- 1,090 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Inflammatory Mechanisms in Asthma
About this book
This timely volume brings together the latest basic and clinical insights on the cellular and mediator mechanisms involved in the induction and persistence of airway dysfunction of asthma by over 90 experts in the field-paving the way for developing novel and more effective antiinflammatory therapeutic agents and strategies.
Furnishing a comprehensive and up-to-date view of the expanding and interrelated components underlying asthma pathogenesis, Inflammatory Mechanisms in Asthma
Enhanced with over 4700 references, tables, drawings, and photographs, this compelling investigation into the pathophysiology of asthma is an indispensable resource for pulmonologists, physiologists, immunologists, allergists, epidemiologists, biochemists, molecular biologists, and graduate and medical school students in these disciplines.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Inflammatory Mechanisms in Asthma by Stephen Holgate in PDF and/or ePUB format, as well as other popular books in Medicine & Clinical Medicine. We have over one million books available in our catalogue for you to explore.
Information
1
The Pathology of Fatal Asthma
Sir Charles Gairdner Hospital
Nedlands, Western Australia
I. | Introduction |
Descriptions of the macroscopic findings in the lungs of individuals with fatal asthma date back as far as the seventeenth century. In 1883 spirals of mucus occluding airways in such cases were described by Curschmann (1). In their comprehensive review of asthma pathological characteristics and mechanisms, Huber and Koessler (2) in 1922 identified 15 cases in which the microscopic findings in fatal asthma had been described and added 5 cases of their own. In the first quantitative study of asthma pathological features, they compared these cases to a nonasthmatic group using a stratified technique of sampling large and small airways and even considered the confounding effects of muscle spasm on measured airway dimensions. They documented the classic pathological findings in fatal asthma, including overinflated lungs, mucus plugs occluding airway lumens and containing shed epithelial cells and Charcot-Leyden crystals, variable epithelial damage, dilated mucus gland ducts, thickening of the “basement membrane,” infiltration of round cells and eosinophils into the airway wall, and greater thickness of the epithelium, smooth muscle, and airway wall compared to those of nonasthmatics.
A number of qualitative studies (3,4,5,6,7,8,9,10,11,12), including over 550 cases of fatal asthma with postmortem findings, have since been reported and confirm the pathological abnormalities described. Descriptions from the first half of this century have also reported the presence of peripheral edema, right ventricular hypertrophy, emphysema, atelectasis, bacterial and tuberculous infection, and bronchiectasis. Some of these changes probably reflect long-standing severe airway obstruction, the lack of antibiotics and corticosteroids, and the unrecognized effects of smoking cigarettes. Gough (13) showed that although the lungs were hyperinflated in cases of fatal asthma, emphysema, characterized by destuction of alveolar walls, was not present.
The precise definition of subdivisions of the bronchial wall is confounded by the lack of uniformity among groups of anatomists, pathologists, and physiologists (14). For the purposes of this review the airway will be partitioned as follows: the lumen, which includes the mucus layer; the epithelium (or mucosa); the submucosa, which includes all structures bound by the subepithelial basement membrane and the smooth muscle; and the adventitia, which includes structures between the smooth muscle and the outer limit of the loose connective tissue surrounding the airway.
II. | Lumen |
Plugging of airway lumens with tenacious mucus is an almost constant macroscopic and microscopic finding at autopsy in cases of fatal asthma and may extend from the central airways (Fig. 1a–c) to the small airways (Fig. 1d) as far as the respiratory bronchioles (2,3,4,5,6,7,8,9,15,16,17,18,19,20). Cases in which mucus is not found in the airways are rare (15,21). The mucus plugs in fatal asthma contain shed epithelial cells, inflammatory cells, and proteinacious exudate (Fig. 1). The formation of Charcot-Leyden crystals from the degeneration of eosinophils and the presence of lamellae (Fig. 1c) in the mucus (22) suggest that the mucus accumulates over a period of time. Sudden attacks of asthma, severe enough to require intubation, can occur in the absence of intraluminal mucus (23). These episodes are presumably due to excessive airway smooth muscle shortening. It has been estimated that a single outpouring of mucus gland contents is unlikely to cause significant airway obstruction in the absence of any airway smooth muscle shortening (24). Therefore it is likely that pooling of mucus or gradual accumulation of mucus in the airway lumen would be necessary to cause significant airway narrowing. Shortening of the airway smooth muscle greatly exaggerates the effect of intraluminal mucus in causing airway narrowing (24).
Mucus is produced by the goblet cells of the epithelium and by the mucus glands in the deeper layers of the airway wall. The number of goblet cells and the area of mucus glands are increased above normal in cases of fatal asthma (5,25). Aikawa and colleagues (25) found that the degree of mucus plugging of the airway lumen and the number of goblet cells were greater in patients dying of acute, severe attacks of asthma than in those dying of asthma after a long period of hospital admission. The amount of mucus plugging was related to the area of goblet cells within the airway epithelium, but the area of airway wall mucus gland tissue was similar in both groups. The relative contribution of goblet cells and mucus glands to the mucus in the airway lumen is difficult to assess from such studies because the rate and volume of mucus production from these two sources in patients with asthma are poorly understood.
