schedules, orders, records, and notes), electronic systems (for example, databases, software programs, equipment displays, and controls), as well as phones, pagers, and personal digital assistants.
Views of the way that work is performed also shape notions of the tools that are intended to support it. Recent research into cognition at large scale (Nemeth 2007) in healthcare demonstrates the scope and level of effort that is necessary to understand it. Such studies rely on cognitive systems engineering (CSE) methods (Hollnagel and Woods 1983; 2005) to elicit information about work domains and to derive criteria for the development of information and communications technology (ICT) tools that are intended to aid such work. The insights that the chapters in this text contain can be used to guide the development of ICT that is intended to support healthcare cognitive work. Without the scientific analysis of such complex work, healthcare ICT systems will certainly remain clumsy (Weiner 1985), brittle (Sarter, Woods and Billings 1997), and fail to be a useful team player (Christoffersen and Woods 2002).
Team communications as it is performed in aviation is often proposed as a model for healthcare to adopt. That assumption’s pristine simplicity belies the reality of healthcare’s messy details (Nemeth, Cook and Woods 2004). A number of authors including Helmreich (2000), Helmreich, Musson and Sexton (2001), and Powell, Haskins and Sanders (2005) have encouraged the healthcare community to emulate the models of communications that have been developed in aviation research. Research in aviation team communication cannot be imported in its entirety to healthcare. As the introduction to this chapter explained, the domains are too different for such a simple solution to succeed. Instead, aviation should be understood in terms of what lessons will benefit healthcare communications. Rather than an ending point, research into communication in aviation provides a starting point. This text draws the connection between the lessons that have been learned through cognitive research in aviation and aerospace to cognitive research that is underway in healthcare.
How This Text is Organized
Five sections address improvement to healthcare team communications. Guest author Eric Eisenberg applies his considerable experience in team communications to describe issues that apply across high hazard sectors and to healthcare in particular. This is a valuable contemporary view of organizational communication, with a vocabulary and a framework that we can use to address the very real challenges that face healthcare systems.
Part 1 surveys the origins of research in aviation team communications as a starting point to improve communications in healthcare. Few authors have published on aviation safety as extensively as Judith Orasanu and Ute Fischer. They account for key findings in the aviation literature on aircrew effectiveness, efficiency, breakdown, interrelationships, and error mitigation, then point to lessons from that foundation which can be applied to healthcare. David Musson dispels widely held myths about crew resource management (CRM), which is one of the most popular aspects of aviation communication. Rather than leap into CRM programs, Musson cautions clinicians to better understand the presumed benefits of CRM before adopting them for use.
Part 2 covers recent work in aviation and aerospace that are less well known than flightdeck group studies and CRM, yet provide compelling lessons for healthcare. Asynchrony (conveying healthcare information across time and locations) is growing as the number of participants, and pace and complexity of the care process grows. The potential for gaps in care continuity (Cook, Render and Woods 2000) grows along with it. Two of the chapters in this section share valuable insights into effective ways to deal with asynchrony. Charles Billings, Philip Smith, and Amy Spencer leverage Dr Billings’ seminal work on the Aviation Safety Reporting System to explain the implications for reporting adverse events in healthcare. Emily Patterson describes the National Aeronautic and Space Administration (NASA) use of voice loops that enables staff members to communicate asynchronously and efficiently. Melanie Wright and Mica Endsley explain the close link between healthcare communication and situation awareness—the understanding of dynamic information that is critical for task performance.
In Part 3, recent research in acute healthcare provides a well-grounded understanding of cognitive work and communication among teams. Tom Reader, Rhona Flin, and Brian Cuthbertson describe how variations in care provider perceptions influence ICU team communication. Nemeth et al. describe how clinicians create their own highly plastic forms of hand-offs between shifts in a pediatric ICU as a way to minimize gaps in the continuity of care. Jeff Brown reveals how clinicians collaboratively cross-check each other by detecting, verbalizing, and correcting work in order to sustain safety. Leila Johannesen employs an analytic approach to show how teams maintain a common ground of understanding during complex and extended surgical procedures in the OR.
