eBook - ePub
Vagus Nerve Stimulation
- 184 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Vagus Nerve Stimulation
About this book
This second edition presents a timely and practical discussion of vagal nerve stimulation in a clear and well-illustrated format. It provides a clinical approach to the treatment of patients with medically-intractable seizures, as well as for those with depression (a new indication since the publication of first edition). The book's focus has made it successful, as it zeros in on clinically relevant findings. The new edition includes downloadable resources with actual footage of the implantation procedure and the latest research findings of the treatment potential for depression and obesity. Vagus Nerve Stimulation gives the attending neurologist step-by-step information on this exciting method of treating epilepsy.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Topic
MedicinaSubtopic
Neurologia1
Vagus nerve stimulation for epilepsy: anatomical, experimental and mechanistic investigations
Thomas R Henry
Introduction
Vagus nerve stimulation (VNS) is the most widely used non-pharmacological treatment for drug-resistant epilepsy. Experiments in animal models of epilepsy and observations in human epilepsies demonstrate three temporal profiles of VNS antiseizure effects: (1) acute abortive effect, in which an ongoing seizure is attenuated by VNS applied during the seizure; (2) acute prophylactic effect, in which seizures are less likely to occur within minutes after a train of VNS than they would be in the absence of VNS, an effect that begins as soon as VNS is initiated; and (3) chronic progressive prophylactic effect, in which overall seizure frequency is reduced more after chronic VNS over weeks or months than occurred due to acute abortive and prophylactic effects. The mechanistic studies and clinical trials of VNS support regulatory approvals internationally, and provide greater information concerning VNS than is available for any other non-pharmacological epilepsy therapy. The mechanistic investigations of VNS, which are the subject of this chapter, and the extensive clinical investigations and applications reviewed in subsequent chapters, justify consideration of VNS as a new epilepsy therapy.
A confluence of experimental and human data indicate that antiseizure actions of VNS are entirely based on alterations in brain function mediated through vagal afferents, with no participation of vagal visceroeffector activities. Vagal efferents underlie some of the common adverse effects of VNS, however. This chapter will first review the peripheral and central anatomy of the vagus and related systems, followed by considerations of experimental and clinical investigations of VNS mechanisms in the epilepsies.
Vagus nerve: course and composition
The vagus nerves carry somatic and visceral afferents and efferents. Most of the efferent fibers originate from neurons located in the medulla oblongata. Vagal efferents innervate striated muscles of the pharynx and larynx, and most of the thoracoabdominal viscera.1,2 The two vagus nerves coalesce from multiple rootlets at the medulla, exit the skull in the jugular foramina, and traverse a long and winding route throughout the viscera. This complex and wide distribution earned the vagus nerve its name, as the Latin for ‘wanderer.’
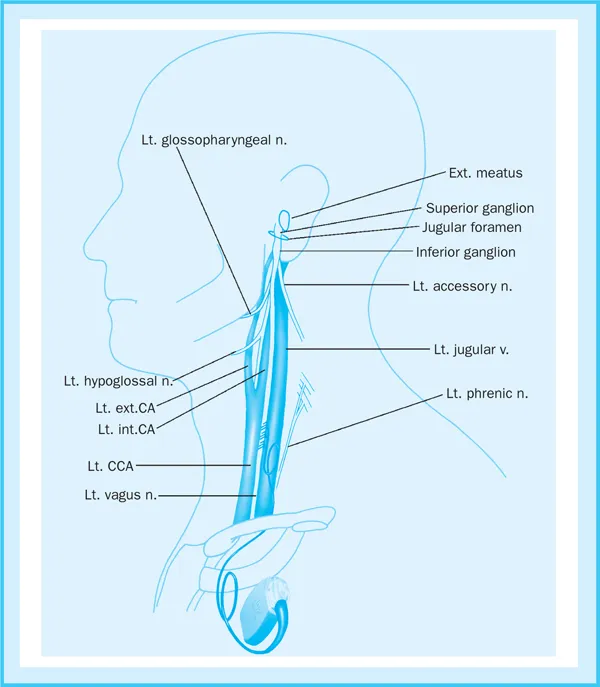
Each vagus nerve lies between the carotid artery and the jugular vein in the neck, within the carotid sheath (see Figure 1.1). In the cervical portion of the vagus nerve, unmyelinated, narrow-caliber C-fibers predominate over faster conducting, myelinated, intermediate-caliber B-fibers and thicker A-fibers.3 Afferents compose about 80% of the fibers in the cervical portion of the vagus.4 Most of the neurons that contribute afferent fibers to the cervical vagus have cell bodies located in two parasympathetic ganglia, the superior (jugular) vagal ganglion and the larger inferior (nodose) vagal ganglion, which are located at and immediately below the jugular foramen. A large population of special and general visceral afferents carry gustatory information, visceral sensory information, and other peripheral information. A limited number of vagal somatosensory afferents carry sensory information from skin on and near the ear.