The mucus in cases of fatal asthma is characteristically thick and tenacious, protruding from the cut surface of the lung at postmortem. This property has been attributed to abnormal mucins of high molecular weight, which are not found in normal individuals or in individuals who have cystic fibrosis (26). The mucus does not seem to derive its physical properties from epithelial glycoprotein or large amounts of deoxyribonucleic acid (DNA) (27).
III. | Epithelium |
Epithelial damage and desquamation (Fig. 2) have been described as characteristic features of asthmatic airways at autopsy (2,3,4,5,6,7,8,9,15,16,17,18,20,28,29). However, the degree of epithelial damage that is present is variable and subject to postmortem effects, and the reliability of assessing epithelial structure in autopsy cases remains unclear (30). That epithelial shedding is a feature of asthma is supported by a number of observations. Naylor (31) found clumps of columnar epithelial cells (which he called by the “euphonious and succinct” eponym “Creola bodies”) in the sputa of 42% of 100 asthma patients. They were more frequently seen during an asthma attack and occurred in only 3% of 100 nonasthmatic patients. Shed epithelial cells are found mixed in the deep layers of intraluminal mucus, and their presence in airways where the epithelium is still intact also suggests they have originated elsewhere in the bronchial tree (9) (Fig. 2c). Thomson (32) observed epithelial shedding in addition to thickening of the “basement membrane” and eosinophil infiltration in ciliated respiratory-type epithelium found in an ovarian teratoma of a patient who died of asthma with typical pathological changes observed in the lung.
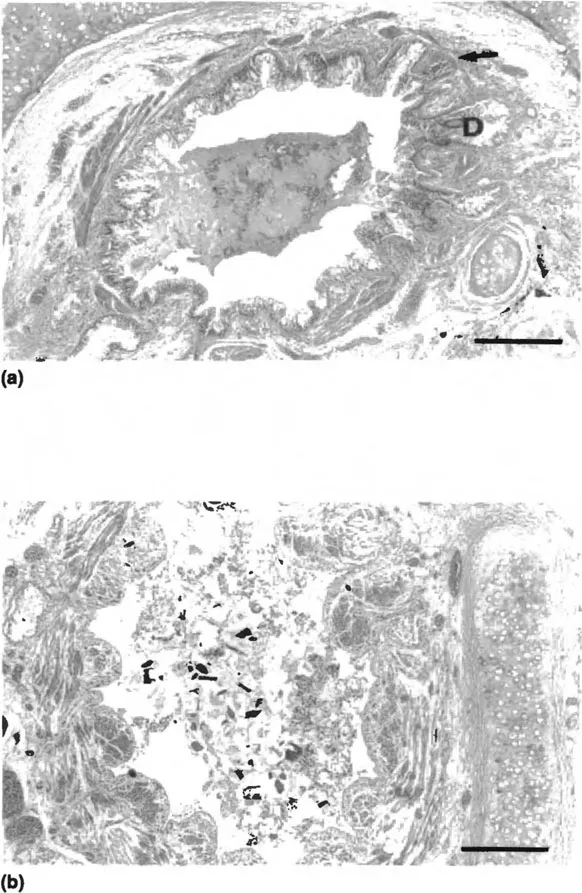
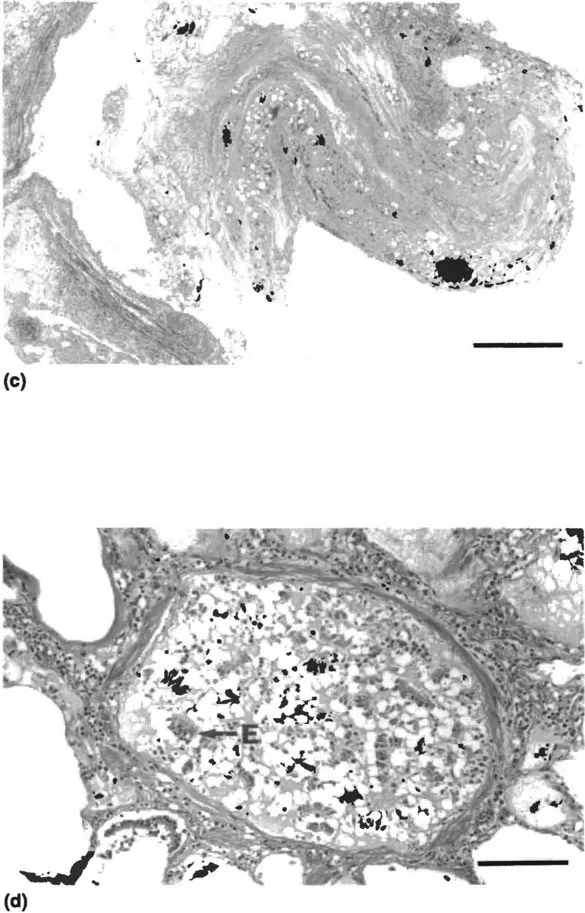
Figure 1 Photomicrographs of airways from individuals with fatal asthma with intraluminal mucus plugs: (a) intact epithelium, thickened “basement membrane,” dilated mucus gland ducts (D), and few cells in the mucus plug, bar = 0.5 mm; (b) loss of epithelium with inflammatory and epithelial cells and cellular debris in the mucus, bar = 0.5 mm; (c) organization and lamination of the mucus plug, bar = 0.2 mm; (d) obstruction of the lumen of a membranous airway with mucus, epithelial cells (E), and inflammatory cells, bar = 0.05 mm.
