Making Sense of Fluids and Electrolytes
A hands-on guide
- 172 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
About this book
Interpreting the fluid requirements of a patient and working out what to do next can seem like a daunting task for the non-specialist, yet it is a skill that any doctor, nurse or paramedic needs to be fully appraised of and comfortable with.
Making Sense of Fluids and Electrolytes has been written specifically with this in mind, and will help the student and more experienced practitioner working across a variety of healthcare settings to understand why fluid imbalance in a patient may occur, to assess quickly a patient's fluid needs through a thorough clinical assessment and to develop an effective management plan. Reflecting the latest guidelines, this practical, easy-to-read and easy-to remember guide will be an invaluable tool to aid speedy and appropriate management in emergency situations, on the ward and in the clinic.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
CHAPTER 1
Fluid assessment
FLUID ASSESSMENT – FORMAT
HISTORY
Current medical problem
Why is the patient in hospital?
Current fluid status
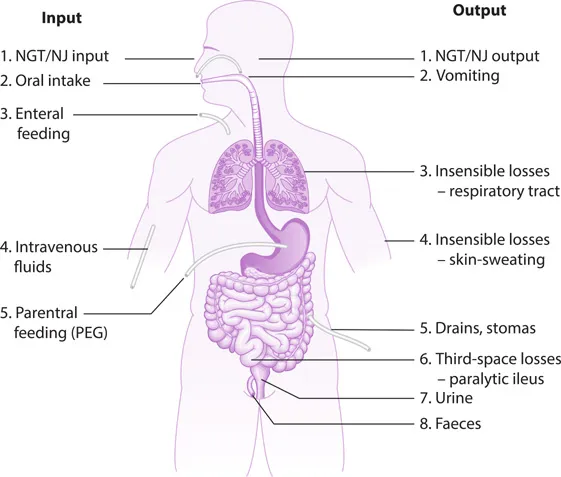
Intake
- Oral intake: All types of fluid
- IVF: Note types of fluids (crystalloids, colloids, blood products) and electrolyte composition
- Parenteral feeding: Note electrolyte composition
- Enteral feeding via a nasogastric tube (NGT), nasojejunal (NJ) tube or a percutaneous endoscopic gastrostomy (PEG) tube
Output
- Previous/current diarrhoea, vomiting, urination and faeces.
- Catheters, drains, stoma outputs, NGTs, NJs, PEGs.
- Third-space losses, which are those where fluids shift to a ‘new’ compartment which is an extension of the extracellular fluid (ECF). This is sometimes seen in paralytic ileus, peritonitis and conditions causing ‘leaking’ from capillaries, such as anaphylaxis and sepsis.
- Insensible losses, which are those that cannot be accurately measured but can contribute significantly to a patient’s fluid losses (Figure 1.1):
- Respiratory tract: Fluid that evaporates from the respiratory tract increases with increased respiratory rate, ‘mouth breathers’ and also in ventilated patients.
- Skin: Sweating and pyrexia will increase fluid loss.
- Surgical evaporation: Evaporation from exposed surgical sites during the operation.
Hypovolaemia
- Symptoms: thirst, oliguria/anuria, orthostatic hypotension, headache, lethargy, confusion, vomiting, diarrhoea
- Signs: decreased skin turgor, increased capillary refill time (>2 seconds), cool peripheries, dry mucous membranes, tachycardia, weak thready pulse, tachypnoea, hypotension, increased respiratory rate, coma
Hypervolaemia
- Symptoms: polyuria or oliguria, shortness of breath (SOB), orthopnoea
- Signs: peripheral and central oedema, ascites, raised jugular venous pressure (JVP), added heart sounds, basal crepitations on chest auscultation, increasing weight over a short period of time, headache, confusion, coma
Compartment | Symptoms of hypovolaemia | Symptoms of hypervolaemia | Signs of hypovolaemia | Signs of hypervolaemia |
Intravascular | Thirst, nausea | Tachycardia, hypotension | Raised JVP | |
Interstitial | Thirst, nausea | SOB, orthopnoea | No oedema, dry mucous membranes, poor skin turgor | Oedema, ascites In good hydration: moist mucous membranes, good skin turgor |
Intracellular | Headache, coma | Difficult to assess directly | Difficult to assess directly |
Past medical history
- Cardiovascular: Ischaemic heart disease (IHD) and heart failure (HF) will, in varying degrees, affect the heart’s ability to pump blood around the body. Be cautious when prescribing fluid as decreased cardiac output might result in excess fluid outside the intravascular space, especially in patients with congestive cardiac failure (CCF). At the same time, it is important to aim for euvolaemia in these patients to ensure an adequate stroke volume and cardiac output (remember the Frank–Starling mechanism). Traditionally, getting the fluid balance right in this particular group of patients has always been a big challenge for doctors.
- Renal: Depending on the extent and cause of acute kidney injury (AKI) a patient may require extra fluids, or conversely they may require dialysis. Dehydration is one of the main causes of AKI, hence most patients require IVFs to manage their condition (a balanced crystalloid such as Hartmann’s is generally the first choice). If, however, an AKI patient is oligo-anuric and develops clinical signs of fluid overload, in most cases this would be an indication for urgent renal replacement therapy. Chronic kidney disease (CKD) of varying degrees will affect how the body excretes fluids and electrolytes and hence the quantity and type of fluid required. Patients with end-stage renal failure may be on dialysis and no longer producing any urine; fluid therapy in these patients should be measured and conducted under senior guidance.
- Hepatic: Decompensated liver disease may affect s...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Acknowledgements
- List of abbreviations
- How to use this book
- 1 Fluid assessment
- 2 Keeping the balance: physiology, electrolytes and intravenous fluids
- 3 Cardiac arrest and shock
- 4 Intravenous fluid therapy in medical patients
- 5 Fluid therapy management in surgical patients
- 6 Blood products and transfusion
- Index