Vagus nerve efferents
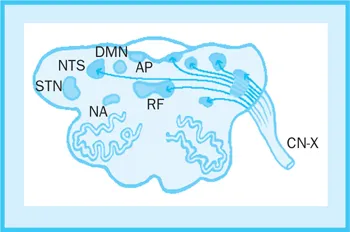
Most vagal efferents are parasympathetic projections to the heart, lungs, stomach and intestines, liver, pancreas, and kidneys. These efferents originate from preganglionic neurons of two pairs of nuclei in the medulla, the dorsal motor nucleus of the vagus and the nucleus ambiguus (see Figure 1.2). Vagal parasympathetic efferents synapse on neurons located in parasympathetic ganglia, which are located in or near the target organs. The vagus nerves are asymmetric with regards to cardiac innervation. The left vagus nerve carries most of the parasympathetic fibers that less densely innervate the ventricles, and the right vagus nerve carries most of the parasympathetic fibers that more densely innervate the cardiac atria.5 Thus, vagal anatomy favors left (over right) vagus stimulation in order to avoid effects on cardiac rhythm. Actual measurements of cardiac rhythm with Holter monitoring, of respiratory function with pulmonary function tests, and of gastrointestinal parasympathetic effects with serum gastrin levels, show remarkably little vagal visceroeffector activity during therapeutic VNS in humans.6–12 In one report, decreased myocardial contractility occurred in humans during intraoperative stimulation of distal branches of the vagus,9 but stimulation at this site appears to have limited relevance to cervical vagus stimulation. Cases of altered cardiac rhythm and altered respiration during cervical vagus stimulation have been reported to occur only during unusual states of intervention such as general anesthesia,12 in patients with obstructive sleep apnea,11 or in the absence of clinical manifestation.10 As a group, these studies raise concern over possible adverse effects of VNS that may be specific to particular non-epileptic medical conditions involving viscera that receive vagal innervation. With the exception of obstructive sleep apnea, which has been the subject of one pilot study in patients receiving VNS,11 VNS has not been studied in series of patients with cardiac arrhythmias, congestive heart failure, or other dysfunctions of vagally innervated organs.
Vagal branchiomotor efferents synapse as motor end plates on skeletal muscle fibers of the larynx and pharynx. The alphamotoneurons of these efferent axons are located in the nucleus ambiguus of the medulla. Each vagus nerve contains efferents that innervate the vocal cord and other skeletal muscles of the larynx and pharynx unilaterally. Volitional swallowing does not appear to be affected by VNS using typical stimulation parameters, except for anecdotal reports of aspiration in children with severe cognitive and motor delay, when assisted feeding is performed during VNS. Vocalization is commonly altered by VNS, however. After upwards titration of current output, vocal stridor typically occurs during each train of stimulation.6,13 VNS-induced vocal stridor is promptly reversible with a reduction in current density.
Afferent terminations and central pathways of the vagus nerve
Vagal afferent fibers enter the dorsolateral medulla and traverse the brainstem in the solitary tract. Most vagal afferents synapse in nuclei of the dorsal medullary complex of the vagus,14–16 which includes the following structures of the medulla (see Figure 1.2):
- nucleus of the tractus solitarius (NTS);
- nucleus of the spinal tract of the trigeminal nerve;
- medial reticular formation of the medulla;
- area postrema;
- dorsal motor nucleus of the vagus;
- nucleus ambiguus.