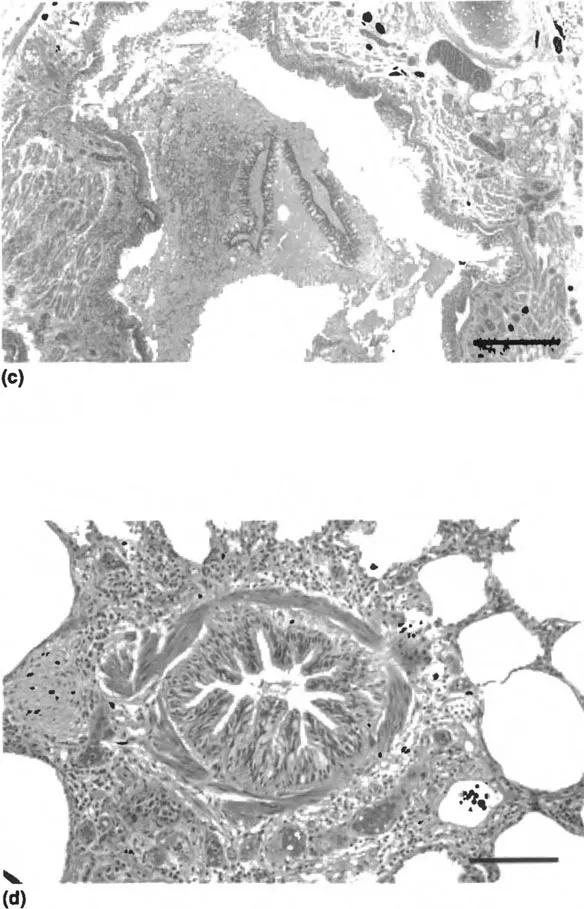
Figure 2 Photomicrographs: (a) normal pseudostratified columnar epithelium from a nonasthmatic individual, bar = 0.05 mm; (b) airway section from case of fatal asthma...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Introduction
- Preface
- Contributors
- 1. The Pathology of Fatal Asthma
- 2. Bronchoscopy
- 3. Bronchoalveolar Lavage in Studies of Asthma
- 4. Evidence from Induced Sputum
- 5. Mast Cell Proteases in Asthma
- 6. Mast Cell Cytokines in Allergic Inflammation
- 7. Airway Responses to Antigen in Asthmatic and Nonasthmatic Subjects
- 8. The Role of the Basophil in the Inflammatory Mechanisms of Asthma
- 9. Eosinophils: Granule Proteins
- 10. Eosinophil Activation in Asthma
- 11. Eosinophil Autacoids
- 12. Eosinophil Cytokines
- 13. Eosinophils in Asthma
- 14. Interactions Between Eosinophils and the Airway Epithelium
- 15. Neutrophils and Asthma
- 16. Allergen Recognition Sites in Immunoglobulin E from Patients with Asthma
- 17. Τ Cells in Asthma
- 18. Macrophages and Macrophage Diversity in Asthma
- 19. Antigen Presentation in the Asthmatic Lung
- 20. Macrophage and Dendritic Cell Populations in Airway Tissues
- 21. Fibroblasts and the Extracellular Matrix in Asthma
- 22. Mediator Functions of Epithelial Cells
- 23. Epithelium as a Target
- 24. Airway Neuropeptides and Their Role in Inflammation
- 25. Neuroimmune Interactions in Airway Inflammation
- 26. Microvascular–Epithelial Exudation of Bulk Plasma in Airway Defense, Disease, and Repair
- 27. Neuroregulation of Mucosal Vasculature
- 28. Leukocyte–Endothelial Adhesion
- 29. Prostanoids
- 30. Leukotrienes
- 31. Adenosine: Its Contribution to Our Understanding of Asthma
- 32. Chemotaxis and Mechanisms of Cell Migration
- 33. Kinins
- 34. The Early and Late Asthmatic Response to Allergen
- 35. Inflammatory Mechanisms of Aspirin-Sensitive Asthma
- 36. Inflammatory Mechanisms in Nocturnal Asthma
- 37. Inflammatory Mediators and Exercise-Induced Asthma
- 38. Mechanisms of Airway Hyperresponsiveness
- 39. Transcription Factors as Activators and Repressors of Gene Transcription: NF-κB and Glucocorticoid Receptors
- 40. Lower Airway Responses to Viruses
- Index