eBook - ePub
The Long-Term Impact of Medical Complications in Pregnancy
A Window into Maternal and Fetal Future Health
- 242 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
The Long-Term Impact of Medical Complications in Pregnancy
A Window into Maternal and Fetal Future Health
About this book
This sensible book draws on evidence-based data, provides updated evidence focusing on the impact of pregnancy complications on long-term morbidity of both mother and child and aims to give a clear and comprehensive set of tools for general practitioners counseling women in different stages of their lives. Chapters are contributed by a multidisciplinary team of obstetricians, oncologists, pediatricians, internal medicine specialists, and psychiatrists. The book may serve as a valuable resource for a broad spectrum of clinicians and healthcare professionals. Medical and nursing students as well as residents in family medicine, obstetrics, and pediatrics may derive great benefit from it in various stages of their training.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access The Long-Term Impact of Medical Complications in Pregnancy by Eyal Sheiner in PDF and/or ePUB format, as well as other popular books in Medicine & Gynecology, Obstetrics & Midwifery. We have over one million books available in our catalogue for you to explore.
Information
Topic
Medicine1
Preeclampsia and Long-Term Maternal Atherosclerotic and Cardiovascular Disease
Introduction
Preeclampsia is a multisystem disorder of pregnancy characterized by the new onset of hypertension, usually in the third trimester, and is sometimes associated with proteinuria. It is a major cause of both maternal and neonatal morbidity and mortality [1–3].
Despite the morbidity and mortality associated with preeclampsia, the underlying pathophysiology is not completely understood. It is currently believed that the initiating event is reduced placental perfusion due to shallow cytotrophoblast migration toward the uterine spiral arterioles, leading to inappropriate vascular remodeling and a hypoperfused placenta [4]. The placental ischemia results in the release of factors that cause maternal vascular endothelial dysfunction, which leads to many of the manifestations of preeclampsia including hypertension and proteinuria. Recently, the circulating antiangiogenic factors soluble fms-like tyrosine kinase (sFlt-1) and soluble endoglin (sEng) have been implicated in the pathogenesis of preeclampsia. The administration of adenovirus-expressing sFlt-1 to pregnant rats causes preeclampsia-like syndrome, exacerbated by the coadministration of sEng [5,6]. Moreover, a rise in sFlt-1 and sEng and a reduction in placental growth factor (PLGF) have been demonstrated in maternal serum 5–10 weeks before the onset of preeclampsia and are thought to contribute to maternal endothelial dysfunction [7,8]. Although many of the clinical and physiological manifestations associated with preeclampsia resolve soon after delivery, its impact persists years after pregnancy. Epidemiological studies provide evidence that women with a history of preeclampsia are more likely to develop cardiovascular disease later in life. The strength of these data has led to the American Heart Association (AHA) recommendation that a history of preeclampsia should be considered a major risk factor for cardiovascular disease and cerebrovascular disease [9]. The mechanism linking preeclampsia with future cardiovascular disease are unknown but may include preexisting risk factors common to both preeclampsia and cardiovascular disease such as insulin resistance, obesity, chronic hypertension, renal disease, and diabetes [10–12]. Endothelial dysfunction is an important indicator for subsequent cardiovascular disease and is a regular feature in preeclamptic pregnancies. Several studies have shown reduced maternal endothelial function months to years after a preeclamptic pregnancy [13–15].
In this chapter we will review the epidemiologic data on the increased risk of cardiovascular disease after preeclampsia and highlight the pathophysiologic mechanisms mediating the link between preeclampsia and future cardiovascular disease. Recommendations to optimize the clinical management of women with a history of preeclampsia will be discussed.
