- 144 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
In this new color handbook, the authors deal systematically with those skin conditions that are particular to or more common in the elderly covering testing, diagnosis and treatment options. Given ageing populations the need for such a book is urgent. More and more elderly patients will seek care for a variety of skin conditions, ranging from eczem
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Skin Diseases in the Elderly by Colby Evans,Whitney High in PDF and/or ePUB format, as well as other popular books in Medicine & Dermatology. We have over one million books available in our catalogue for you to explore.
Information
PART 1 Skin changes with aging
Although elderly patients are prone to a number of skin diseases, there exist also typical age-related skin changes that are not disease associated. Although these changes occur to all patients, should they live long enough, they can have profound effects on the proper function of the skin, and, hence, the patient’s corresponding quality of life.
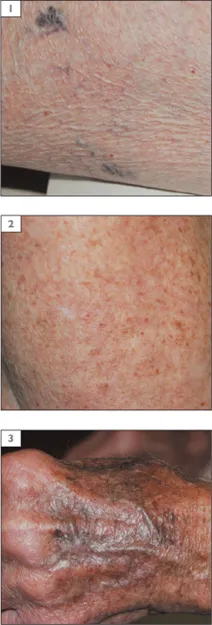
Age-related atrophy
Skin atrophy is commonly seen in elderly patients, evidenced by thinning or fine wrinkling, easy tearing, and bruising. In sun-protected sites, this atrophy usually results in fine, ‘cigarette paper’ wrinkling of the skin (1&2). The skin is often light in color compared with chronically sun-exposed skin.
Fat loss, especially on the face and hands (3), is quite common with age. Since the fat layer provides a cushion for blood vessels, they become more visible with time and more prone to bleeding with minor trauma. Fat loss, especially in the face and hands, is also a common cosmetic concern for older patients.
1–3 Skin atrophy.
Solar atrophy
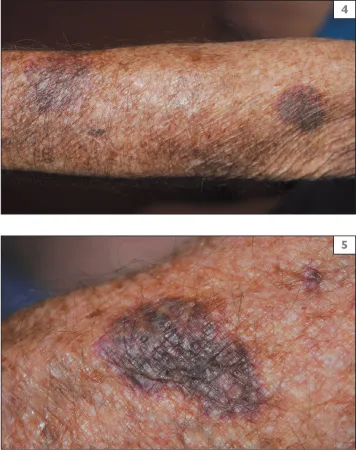
Atrophy is also common on the sun-exposed skin, but in a different form. Solar atrophy often exhibits hyperpigmentation, deep wrinkles, and a ‘leathery’ appearance. It is commonly seen on the face, neck, forearms, and dorsal hands. It not only leads to easy tearing and bruising of the skin (4), but is a sign of chronic sun damage which can lead to other problems, especially skin cancer.
Bruising
Elderly patients often complain of easy bruising and tearing of the skin that leads to bleeding (4&5). One contributory cause is the blood-thinning medications often taken by elderly patients to prevent myocardial infarction or stroke. Aspirin, warfarin, and clopidogrel are common examples. Other medications, especially NSAIDs, may also increase this tendency. Even patients who do not take such medications, however, may also experience easy bruising due to fat loss and skin atrophy, with subsequent loss of the surrounding supportive collagen near vessels, leading to bruising on the frequently traumatized forearms and hands.
4, 5 Bruising.
Xerosis
As the skin ages, its ability to produce and maintain the normal oils and fats that help retain moisture erodes. The skin becomes drier and moisturizer must be applied more often to avoid itchy, painful, or fissuring skin (6 see also 84). Xerosis (skin dryness) is usually worse in the winter due to low humidity and indoor heat. Xerosis may be a problem unto itself or it may worsen common skin conditions such as eczema or psoriasis. It can be particularly difficult for elderly patients to avoid, as bathing and applying moisturizer may be more difficult due to arthritis, visual problems, or other comorbid conditions.
Varicosities
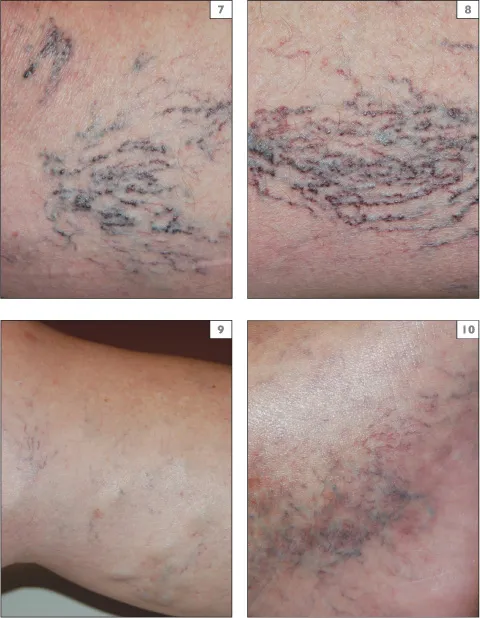
Since gravity attempts to pull all blood towards the feet, the vessels of the legs are under constant pressure. A system of muscular milking and valves helps return the blood to the heart, but these vessels weaken over years of time and pressure, and varicosities are the result. Superficial or deep, red, blue, or purple serpiginous veins are visible on the legs (7–10). Varicosities may be both medically and cosmetically troublesome. If they are painful, examination by ultrasound may be necessary followed by vein stripping or endovascular procedures performed with a heat probe or laser. Cosmetically bothersome veins can often be treated with sclerotherapy, the injection of a sclerosant material into the vein causing it to seal closed.
6 Xerosis.

7–10 Varicosities.