Part 4 looks to the future of team communications in healthcare, taking particular note of the role that technology will play in both public and professional settings. Anne-Sophie Nyssen and Adélaïde Blavier examine how the addition of a major player – a robotic surgery unit – affects team communication in the OR. Rod Elford shares his insights into telehealth, noting how the ways that remote populations currently rely on Internet resources for healthcare information suggest future aspects of communication among patients and clinicians. Finally, Nemeth and Robert Wears offer thoughts on the future of healthcare team communication and what it will take for further research in this arena to get traction in the real world of clinical practice.
Conclusion
The chapters amply draw the connection from one high hazard sector to another, demonstrating that lessons from aviation and aerospace do inform team communication in healthcare. Their value lies not in the wholesale adoption of procedures, though, but rather in the insights that come from intense study of complex sharp end activities. More than anything, aviation and aerospace research points out how to learn about team communication. The text’s value is not to provide definitive conclusions, but rather to signal a research approach and agenda that will make it possible to better understand and improve team communications in healthcare.
References
Agans, R.P. and Shaffer, L.S. (1994), ‘The Hindsight Bias: The Role of the Availability Heuristic and Perceived Risk’, Basic and Applied Social Psychology 15:4, 439–49.
Ashby, W.R. (1956), An Introduction to Cybernetics (London: Chapman and Hall).
Christoffersen, K. and Woods, D. (2002), ‘How to Make Automated Systems Team Players’, in E. Salas (ed.), Advances in Human Performance and Cognitive Engineering Research 2, 1–12.
Conant, R.C. and Ashby, W.R. (1970), ‘Every Good Regulator of a System Must Be a Model of That System’, International Journal of Systems Science 1:2, 89–97.
Cook, R., Render, M. and Woods, D. (2000), ‘Gaps in the Continuity of Care and Progress on Patient Safety’, British Medical Journal 320:7237, 791–4.
Cook, R.I., Woods, D.D. and Miller, C. (1998), A Tale of Two Stories: Contrasting Views of Patient Safety (Chicago: National Health Care Safety Council of the National Patient Safety Foundation, American Medical Association). <http://www.npsf.org>, accessed June 8, 2002.
Helmreich, R. (2000), ‘On Error Management: Lessons from Aviation’, British Medical Journal 320:7327, 781–5.
Helmreich, R., Musson, D. and Sexton, J.B. (2001), ‘Applying Aviation Safety Initiatives to Medicine’, Focus on Patient Safety: A Newsletter from the National Patient Safety Foundation 4:1, 1–2.
Hollnagel, E. (2004), Barrier Analysis and Accident Prevention (Aldershot, UK: Ashgate Publishing).
Hollnagel, E. and Woods, D. (1983), ‘Cognitive Systems Engineering: New Wine in New Bottles’, International Journal of Man Machine Studies 18:6, 583–600.
Hollnagel, E. and Woods, D.D. (2005), Joint Cognitive Systems: Foundations of Cognitive Systems Engineering (New York: CRC Press).
Nemeth, C. (ed.) (2007), ‘Special Issue on Large Scale Coordination: The Study of Groups at Work in Healthcare’, Cognition, Technology and Work 9:3, 127–76.
Nemeth, C., Cook, R. and Woods, D. (2004), ‘The Messy Details: Insights from Technical Work in Healthcare’, in C. Nemeth, R. Cook and D. Woods (eds), Special Issue on Studies in Healthcare Technical Work, IEEE Transactions on Systems, Man and Cybernetics-Part A 34:6, 689–92.
Powell, S.M., Haskins, R.M. and Sanders, W. (2005), ‘Improving Patient Safety and Quality of Care Using CRM’, Patient Safety and Quali...