eBook - ePub
Textbook of the Neurogenic Bladder
- 839 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Textbook of the Neurogenic Bladder
About this book
The editors of this comprehensive third edition of the Textbook of the Neurogenic Bladder have assembled an impressive team of world specialists to develop an essential resource for physicians, continence specialists, and other health care professionals involved in the diagnosis and management of patients who have lost normal bladder function.The b
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Textbook of the Neurogenic Bladder by Jacques c, David Ginsberg, Gilles Karsenty, Jacques c,David Ginsberg,Gilles Karsenty,Jacques Corcos in PDF and/or ePUB format, as well as other popular books in Medicina & Teoria, pratica e riferimenti medici. We have over one million books available in our catalogue for you to explore.
Information
Topic
MedicinaPart I
The normal genitourinary tract
1
Simplified anatomy of the vesicourethral functional unit
Introduction
The bladder and urethra should necessarily be described together. Functionally, these two organs cannot be dissociated and, anatomically, their connections are too imbricated to distinguish them as two different organs. The pelvic floor, with its muscles, fascia, and ligaments, is a separate anatomic entity, but, functionally, it is also an important component of urethra–vesical physiology.1
The bladder
The bladder (Figure 1.1), located in the pelvis behind the pubic bone, can be divided into two portions. The dome, the upper part of the bladder, is spherical, extensible, and mobile. The median umbilical ligament (urachus) ascends from its apex behind the anterior abdominal wall to the umbilicus, and the peritoneum behind it creates the median umbilical fold. In males, the superior surface of the dome is completely covered by the peritoneum extending slightly to the base. It is in close contact with the sigmoid colon and the terminal coils of the ileum. In females, the difference arises from the posterior reflection of the peritoneum on the anterior face of the uterus, forming the vesico–uterine pouch. In both sexes, the inferolateral part of the bladder is not covered by the peritoneum. In adults, the bladder is completely retropubic and can be palpated only if it is in overdistension. In contrast, at birth, it is relatively high and is an abdominal organ. It descends progressively, reaching its adult position at puberty.
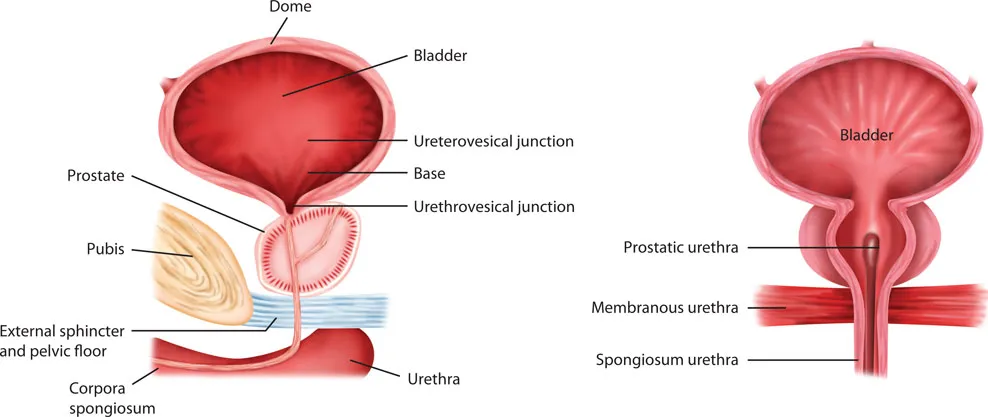
Figure 1.1
Anatomy of the vesicosphincteric unit in man. (a) Sagittal view and (b) frontal view.
Anatomy of the vesicosphincteric unit in man. (a) Sagittal view and (b) frontal view.
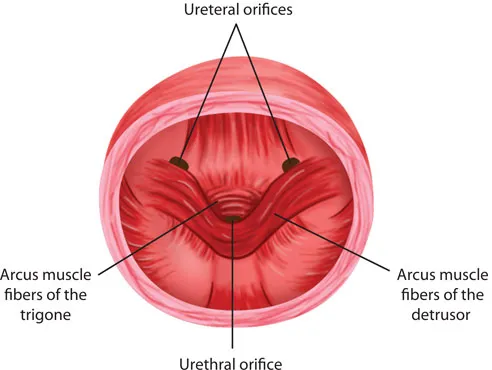
Figure 1.2
Trigone endovesical view.