Preeclampsia and Long-Term Vascular Complications
Preeclampsia and Future Cardiovascular Disease
In recent years, a growing body of literature has clearly shown a link between preeclampsia and future vascular disease. An increased future risk of hypertension, cardiovascular disease, stroke, and end-stage renal disease has been noted in women with a history of preeclampsia [16–23]. In order to determine the association between preeclampsia and future cardiovascular disease, a systematic review and metaanalysis including 25 studies was carried out [16]. Overall, this meta-analysis included 3,488,160 women, of whom 198,252 had preeclampsia and over three million did not. The relative risk of later development of hypertension in women after preeclampsia was 3.7 (95% confidence interval [CI] 2.7–5.05) compared with women who did not have preeclampsia (Table 1.1). Analysis according to parity indicated a higher risk of hypertension after preeclampsia in any pregnancy compared with preeclampsia in the first pregnancy only [16]. Similarly, women with previous preeclampsia were at increased risk of developing ischemic heart disease (relative risk of 2.16, 1.86–2.52) as well as future fatal ischemic heart disease events (relative risk of 2.6, 1.94–3.49) compared with women with no history of preeclampsia. Moreover, the overall risk of stroke as well as venous thromboembolism in later life also increased among women with a history of preeclampsia, with a relative risk of 1.81 (1.45–2.27) and 1.79 (1.37–2.33), respectively (Table 1.1). However, no increased risk of any cancer, including breast cancer, was found 17 years after preeclampsia. Overall mortality after preeclampsia also increased after 14.5 years, with a relative risk of 1.49 (95% CI 1.5–2.14) [16]. In accordance with these findings, Shalom et al. have recently reported on a significantly higher rate of chronic hypertension in 2072 patients with previous preeclampsia compared with 20,742 patients without a history of preeclampsia (12.5% vs. 0.9%; odds ratio of 15.8, 95% CI 12.9–19.3) [24].
The risk of future vascular disease after preeclampsia seems to be related to the gestational age at delivery and to the severity of preeclampsia (Table 1.2). A Norwegian population-based cohort study has looked at the mortality from cardiovascular causes, cancer, and stroke of 626,272 mothers whose first delivery was registered between 1967 and 1992, with a median follow-up of 13 years [18]. They found that women who had preeclampsia had a 1.2-fold higher long-term risk of death (95% CI 1.02–1.37) than women who did not have preeclampsia, but this risk increased to 2.71 (1.99–3.68) in women with preeclampsia and preterm delivery at less than 37 weeks of gestation compared with women who did not have preeclampsia and whose pregnancies went to term. Furthermore, the risk of death from cardiovascular causes among women with preeclampsia and preterm delivery was 8.12-fold higher (4.31–15.33) than women without preeclampsia who delivered at term, whereas women with preeclampsia who delivered at term had only a 1.65-fold (1.01–2.7) higher risk of cardiovascular death (Table 1.2) [18]. Therefore, women with a history of early-onset preeclampsia appear to be at a much higher risk of future cardiovascular disease compared with women who developed late-onset preeclampsia during their pregnancy. Likewise, in the California Health and Development Study, women with prior preterm preeclampsia (onset of preeclampsia <34 weeks) had a 9.5-fold increased risk of cardiovascular death compared with women with normotensive pregnancies, in contrast to a 2.1-fold risk among women with previous late-onset preeclampsia [25]. A recent study using the same cohort has shown that early-onset preeclampsia (<34 weeks) was not only a strong predictor of cardiovascular death, but also showed evidence of age dependence, as early-onset preeclampsia was associated with very high cardiovascular mortality by age 60 [26]. In a Norwegian study, the hazard ratio for cardiovascular death associated with preterm preeclampsia (delivery <37 weeks) compared with normotensive pregnancy was 3.7 compared with a 1.6-times higher risk among women with prior preeclampsia at term [27]. Moreover, among women with only one lifetime pregnancy, the increased risk of cardiovascular death was higher than for those with two or more children (hazard ratio of 9.44 after preterm preeclampsia and 3.4 after term preeclampsia compared with normotensive pregnancies) [27]. There is also evidence for an association between the severity of preeclampsia and the future risk of cardiovascular disease. Compared with women who had a normotensive pregnancy, women who had mild preeclampsia had a relative risk of future cardiovascular disease of 2 (95% CI 1.83–2.19), women who had moderate preeclampsia had a relative risk of 2.99 (2.51–3.58), and those who had severe preeclampsia had a relative risk of 5.36 (3.96–7.27) [28]. Similarly, Kessous et al. have recently shown a significant association between preeclampsia and cardiovascular morbidity (Figure 1.1). Moreover, they have shown a linear association between the severity of preeclampsia (no preeclampsia, mild preeclampsia, severe preeclampsia, and eclampsia) and the risk of future cardiovascular morbidity (2.75 vs. 4.5% vs. 5.2% vs. 5.7%, respectively; p = .001) [29].
