eBook - ePub
Genital and Perianal Diseases
A Color Handbook
- 288 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Genital and Perianal Diseases
A Color Handbook
About this book
Highly Commended, BMA Medical Book Awards 2014Despite the development of penicillin and other treatments, the incidence of sexually transmitted diseases (STDs) worldwide continues to rise. In Genital and Perianal Diseases, A Colour Handbook, the authors discuss the diagnosis and treatment of the main cutaneous conditions of the anogenital region, w
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Genital and Perianal Diseases by Tomasz F. Mroczkowski,Larry E. Millikan,Lawrence Charles Parish MD in PDF and/or ePUB format, as well as other popular books in Medicine & Dermatology. We have over one million books available in our catalogue for you to explore.
Information
SECTION 1

SEXUALLY TRANSMITTED DISEASES
CHAPTER 1

Syphilis
Erin Santa, MD, and Joya Sahu, MD
• Definition and epidemiology
• Primary syphilis
• Secondary syphilis
• Early latent syphilis
• Tertiary syphilis
• Congenital syphilis
• Treatment

Definition and epidemiology

Syphilis (Lues) is a chronic sexually transmitted infection caused by the spirochete Treponema pallidum. The disease is defined by primary, secondary, and tertiary stages, with intervening periods of latency. If left untreated, it may be either self limiting or progress, causing serious complications several years after acquisition. Pregnant women, if untreated, may pass infection to their infants transplacentally – congenital syphilis1,2.
In the USA, rates of syphilis fell by 95% between 1945 and 2000 with the advent of penicillin therapy3. Unfortunately, in more recent years, there has been a steady increase in rates of the disease, specifically in men who have sex with men (MSM). In the early 2000s, rates of syphilis were reported to be highest in MSM aged in their 30s; however, a recent study has shown that syphilis is increasingly affecting younger MSM, those between the ages of 15 and 29, in addition to black and Hispanic MSM4,5.

1.1 Primary lesion in the early stage of development.
Primary syphilis

CLINICAL FEATURES
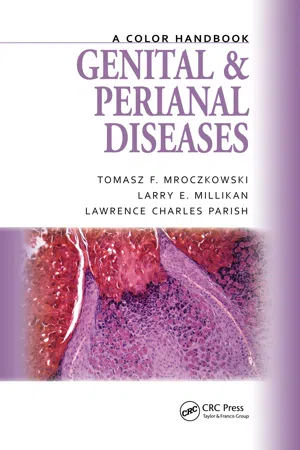
The primary infection usually appears after an incubation period, ranging from 10 to 90 days, with an average of 3 weeks. The initial lesion or ‘primary chancre’ appears at the point of inoculation, which is most commonly the genitals or anus. The first sign may be a dusky, red macule, which quickly develops into a pinkish papule and then a painless chancre with an ulcerated center (1.1). The classical chancre is usually solitary, regular in shape, round or oval, with clearly defined, raised, smooth borders, surrounded by a dull red areola or even normal skin (1.2). The base is finely granular, glistening, and clean (1.3), unless secondarily infected. On palpation, the base of the ulcer has hard button-like or cartilaginous induration. Squeezing or abrading the ulcer produces a serous or yellowish exudate containing spirochetes. The chancre of syphilis is painless, unless secondarily infected. In heterosexual men it is most commonly found on the penis (1.4), while in homosexual men, the anus (1.5), rectum, or mouth, and in women the labia and the cervix (1.6). Extragenital lesions are most commonly found in the oral cavity and on fingers. Multiple or erosive primary lesions are rare but do occur in men with concurrent HIV infections and in chronic alcoholics. Without treatment, the lesion usually heals spontaneously in 2–6 weeks, leaving a thin atrophic scar which, in many instances, becomes barely visible.

