![]()
SECTION 1
HEAD AND NECK
![]()
CHAPTER 1
Diseases of the Oral Cavity
Urjeet A. Patel, Alice C. Lin, and Christopher Vanison
• Angioedema
• Ameloblastoma
• Keratocyst odontogenic tumor
• Lip cancer
• Mucosal melanoma
• Oral cancer
• Ranula
Angioedema
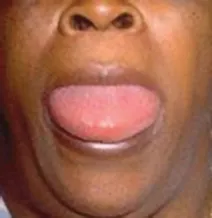
DEFINITIONS AND CLINICAL FEATURES
Angioedema is a rapid swelling or edema of the dermis, mucosa, or submucosa. It is usually associated with allergy and is frequently seen as a drug reaction, particularly to antihypertensive ACE inhibitors. The skin of the face and lips may become rapidly swollen over the course of minutes to hours. More concerning, however, is the edema that often occurs in the oral and oropharyngeal mucosa resulting in dramatic tongue and pharynx edema. In such cases, inspiratory stridor can develop with imminent airway obstruction (Figures 1.1 and 1.2).
Angioedema can be classified as acquired or hereditary. Patients with acquired angioedema generally have a history of allergy, and episodes may occur in conjunction with other allergic findings such as urticaria. Hereditary angioedema is caused by a genetic mutation that is inherited in an autosomal dominant fashion. This results in diminished levels of the C1-inhibitor protein, which then leads to abnormal activation of the complement cascade as the trigger for clinically apparent angioedema.
Figure 1.1 Angioedema involving the oral tongue.
Figure 1.2 Angioedema involving the upper lip.
DIFFERENTIAL DIAGNOSIS
Urticaria, allergic reaction, anaphylaxis.
WORKUP
The diagnosis of angioedema is based largely on the clinical picture. Testing may include routine blood tests in addition to complement levels.
TREATMENT
Since the acute episode may be life threatening, early treatment involves acute administration of steroids and antihistamines. If a drug history demonstrates a likely culprit, such medications are of course discontinued. In life-threatening cases, the airway must be stabilized by either elective intubation or urgent/emergent tracheotomy or cricothyrotomy placement. In less critical patients, airway observation may be sufficient as medical therapy is instituted and the angioedema resolves.
Ameloblastoma
DEFINITION AND CLINICAL FEATURES
Ameloblastoma is a benign tumor arising from the odontogenic epithelium and is more commonly seen in the mandible compared to the maxilla (Figure 1.3). They are most commonly associated with unerupted teeth and are generally seen in the posterior aspect of the maxilla or mandible. These tumors are rarely malignant or metastatic; however, they are progressively enlarging lesions that can be locally destructive to the native bone and surrounding soft tissue. Accordingly, they can cause significant facial deformity and functional difficulties with mastication if left untreated.
DIFFERENTIAL DIAGNOSIS
Other benign tumors of the mandible and maxilla including dentigerous cyst, odontogenic keratocyst, odontogenic myxoma, giant cell granuloma.
Figure 1.3 Facial deformity caused by underlying ameloblastoma of the left mandible.
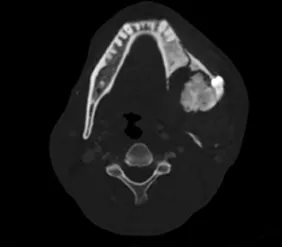
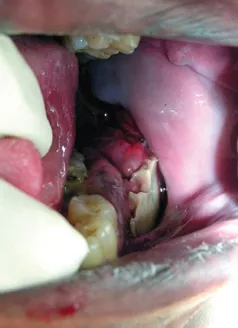
WORKUP
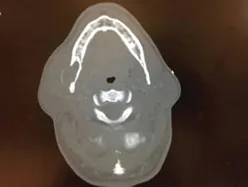
Imaging is recommended for workup of ameloblastoma. This begins with either plain films or panorex imaging, followed by CT scan if ameloblastoma is considered (Figure 1.4). Given the slow-growing nature of this lesion, the bone is often expanded and remodeled with a thin layer of new bone deposited and the leading edge of growth. This can often be seen as an expansile lesion on imaging studies. Biopsy is recommended, often transoral, to make the definitive diagnosis to guide further treatment (Figure 1.5).
