![]()
COMMUNITY AS A SOCIAL WORK
ORIENTATION
Community Based
Rural Health Care in India:
Potential for Social Work Contribution
Sukla Deb Kanango
SUMMARY. India is a large country, geographically as well as populationwise. The majority of its population lives in rural areas, i.e., villages. Again, most of the villages are in remote areas. The State has been making sincere efforts to make the basic social services accessible to all in the rural area. Health being one of the vital services, it has been a challenging task before the State to extend it to the remote rural areas, many of which are not yet connected by motorable roads. As a result of various experiments carried out over the last five decades, the State has developed a fairly well-designed primary health care service, and it is in operation in rural areas. However, there appears to be a striking gap between the delivery of health services in rural areas and utilization of the services by the people. Attempts have been made in this article to apprise the readers of the health service system in India, and it discusses the issue of health service delivery at the village level. The discussion is based on a small study carried out in a rural area in the State of West Bengal (India) where students of social work of the University to which the author belongs are placed for field work. Following the inputs received through supervision of the students’ work, the study was initiated and conducted.
This article based on the study seeks to focus on peoples’ perception of the health services as provided by the State in rural areas, which in turn gets reflected in the extent to which they utilize the services. Social workers being an integral part of the health set up, their role bears special significance. Discussion, therefore, centres on scope for social work intervention at the community level as well as in institutional level of the health service delivery system to make the services meaningful and effective in rural areas. In fact, it has to take the leadership role in reforming the service delivery system when required.
[Article copies available for a fee from The Haworth Document Delivery Service: 1-800-HA WORTH. E-mail address: <[email protected]> Website: <http://www.HaworthPress.com> © 2004 by The Haworth Press, Inc. All rights reserved.]KEYWORDS. Rural, State, Primary Health Centre, development block, health care service, West Bengal, service delivery, village, utilization, student, system, remote
INTRODUCTION
Investment in health is regarded as an important contributing factor to the development of a nation, not only in social terms but also in economic terms. A good health service is an asset of a society. For India, the health sector has been an important area in its total development endeavour. It has also been a serious concern for the State for the following reasons. India has a large population; compared to it the resources required to meet health needs are much less. The bulk of the population lives in rural areas and a large part of rural area in the country is remote and inaccessible in rainy seasons. Last but not least important are peoples’ ignorance, apathy, and various myths and beliefs related to health practices. All these together have made the provision for health care service a challenging task for the State.
In addition, there is another major problem. As happens generally, all advanced and efficient systems of health services develop and get concentrated in big cities and towns. This has been the case in India also. As a result, the flow of people from the villages to towns and cities has become inevitable. This places unbearable pressure on the health services in urban areas. To reverse the process requires development of appropriate health care services in rural areas. Such services have to be of the kind that include preventive measures of sizable proportion along with curative services for ailments that do not require any complex system of treatment and can be safely treated in their place of origin. Keeping these two vital factors in view the State in India had established a well-designed network of primary health care services in rural areas. The present health service delivery system is now nearly more than three decades old. However, the service has been constantly subjected to intense public scrutiny and review, and reform of the delivery system is often demanded. The State attempts to respond to such situations but often its response falls far short of public expectations. A major issue in the health service delivery system in India lies here.
HEALTH CARE SYSTEM IN INDIA
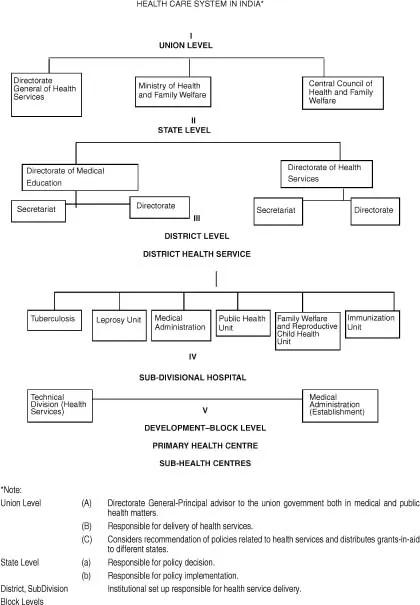
In order to understand the health care system in India, it is useful to know the general administrative set-up in the country. Indian union is a federation of states (provinces). Various sectors’ administration at the union and state level are regulated according to the jurisdiction laid down in the Indian Constitution. The sectors are grouped under three lists: (i) central list, which includes subjects exclusively administered by the union (central) government, e.g., defence, foreign policy, (ii) state list, which includes subjects that are exclusively under the domain of the states (provinces), e.g., law and order, (iii) concurrent list, which includes subjects which are within the purview of both union and state governments. Health is one such subject in the third list, so also education, social welfare, etc. In relation to the concurrent list, the union government provides the broad policy framework. It makes provision in the form of plan allocation, which is distributed among the states spread over the (five year) plan period. Each state, however, has the freedom to decide its own policy keeping in view its specific requirements within the national policy framework. Each state is also expected to mobilize its own resources to implement the programmes. Health being one of these, it may be helpful to know the health service set-up in India. For brevity and clarity, it is being presented in the form of a chart (see Chart I).