1.2 Classical primary chancre on the glans of penis.

1.3 Classical primary chancre.

1.4 Primary chancre on the penis.

1.5 Primary chancre in the anus.
1.6 Primary chancre on the labium.
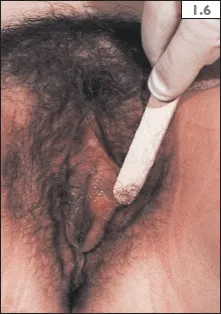
Unilateral or bilateral inguinal lymphadenopathy follows the primary chancre on the genitalia within a few days (1.7). The enlarged nodes are firm on palpation, movable, and separate from one another, and the skin over them is not reddened. Such nodes are usually painless and do not suppurate. In women, the femoral nodes may also be involved.
COMPLICATIONS
In uncircumcised men, the most common complication is phimosis, when as a result of edema, the foreskin cannot be retracted behind the coronal sulcus. The other frequent complication is paraphimosis, when the retracted foreskin cannot be returned to its normal position. In circumcised patients, secondary infection may cause painful edema of the penile shaft and tender lymphadenopathy. Rare complications include Follman’s balanitis, a superficial infection of the glans of penis, caused by T. pallidum itself.
In women, the most common complication is edema of the labium, at the site of the primary chancre.
DIAGNOSIS
The diagnosis of primary syphilis is based upon the clinical features (painless ulcer with regional lymphadenopathy), supported by the presence of T. pallidum on dark-field microscopic examination. Venereal Disease Research Laboratory (VDRL) and rapid plasma reagin (RPR) serologic tests are reactive in primary syphilis approximately 60–90% of the time, and the fluorescent treponemal antibody absorbtion test (FTA-Abs) or the new immunoassays, e.g. TREP-SURE, 86–100%. Serologic tests are more likely to be nonreactive if the chancre has been present shorter than a week.
1.7 Unilateral inguinal lymphadenopathy due to primary syphilis.
DIFFERENTIAL DIAGNOSIS
The primary chancre in the genitals should be distinguished from: genital herpes, chancroid, lymphogranuloma venereum (LGV), Donovanosis (see Table 3.1, p. 34), Behçet’s syndrome, carcinoma, traumatic lesions, or other infection, either bacterial or fungal in origin.
An extragenital chancre may be mistaken on the lips for herpes labialis (1.8), carcinoma, aphthous ulcer, or angular cheilitis; on the tongue for aphthous ulcer, squamous cell carcinoma, or tuberculosis; on the fingers for herpetic whitlow, paronychia, or traumatic abrasion; and in the anorectal region for hemorrhoids, anal fissure, carcinoma, rectal warts, and Bowen’s disease.

1.8 Primary chancre on the inner site of the lower lip. (Courtesy of Dr. Tomasz F. Mroczkowski.)
Secondary syphilis

Signs and symptoms of secondary syphilis commonly appear 6 weeks to 6 months after the initial infection; however, the eruption may follow the primary lesion as early as several days or with a delay of several months. At this stage, there may be multiple skin findings and/or a wide range of systemic involvement. In addition to cutaneous manifestations (the hallmark of secondary syphilis), patients may develop constitutional, flu-like symptoms which precede or accompany the first skin signs, with complaints of malaise, headache, muscular and joint aches, sore throat, hoarseness, and a low-grade fever. With these symptoms, generalized lymphadenopathy is frequently present. Some patients may have an enlarged liver and/or spleen.
Although constitutional and other signs may be present, the diagnosis of secondary syphilis is suspected primarily on the basis of the skin and mucous membrane lesions, which have certain common characteristics, allowing the physician to distinguish them from other skin diseases. One must always remember that the diagnosis of secondary syphilis must not be made on clinical grounds only and should be confirmed by serologic tests6.
TYPES OF SKIN LESIONS
Macular eruption (roseola syphilitica)
The earliest cutaneous expression of secondary syphilis is a macular (roseolar) eruption, which usually appears 5–8 weeks after the primary chancre. It is first seen on the side of the trunk and later involves the chest, abdomen, and shoulders (1.9). The arms and legs are frequently affected, with the flexor surfaces being the sites of predilection. The macular eruption may be limited to the trunk or be generalized, but the palms, soles, and the face are usually spared except for a few lesions around the mouth. Because the macular eruption may be very discrete, it is best seen in natural daylight or with oblique artificial illumination. It usually disappears within a few days, but in rare instances it may persist and develop into a papular eruption. In pigmented patients, the roseolar eruption may leave slight postinflammatory pigmentation resembling tinea versicolor, which lasts for only a few days.

1.9 Discrete macular eruption in secondary syphilis.
Maculopapular eruption
The maculopapular eruption is the hallmark finding of early secondary syphilis. It usually appears 2–4 months after infection. The eruption is generalized, involving the face, trunk, flexor surfaces of arms, and to a lesser extent, the extremities. The symmetric involvement of the palms and soles is characteristic (1.10–1.12). In this location, the papular lesions remain flat or may be only slightly elevated due to the pressure and the horny characteristics of the epithelium. Slight scaling may be present.
Papular eruption
This type of eruption, along with maculopapular eruption...
Table of contents
- Cover
- Title Page
- Copyright
- Contents
- Preface
- Contributors
- Abbreviations
- SECTION 1 SEXUALLY TRANSMITTED DISEASES
- SECTION 2 CUTANEOUS DISEASES OF THE ANOGENITAL REGION
- References
- Index