Trigone endovesical view.
The base of the bladder, i.e., the lower part, is fixed. The trigone, at the post part of the bladder base, is a triangular area between three orifices: two ureteral orifices and a urethral orifice or bladder neck.
At the level of the vesicourethral junction, the ureters cross the bladder wall obliquely in a length of 1–2 cm. This type of path through the bladder wall creates a valve mechanism, preventing urine reflux toward the ureters when bladder pressure increases. This is achieved by the fact that the ureter pierces the bladder wall obliquely. As the ureter passes through a hiatus in the detrusor (intramural ureter), it is compressed and closed completely by detrusor contraction. This intravesical portion of the ureter lies immediately beneath the bladder urothelium, and, therefore, it is backed by a strong plate of detrusor muscle. It is believed that with bladder filling, this results in passive occlusion of the ureter, like a flap valve.
At the level of the vesicourethral junction or bladder neck, the original disposition of the muscle fibers allows closure during the bladder-filling phase (Figure 1.2).
Detrusor muscle
The detrusor muscle can be described as a sphere of smooth muscle bundles. It is a complex imbrication of smooth muscle fibers without a well-defined orientation, but is usually viewed as an external and internal longitudinal layer with a circular intermediate layer. These layers are inseparable in the upper aspect of the bladder. On the other hand, near the bladder neck, they are clearly separable into the three layers mentioned earlier. In men and women, the muscle fibers of the inner longitudinal layer extend down into the urethra in a funnel-shaped structure, allowing continence and emptying of the bladder. In men, the middle circular layer forms a circular preprostatic sphincter, which is responsible for continence, as it forms a ring-like structure at the level of the bladder neck. The outer longitudinal layers are thickest posteriorly at the bladder base, providing a strong trigonal support. Laterally, fibers from this sheet pass anteriorly and fuse to form a loop around the bladder neck, participating in the continence mechanism.
The female bladder neck, on the other hand, differs from that of the male in that its sphincteric function is limited. Some authors have denied its existence altogether.2
Bladder mucosa
The bladder mucosa, folded when the bladder is empty, is loosely adhered to the submucosal tissue and the detrusor. Over the trigone and all around the bladder neck it becomes much more adhered. The bladder mucosa is richly vascularized and very sensitive to pain, distention, temperature, and so on.
Deep to this, the lamina propria forms a relatively thick layer of fibroelastic connective tissue that allows considerable distension. This layer is traversed by numerous blood vessels and contains smooth muscle fibers collected into a poorly defined muscularis mucosa. Beneath this layer lies the smooth muscle of the bladder wall.
Urethral orifice
The urethra Female urethra
The female urethra is 4 cm long and approximately 6 mm in diameter. It begins at the internal vesical orifice, extends downward and forward behind the symphysis pubis, and terminates at the external urethral meatus about 2 cm behind the glans clitoris. The urethral mucosa is surrounded by a rich, spongy, estrogen-dependent submucosal vascular plexus encased in fibroelastic and muscular tissue. The outer layer of the female urethra, covered two-thirds of its proximal length by a striated muscle, represents the external urinary sphincter. This sphincter has its largest diameter in the middle part of the urethra. The striated urogenital sphincter has two distinct portions: the upper portion, which is arranged circularly around the urethra, corresponds to the rhabdosphincter, whereas the lower portion comprises arch-like muscular bands (Figure 1.3). Many small mucous glands open into the urethra, forming what are called the paraurethral ducts, which are usually located on the lateral margin of the external urethral orifice.2
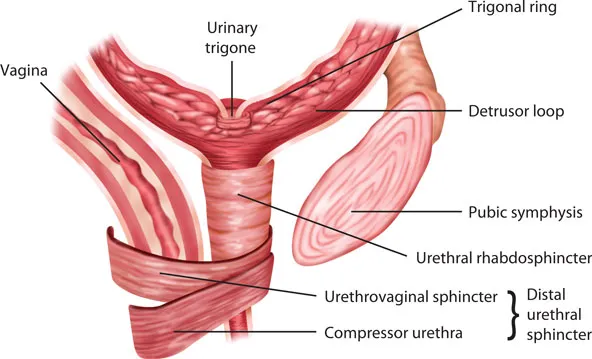
Figure 1.3
Architectural organization of the striated urethral sphincter. Location of its three components: the urethral rhabdosphincter, the compressor urethra, and the urethrovaginal sphincter.