PART 2 Inflammatory skin disease
• Autoimmune
• Neutrophilic dermatoses
• Allergic and hypersensitivity processes
• Photorelated conditions
• Other inflammatory conditions
AUTOIMMUNE
Bullous pemphigoid
DEFINITION AND CLINICAL FEATURES
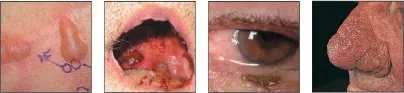
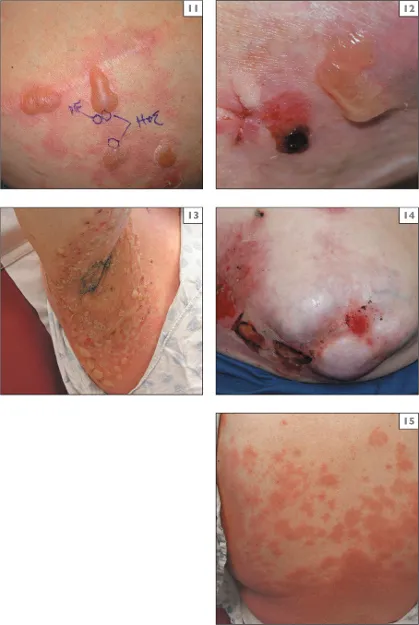
Bullous pemphigoid (BP) is an autoimmune blistering disorder that often results in large, tense, bullae (11). These bullae, being subepidermal in origin, are often resistant to rupture and, in comparison to pemphigus, intact blisters on clinical exam are not unexpected. Lesions of BP often appear first on the flexural aspects of the limbs (12), including the axilla (13). The trunk may be involved as well (14). Associated pruritus can be intense.
The face and scalp are not often involved in BP, and while the mucosa may be involved in up to 10–25% of cases, in direct contrast to pemphigus vulgaris, the mucosa is not typically the site of first involvement in this disease. Urticarial BP is a variant that presents with intense itching and erythematous skin lesions, but lacks frank bullae (15). Sometimes patients with urticarial BP may never develop blisters and, on occasion, the condition may be present for years before the diagnosis is established.
EPIDEMIOLOGY
BP is chiefly a disease of the elderly. The average age at onset is about 65 years. Females and males are equally affected and the disease is seen in all races. It is not uncommon for a patient with BP to have multiple comorbidities; a factor that must be considered in prescribing treatment with corticosteroids or immunosuppressive medications.
DIFFERENTIAL DIAGNOSIS AND INVESTIGATIONS
Other bullous skin diseases, such as pemphigus, cicatricial pemphigoid, bullous lupus erythematosus, epidermolysis bullosa acquisita, and porphyria cutanea tarda must be considered. Some medications may cause drug-induced bullous disorder resembling BP.
The diagnosis of BP is most easily established by histological analysis. Light microscopy should be performed from the edge of a blister and direct immunofluorescence studies should be performed on normal-appearing perilesional skin (11). Routine histology demonstrates a subepidermal vesiculatory process, often with a preponderance of eosinophils in the blister cavity.
Direct immunofluorescence studies demonstrate the deposition of immunoreactants as a band at the dermoepidermal junction of the skin. This pattern of deposition is not specific for BP and it may be seen in cicatricial pemphigoid and epidermolysis bullosa acquisita, as well. Clinical information, the findings of light microscopy, performance of direct immunofluorescence on salt-split skin (with induced separation at the dermoepidermal junction) or indirect immunofluorescence studies using the patient’s serum and normal salt-split skin can be used to further refine the diagnosis.
ELISA testing is increasingly available at major medical centers and this can detect one of the pathological antibodies (BP antigen-1) in more than 90% of patients with BP.
SPECIAL POINTS
Because a biopsy from the center of a lesion of BP rarely provides any useful diagnostic information by light microscopy, and may in fact yield false-positive results by immunofluorescence, many experts advocate the deep-shave (saucerization) excision of a small bullae intact for histological examination. A small perilesional punch may then be performed for immunofluorescence studies.
Unlike in pemphigus, it does not appear that the titers as measured by ELISA correspond to disease activity in BP.
Since BP is an antibody-mediated autoimmune condition, immunosuppressive therapies are often helpful. Prednisone is the mainstay of initial treatment, but the condition may recur when it is tapered.
Since prednisone causes significant side effects when used long term, increasingly, dermatologists use less-noxious anti-inflammatory regimens, such as combination therapy with tetracyclines and nicotinamide, as steroid-sparing agents in the management BP. These are often easily tolerated even in elderly patients.
If these more gentle regimens are not successful, more aggressive immunosuppressant agents, such as mycophenolate mofetil or azathioprine may be needed. These agents have serious potential side effects and should be managed by providers experienced in their use.
11–15 Bullous pemphigoid (11–14); urticarial bullous pemphigoid (15).
Cicatricial pemphigoid (mucous membrane pemphigoid)
DEFINITION AND CLINICAL FEATURES
Cicatricial pemphigoid (CP), also known as mucous membrane pemphigoid, refers to a group of autoimmune blistering disorders that cause primarily erosions on mucosal services, specifically the oral mucosa and conjunctiva (16 & 17). The skin may also be affected, particularly that of the scalp, head and neck, the distal extremities, or the trunk (18)...
Table of contents
- Cover Page
- A Color Handbook Skin Diseases in the Elderly
- Dedication
- Copyright Page
- CONTENTS
- PREFACE
- ABBREVIATIONS
- SUGGESTED READING
- PART 1 Skin changes with aging
- PART 2 Inflammatory skin disease
- PART 3 Neoplasms of the skin
- PART 4 Infestations and infections
- PART 5 Metabolic and nutritional disease
- PART 6 Skin signs of systemic disease
- INDEX