TABLE 1.1
Preeclampsia and Risk of Future Vascular Disease
Disease | Mean Follow-Up (Years) | Relative Risk | 95% CI |
Hypertension [14] | 14.1 | 3.7 | 2.7–5.05 |
Ischemic heart disease [14] | 11.7 | 2.16 | 1.86–2.52 |
Stroke [14] | 10.4 | 1.81 | 1.45–2.27 |
Thromboembolism [14] | 4.7 | 1.79 | 1.37–2.33 |
End-stage renal disease [19] | 26.5 | 4.7 | 3.6–6.1 |
TABLE 1.2
Preeclampsia and Risk of Cardiovascular Mortality According to Gestational Age at Onset or Delivery
Reference | Definition of Early Preeclampsia | Early Preeclampsia: Hazard Ratio (95% CI) for Cardiovascular Death | Late Preeclampsia Hazard Ratio (95% CI) for Cardiovascular Death |
Irgens et al. [18] | Delivery <37 weeks | 8.12 (4.3–15.3) | 1.65 (1.0–2.7) |
Mongraw-Chattin et al. [25] | Onset <34 weeks | 9.54 (4.5–20.2) | 2.08 (1.2–3.4) |
Cirillo and Cohn [26] | Onset <34 weeks | 6.7 (2.7–16.2) | 2.5 (1.3–3.8) |
Skjaerven et al. [27] | Delivery <37 weeks | 3.7 (2.7–4.8) | 1.6 (1.4–2.0) |
Another question is the extent to which recurrent preeclampsia is associated with cardiovascular risk. Preeclampsia usually occurs only in first pregnancies and recurs in only 15% of second pregnancies following a first pregnancy complicated by preeclampsia. Less than 1% of parous women experience preeclampsia twice. However, those who do appear to be at especially high risk of cardiovascular disease. In a registry-based cohort study from Denmark, multiparous women had a 1.3-fold (95% CI 1.1–1.5) increased risk of future cardiovascular disease if their first pregnancy was preeclamptic, and a 2.8-fold (95% CI 2.3–3.4) increased risk after two pregnancies complicated by preeclampsia compared with multiparous women without hypertensive disease. The corresponding relative risks for stroke were 1.2 and 1.5 [30]. Likewise, Kessous et al. have recently demonstrated a significant linear association between the number of previous pregnancies with preeclampsia and the risk of future cardiovascular disease [29]. In a Norwegian study, the differences in cardiovascular risk were more subtle among women with nonrecurrent and recurrent preeclampsia: women with preeclampsia only in their first pregnancy had a relative risk of cardiovascular death of 1.5 (1.2–1.9), whereas women with two preeclamptic pregnancies had a relative risk of cardiovascular death of 2 (1.2–3.3) compared with multiparous women with normotensive pregnancies [27].
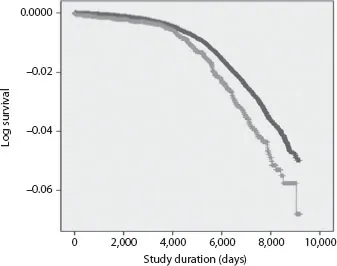
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Dedication
- Table of Contents
- Preface
- Contributors
- 1. Preeclampsia and Long-Term Maternal Atherosclerotic and Cardiovascular Disease
- 2. Gestational Diabetes Mellitus: Definition, Pregnancy Complications, and Long-Term Maternal Complications
- 3. Placental Syndrome and Long-Term Maternal Complications
- 4. Pregnancy Complications and Impact on Long-Term Oncological Morbidity of the Mother
- 5. Recurrent Pregnancy Loss: Overview and Impact on Future Maternal Health
- 6. Preterm Parturition and Long-Term Maternal Morbidity
- 7. Renal Function Tests during Pregnancy and Long-Term Risk of Atherosclerotic Morbidity
- 8. Pregnancy and Depression: The Tip of the Iceberg?
- 9. Pregnancy and Thromboembolic Morbidity
- 10. Cholestasis and Long-Term Maternal Morbidity
- 11. Fertility Treatment and Maternal Cardiovascular Risk
- 12. Pregnancy as an Opportunity for Weight Control and Smoking Cessation
- 13. Preeclampsia and Long-Term Risk for the Offspring
- 14. Life Course Outcomes for the Child of the Diabetic Mother
- 15. Intrauterine Growth Restriction and Long-Term Disease of the Offspring
- 16. Long-Term Effects of Premature Birth
- 17. Long-Term Health Outcomes for Children Born as a Result of In Vitro Fertilization Treatment
- 18. Long-Term Impact of Antidepressant Exposure in Pregnancy: A Window into Developmental Outcomes in the Child
- Index