Architectural organization of the striated urethral sphincter. Location of its three components: the urethral rhabdosphincter, the compressor urethra, and the urethrovaginal sphincter.
Male urethra
The male urethra (see Figure 1.1a,b) is 18–20 cm long and is usually divided into three portions: the proximal or prostatic urethra, the membranous urethra (both included in the posterior urethra), and the anterior urethra (composed of bulbar, pendulous urethra, and fossa navicularis).3,4
• The first segment (3–4 cm) is mainly a thin tube of smooth muscle lined by mucosa and extending through the prostate from the bladder neck to the apex of the prostate. At the origin of the prostatic urethra, the smooth muscle surrounding the bladder neck is arranged in a distinct circular collar, which becomes continuous distally with the capsule of the prostate. The internal sphincter extends from the internal vesical meatus through the prostatic urethra to the level of the verumontanum, providing passive continence via the sympathetic supply. The prostatic urethra ends distal to the verumontanum.
• The second segment, erroneously called the membranous urethra (there is nothing membranous at that level), is also known as sphincteric urethra. The external sphincter has an omega shape and surrounds the urethra with a fibrotic segment in its posterior midline. It is 2 cm long and 3–5 mm in thickness. It has an outer layer of striated muscle and an inner layer of smooth muscle, intrinsic to the urethral wall, making it both a voluntary and an involuntary unit. Surrounding the external sphincter is a layer of periurethral striated muscle fibers, providing assistance in voluntary control (i.e., interruption of voiding).
• The last segment, the spongiosum urethra, is contained in the corpus spongiosum of the penis and extends from the previous segment to the urethral meatus. Its diameter is 6 mm when passing urine. It is dilated at its commencement to form the intrabulbar fossa and again within the glans penis, where it becomes the navicular fossa. All along the urethra, numerous small mucous glands (urethral glands) open into its lumen.
Vascular and lymphatic supply of the bladder and urethra
The superior and inferior vesical arteries are branches of the internal iliac arteries. The obturator and gluteal arteries also participate in the bladder arterial supply. In females, an additional branch is derived from the uterine and vaginal arteries. Venous drainage forms a complex, extensive network around the bladder and into a plexus on its inferolateral face, ending in the internal iliac veins.
Lymphatic drainage originates from all layers of the bladder and ends in the external iliac nodes. Most urethral lymphatic drainage terminates in the external iliac nodes, except for the spongiosum urethra and the glans penis where it goes to the deep inguinal nodes and from there to the external iliac nodes.3
Urethrovesical unit innervation
Three nerves provide an anatomic and somatic innervation to the bladder (Figure 1.4).5, 6, 7
Hypogastric nerve
The hypogastric nerve has motor and sensory fibers. It originates from preganglionic spinal neuron...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Introduction
- List of contributors
- Part I The normal genitourinary tract
- Part II Functional pathology of the lower urinary tract
- Part III Neurologic pathologies responsible for the development of the neurogenic bladder
- Part IV Evaluation of neurogenic bladder dysfunction
- Part V Classification
- Part VI Treatment
- Part VII Special considerations on meningomyelocele
- Part VIII Synthesis of treatment
- Part IX Complications
- Part X Sexual dysfunction in neurologic disorders
- Part XI Prognosis and follow-up
- Part XII Reports and guidelines
- Index