Applied Population Health
Delivering Value-Based Care with Actionable Registries
- 286 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Applied Population Health
Delivering Value-Based Care with Actionable Registries
About this book
Electronic Health Record (EHR) systems today provide increasing levels of clinical decision support and are the fulcrum for change for value-based healthcare delivery. Billions of dollars of government and insurer payments are dependent on evidence-based workflow design and quality report. In this context, quality measurement is no longer a retrospective exercise, but an essential prospective process embedded in clinical operations. Population health tools in the EHR enhance the efficiency and effectiveness of interventions thus improving the quality of care at lower cost. Population health methods are effective in ensuring that the right patient receives the right care at the right time.
This book provides a clear framework for design, implementation, and monitoring of innovative population health tools to accelerate measurable improvements in care delivery. Key benefits for readers include conceptual framework, team approach, and technical insights that result in improved patient care, improved performance on quality measures and increased revenue from quality performance incentives and risk-based contracts. This is also a practice guide to the healthcare professionals many roles who are eager to build or improve population health programs with the goal of delivering high quality value-based care.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Chapter 1
Introduction
Part 1: Fundamentals
| Policy | A brief history of the U.S. policies driving value-based payment models Quality measure use in pay-for-performance and risk sharing programs Value-based measurement framework |
| People | Organizational characteristics Stepping stones to value-based care Value improvement governance structure Patient empanelment and attribution to define doctor–patient relationships |
| Understanding patients and patient groups Social determinants of health New standards for race, ethnicity, and language (REAL) Data collection for sexual orientation and gender identity (SO/GI) |
| Process | Sample population health protocol Technology flaws underlying healthcare waste |
| Technology | Introduction to the role of registries in value-based care delivery Taxonomy and ontology of health registries |
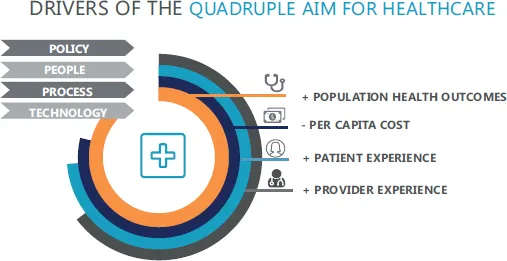
| Measuring the quadruple aims | Population health outcomes Per capita cost Patient experience Provider experience |
| Case studies | Provider engagement practices Collection of ethnic background data Doing the right thing with medication monitoring Use of Social Security decedent data in EHR registry |
Part 2: Effective Delivery of Applied Population Health
- Identify the quality measure(s) to target for change
- Build the registry with data elements needed for the measure calculations
- Add clinical decision support and supporting workflows to drive performance
- Build real-time dashboards for continuous process measurement
| Conceptual model | Applied population health technical foundation |
| Prototype system | Do-it-yourself quality measure management |
| Registry design principles | Transitioning from quality measures to registries |
| Second-generation clinical decision support | EHR tools that use the registry engine to drive care |
| Analytics dashboards | Innovative application of dashboards to: Track rolling performance measures in real time (365 day lookback) Demonstrate utilization and value of technology Co-locate quadruple aim outcomes |
Table of contents
- Cover
- Half Title
- Title
- Copyright
- Contents
- List of Tables
- List of Figures
- Acknowledgements
- About the Authors
- 1 Introduction
- Part 1 Fundamentals
- Part 2 Effective Delivery of Applied Population Health
- Part 3 Applied Population Health Today and Tomorrow
- References
- Answer Key
- Appendix A. Implementation of CDC Race and Ethnicity Codes (CDCREC)
- Appendix B. Population Health White Paper
- Appendix C. Job Descriptions for Population Health Team Members
- Appendix D. DIY System for Quality Measure Management
- Appendix E. Ambulatory Care Health Screening Order Protocol
- Appendix F. Population Health Project Request
- Appendix G. Registry Best Practices
- Appendix H. Resources
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app