![]()
Chapter 1
An introduction to evidence-informed nursing
Robert McSherry, Maxine Simmons and Paddy Pearce
CONTENTS |
What is evidence-informed nursing? | |
How does it relate to clinical effectiveness and evidence-based practice? | |
Implementing evidence-informed practice | |
1 Clinical expertise |
2 Knowledge of research evidence |
3 An understanding of patient preference and choice |
4 Access to adequate resources |
Strengths of evidence | |
References | |
What is evidence-informed nursing?
Nurses are responsible for the care they provide for their patient. They have to be active, competent and autonomous in providing this care and be able to justify what they do. It is no longer acceptable for nurses to base care on ritual and tradition – they must be able to justify the decisions they have made about appropriate care and treatment on the basis of a professional expertise which includes using research evidence to inform practice.
This book aims to enhance your understanding of, and to subsequently support you in practising, evidence-informed nursing. We use the term ‘evidence-informed nursing’ in preference to ‘evidence-based nursing’ in order to recognise that nurses are critical practitioners. It must be sound and relevant research that informs practice. Nurses need to know and understand how to access and use research and how to incorporate it effectively into their everyday practice. They need to acquire and become competent in the skills of research awareness, critical appraisal, reflective practice and decision-making (McSherry 1997). Evidence-informed nursing is the development of a professional practice in which the nurse does something not just because that is how it has always been done or because that is what she/he was told to do, but because she/he has made ‘. . . a decision for actions which can be justified from a knowledge base’ (Marks-Marrah 1993: 123).
This chapter sets the scene by looking at the rationale behind the use of evidence in nursing and at some key definitions and processes associated with it. The following chapters will systematically help you to develop the skills highlighted here as essential to the practice of evidence-informed nursing.
The main imperative for evidence-informed nursing is to ensure the highest possible level of patient care. At the same time proper use of evidence supports nurses in accounting for what they do. Over the last decade there have been significant changes in the expectations placed on nurses by government, employers and the public, with the aim of improving the quality of patient care and achieving clinical excellence. Nurses are accountable to all these groups of people and also to their professional body. A central argument of this book is that a core element of professional nursing is accountability. We recognise, however, that basing practice on evidence is only one element of accountability. Nurses are employed as experts – they are paid to practise on the basis that what they do is well-judged, appropriate and based on an informed appraisal of alternatives. The objective is defensible practice. Nurses should therefore be critical practitioners. Ann Brechin (2000) has indicated that critical practitioners:
conceptualise practice as an open-minded reflective process, build on a sound skills and knowledge base, but taking account of different perspectives, experiences, assumptions and power relations. Critical practice draws on an awareness of wider ethical dilemmas, strategic issues, policy frameworks and social–political context. It acknowledges that there may be no straight forward and ‘right answer . . .’
(Brechin 2000: 11)
and
critical practitioners must be skilled and knowledgeable and yet open to alternative ideas, frameworks and belief systems, respecting and valuing alternative perspectives
(Brechin 2000: 44)
A knowledge and understanding of the relevant research that supports clinical and other nursing practice is only one element of being a critical practitioner, but it is a fundamental one. Evidence-informed nursing is concerned with providing clinically effective patient care and being able to justify the procedures used, the care plan devised or the services provided by reference to authoritative evidence. It is the making of decisions about the care of individual patients and families, on the basis of the best available evidence. French has suggested that it is:
the systematic interconnecting of successfully generated evidence with the tacit knowledge of the expert practitioner to achieve a change in a particular practice for the benefit of a well-defined client/patient group.
(French 1999: 74)
In other words, evidence-informed nursing is the integration of professional judgement and research evidence about effectiveness of interventions. It provides a sound and rational basis for the decisions taken about patient care by nurses. It requires ‘knowledgeable doers’, who have the skills and expertise to implement new procedures and policies and who can supervise others involved in providing care to ensure that they carry out procedures in the most appropriate way. (Not everyone involved in delivering patient care needs to have the sort of skills and knowledge referred to here, but they are essential for anyone involved in the management of the care.) Evidence-informed nursing is a systematic approach to providing nursing care that requires critical appraisal skills. While research evidence on effectiveness is important, it does not require all nurses to be researchers. What it requires is that all nurses have:
an understanding of the importance of practice being based on the most appropriate evidence on effectiveness;
access to and the ability to use research findings;
the ability to evaluate research;
the ability to implement research findings in their own practice.
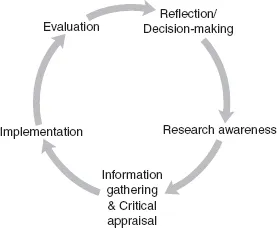
Figure 1.1 The evidence-informed nursing cycle.
Note
Fig. 1.1 demonstrates the cyclical process of how to inform nursing practice with evidence. The process requires reflection on practice, awareness of research, an ability to gather and critically review the evidence, implement the evidence into practice and evaluate the effectiveness of the change in practice. This process subsequently begins again by encouraging the nurse to reflect on the evaluation prompting further decision-making or actions.
Box 1.1 Evidence-informed nursing
requires:
the formulation of answerable questions that arise from practice –
reflection;
the searching of the literature or other relevant evidence sources –
information;
the evaluation of the evidence for validity, generalisability and transferability –
appraisal;
the use of the best available evidence alongside clinical expertise and patient preferences in planning care –
implementation;
the evaluation by practitioners of their own professional practice –
evaluation.
The move towards evidence-informed nursing is a move a...