The NTS receives the greatest number of vagal afferent synapses and each vagus nerve synapses bilaterally on the NTS. Each vagus nerve synapses only ipsilaterally in the other nuclei of the dorsal medullary complex of the vagus. The vagal afferents subserve visceral sensation (of the pharynx, larynx, trachea, and thoracoabdominal organs), somatic sensation (of a small patch of skin on and near the external ear), and taste (with receptors in the periepiglottal pharynx).
Vagal afferent synapses use the usual excitatory neurotransmitters (glutamate and aspartate) and inhibitory neurotransmitter (gamma-aminobutyric acid; GABA), and also use acetylcholine and a wide variety of neuropeptides.17,18 As a group, these transmitters and modulators act very rapidly at neuronal membrane ion channels, and act more slowly via intraneuronal second messengers such as G-proteins.
NTS
The NTS extends as a tube-like structure above and below the vagal entry level, within the dorsal medulla and pons. In addition to dense innervation by the vagus nerves, the NTS also receives projections from a very wide range of peripheral and central sources.1,2,15,19 These sources of afferents to the NTS include other peripheral nerves (the carotid sinus nerve, the aortic depressor nerve, and cranial nerves V, VII and IX), the spinal cord (via the spinosolitary tract), multiple brainstem structures (the area postrema, the rostral ventrolateral medulla, the parabrachial nucleus of the pons, the Kölliker-Fuse nucleus, the dorsal tegmental nucleus of the midbrain, and other sites), and cerebral structures (the paraventricular nucleus, lateral and posterior regions of the hypothalamus, and the central nucleus of the amygdala).
The NTS receives a wide range of somatic and visceral sensory information, receives projections from a diverse set of brainstem nuclei and cerebral structures, performs extensive information processing internally, projects to multiple hindbrain and forebrain structures, and produces motor and autonomic efferent outputs. For these reasons the NTS has been likened to a small brain within the larger brain. The vagus and associated sensory endings are the principal sensory organ of this small brain within a brain.
Vagal networks of the pons, midbrain, and cerebellum
Vagal afferents influence activities throughout a network of posterior fossa sites, with polysynaptic connections through the NTS and other nuclei. The NTS projects to a wide variety of structures within the posterior fossa,1,2,20,21 as shown schematically in Figure 1.3, including all of the other nuclei of the dorsal medullary complex, the parabrachial nucleus and other pontine nuclei, the vermis and inferior portions of the cerebellar hemispheres, and the periaqueductal gray.
The NTS projects to the parabrachial nucleus of the pons most densely, and particular NTS subregions project specifically to different subnuclei of the parabrachial nucleus. Through disynaptic parabrachial relay projections, the NTS can influence activities of respiratory pattern generation and pain modulation. Alterations in the respiratory pattern are not commonly observed during VNS, although patients with obstructive sleep apnea may in some cases experience increased apneas and hypopneas while asleep during high-frequency VNS.11
The periaqueductal gray is involved in central pain processing, and local alterations in processing during VNS may underlie antinociceptive effects of VNS in humans.22 Through its own monosynaptic projections, the NTS can directly influence reflexes involving parasympathetic and sympathetic effector neurons, cranial nerve alphamotoneurons, motor systems subserving posture and coordination, ascending visceral and somatic sensory pathways, and the local arousal system.
The area postrema also receives afferent synapses from the...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Contributors
- Foreword
- 1 Vagus nerve stimulation for epilepsy: anatomical, experimental and mechanistic investigations
- 2 Surgical technique in vagus nerve stimulation
- 3 Vagus nerve stimulation: efficacy, safety and tolerability, in patients with epilepsy
- 4 Potential mechanisms of action of vagus nerve stimulation for depression
- 5 Vagus nerve stimulation: clinical results in depression
- 6 Vagus nerve stimulation in the treatment morbid obesity
- 7 Vagus nerve stimulation in the current treatment of epilepsy
- 8 Practical considerations: vagus nerve stimulation therapy questions that may be encountered from patients, their caregivers, and physician colleagues
- Glossary
- Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Vagus Nerve Stimulation by James Robertson,Claude Roux,Kenneth G. Wiggins, Steven C. Schachter,Dieter Schmidt, Steven C. Schachter, Dieter Schmidt in PDF and/or ePUB format, as well as other popular books in Medicina & Neurologia. We have over one million books available in our catalogue for you to explore.