Macroergonomic issues
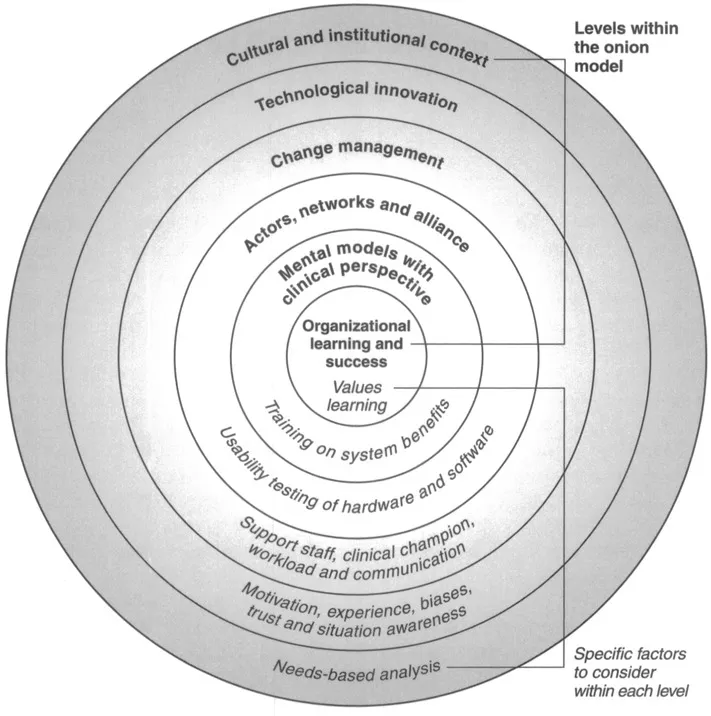
Macroergonomic issues concern organizational issues and the design of workplace systems (see reference 14 for a review). One macroergomic issue to consider is the cultural or institutional context in which the telemedicine technology is implemented (the first layer within the onion model). This issue is particularly salient when evaluating a telemedicine system within the US military, as each military branch has its own distinctive organizational culture. Moreover, some branches may be more receptive to telemedicine technologies based on their population’s needs. For example, US Navy personnel may be more likely to adopt a telemedicine system than other military branches due to the population’s distance from specialist care. As a result of these distinct organizational climates, an evaluation of any telemedicine system must include a needs analysis. A needs analysis is conducted to define the needs of the user population and their expectations of the system.15 A telemedicine system will not be easily adopted if the user population does not perceive a need for telemedicine regardless of whether such a system could benefit the organization.
When evaluating the cultural climate within an organization, one also should consider whether the organization values learning (the sixth layer within the onion model). A telemedicine system is more likely to succeed within an organization that incorporates educational opportunities for the development of new skills.7 An organization needs to be supportive of the telemedicine technologies and willing to devote the resources necessary to train users on the system’s components.
The development of effective training programs is an essential macroergonomic issue as it leads to clinician acceptance.11,12,16 In a survey of a store-and-forward ophthalmic telemedicine system used by the US Army, users reported difficulty viewing images because they did not know how to use the software.16 However, a training program should not be limited to training on the technology and/or software used within the system. Bangert et al.11 assessed the training needs of military healthcare providers by distributing surveys to users and non-users of telemedicine programs. Participants were asked to rank the importance of different learning objectives. Their responses were grouped according to four categories and it was found that the clinical aspects of telemedicine were considered most important for a training program (e.g. specifics about conducting a consultation), followed by the training of telemedicine technologies, organizational/management issues (e.g. funding) and the fundamentals of telemedicine (e.g. history of telemedicine).
Training also should be viewed as an opportunity to explain the organizational benefits to using telemedicine systems. Physicians within a telemedicine system may have limited mental models concerning how telemedicine can benefit them (layer five within the onion model – mental models with clinical perspective). In fact, telemedicine technologies offer benefits to both physicians and patients within the military environment. Telemedicine can increase the opportunities for physicians to interact professionally with specialists, provide educational opportunities and reduce the number of unnecessary patient referrals.4 For example, one telemedicine system offered physicians the opportunity to earn continuing medical education credits through online courses and hosted online conferences where physicians could meet to share information about consultations.17
Physicians will be more receptive to a telemedicine technology if their peers endorse it.10 In particular, physicians have knowledge of the clinical issues related to telemedicine and can explain to other physicians how the system can benefit their practice.9 However, the initial acceptance of physicians must lead to continued acceptance for the success of the telemedicine system. To achieve success, the telemedicine system needs the support of a physician at each site (i.e. a clinical champion) to ensure its continued use.
This clinical champion also can serve as a leader or manager to facilitate the organizational changes that need to occur as a result of the telemedicine system (layer three within the onion model – change management). For example, the clinical champion can manage how workload is distributed among the different team members. The use of a telemedicine system may increase the overall workload for physicians and their clinical staff,6 and there should be assistants in place to handle the administrative aspects of the system to reduce workload.9 Workload is also an issue at the organizational level. It is important that specialists receive recognition for the consults that they answer.7 Currently, a DoD working group has been tasked with the responsibility to complete the workload credit for a teleconsultation (Dingbaum, personal communication). Though not complete, it provides guidance on how to obtain workload credit for a teleconsultation. However, at this time, a teleconsultation is not considered equal to a face-to-face consultation. Thus, the inclusion of an organizational support staff would be essential in managing overall workload in a military environment. The support staff should manage the number of consultations that a specialist receives to avoid overburdening them and losing their participation within the system.
The support staff also could be responsible for managing communication between team members located at different sites. Within a telemedicine system, information is transferred between users and there can be multiple streams of information (i.e. patients). The support staff need to maintain an overall awareness of the status of information within the system. Users a...