Figure 1.4 CT scan demonstrating expansile lesion of the mandible.
Figure 1.5 Intraoral appearance of soft tissue extension to the gingival and buccal mucosa.
TREATMENT
The mainstay of treatment is surgical excision. Given the locally aggressive nature of this disease, curettage is considered insufficient and proper treatment requires wide surgical excision. Curettage has been attempted, though often results in recurrence of disease. Accordingly, wide surgical margins are required for definitive treatment and may result in segmental resection of the jawbones to optimize prognosis.
Keratocyst odontogenic tumor
DEFINITION AND CLINICAL FEATURES
Keratocystic odontogenic tumor (KCOT) is a developmental cystic lesion arising from remnants of the dental lamina, most often in the posterior mandible. Previously referred to as “odontogenic keratocyst,” this lesion was recently reclassified as a neoplasm due to its aggressive clinical course and high propensity for recurrence. KCOTs are typically unilocular cysts that are lined with epithelium and filled with keratinaceous material. Patients with basal cell nevus syndrome (Gorlin syndrome) may have multiple KCOTs. These tumors may grow rapidly and can be locally destructive. Many prove difficult to eradicate and recurrence is common. Rarely, KCOTs may transform to other benign odontogenic tumors such as ameloblastomas or even malignant tumors such as squamous cell carcinoma. Patients most commonly present with enlarging facial mass or swelling in the second through fourth decades.
DIFFERENTIAL DIAGNOSIS
Ameloblastoma, dentigerous cyst, giant cell granuloma, radicular cyst, metastasis.
WORKUP
KCOTs are typically first noted on plain film or panorex. CT and MRI are typically not necessary. Imaging alone is insufficient for diagnosis as the radiographic appearance frequently mimics that of a variety of odontogenic cysts and tumors. Because KCOTs behave aggressively, they must be differentiated from these other lesions. Therefore, histologic diagnosis is important for both patient counseling and treatment choices. Biopsy including the epithelium should be performed transorally, if feasible (Figure 1.6).
TREATMENT
Surgery is the mainstay of treatment for KCOT. The removal of the epithelial lining is imperative for successful eradication. For this reason, simple marsupialization and curettage are considered less effective than more aggressive methods. Enucleation is performed and is typically accompanied by removal of a peripheral margin or bone or by cryotherapy. In cases of extensive or recurrent disease, more radical resections such as segmental mandibulectomy or partial maxillectomy may be required.
Figure 1.6 CT scan of keratocystic odontogenic tumor involving the right mandible posteriorly.
Lip cancer
DEFINITION AND CLINICAL FEATURES
Lip cancer is considered the most common form of oral cancer, though it has its own dedicated staging system separated from other oral cavity tumors. It can occur on either the upper or lower lip, though the lower lip is more common and slow growing. The vast majority are squamous cell carcinomas that arise from the normal squamous cells of the lip epidermis. While squamous cell carcinoma is the most common, basal cell carcinoma and minor salivary gland carcinoma may also arise in the lip. Risk factors include cigarette smoking, pipe smoking, thermal or traumatic injury, and UV light exposure. Lesions may arise as small ulcers at the vermillion border of the lip that are most often painless. Lesions continue to grow and may ultimately invade deeper structures such as the mandible or may metastasize to regional lymph nodes in the submental and submandibular regions (Figures 1.7 and 1.8).
Figure 1.7 Lip cancer involving the midline lower lip.
Figure 1.8 Lip cancer involving the midline upper lip.
DIFFERENTIAL DIAGNOSIS
Like other forms of oral cancer, lip carcinoma must be distinguished from other benign or infectious lesions. These include aphthous ulcer, herpes infection, leukoplakia, and lichen planus.
WORKUP
The workup of a concerning lip lesion begins with incisional biopsy. If the lesion is very small, the entire lesion may be removed at time of biopsy with an adequate margin. For larger lesions, incisional bx yields the diagnosis, and definitive treatment can then be planned. For small lip carcinomas, CT scan is recommended to assess for deeper invasion and assess regional lymph nodes. For small lesions, CT scan may not be required.
TREATMENT
Lip cancer is most often treated with surgical excision. Lip lesions measuring several centimeters may be resected with good reconstructive options that offer good functional and cosmetic results. Lesions are generally resected with a...