NATIONAL HEALTH POLICY
The National Health Policy (1983) evolved by the Ministry of Health and Family Welfare, Government of India, is being followed in designing health service development programmes at the state level.1 The policy lays emphasis on the following aspects: prevention of ill-health, promotion of public health, curative, and rehabilitation services and primary health care services in remote areas.
In pursuit of these goals some of the noteworthy features of health programmes are:
a. supply of safe drinking water and basic sanitation using techniques that people can afford;
b. reduction of existing imbalance in health services by concentrating on the rural health infra-structure;
c. concerted action to combat widespread malnutrition; and
d. greater coordination of different systems of medicines.
Considering the major focus of this particular discussion, these areas bear special significance for rural health services in the country. Item (d) here needs little elaboration. India has a number of indigenous systems of medicine. Important among these are Ayurveda and Unani.2 Ayurveda is called a science of life.3 It teaches not only the art of living but also how to cure diseases totally and maintains the power to fight diseases. Apart from these, many other systems developed by various indigenous groups in different parts of the country are there. While they do not have a nomenclature by which they can be known, their utility has become all the more relevant today in the background of scarce resources and inaccessibility of modern systems of medicine to the majority of the people, particularly in rural areas.
Homeopathy is a comparatively later development in the country but nonetheless one of the most sought after systems of medicine for three main reasons-very nominal cost of treatment, easy accessibility, and not much paraphernalia of investigations needed for treatment.
In the State of West Bengal, which is the focus of the article, efforts are on to bring particularly Ayurveda and Homeopathy within the purview of the formal health care system in rural areas provided through the Primary Health Centres (PHC).
Another aspect that has a significant bearing on health and the health service delivery system is environment. It has become a matter of increasing concern, particularly for the health care system. Environmental hazards of urban areas are usually talked about, but environmental hazards of rural areas are no less disturbing. Lack of proper sanitation facilities, along with increasing use of chemicals in modern agricultural practice leading to pollution of drinking water-the vital means of survival-as well as the receding forest coverage and greeneries have made living in rural areas as threatening as other pollutants in urban areas, the difference being only of degree. This, therefore, is an important health service concern in the State. With the financial assistance from the World Health Organization, it is striving to improve its health service development programmes. Besides this, in collaboration with the UNICEF, a rural sanitation programme has been initiated to devise low-cost sanitary facilities that are/or can be within the means of rural people. Particularly the poor under this programme are helped with the subsidy provided by the government, and some NGOs have also taken the lead in this matter. However, voluntary participation of people in the programme is emphasized, and this, therefore, is a slow process.
CHART 1
HEALTH SERVICE SET-UP IN THE STATE OF WEST BENGAL
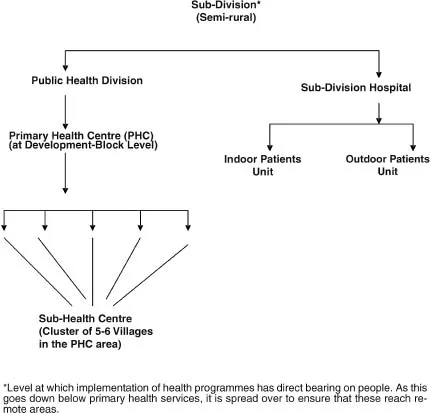
The health service set-up of the State of West Bengal is similar to the one described in the preceding chart. Promotion of health, prevention, and cure of disease form the three broad goals of health services in the State of West Bengal. Realization of the three goals becomes feasible when the service system is well managed. The state government lays special emphasis on the establishment of a dynamic health management system to make the health planning and health programme implementation meaningful. The approach adopted by the state is “bottom up,” laying special emphasis on how the health-related situations can be taken care of at their places of origin (see Chart II).4 The rationale behind this approach is to provide health facilities to treat common ailments at the village level itself. It also includes preventive measures such as mass immunization against childhood killer diseases and pre- and post-natal care of mothers. This is not only effective and meaningful but manageable, considering the limited resources (in material terms) available, while human and social support from families and communities are an added boon to this approach. Availability of such support is a remote possibility when treatment is carried out in a far-off health centre or hospital.
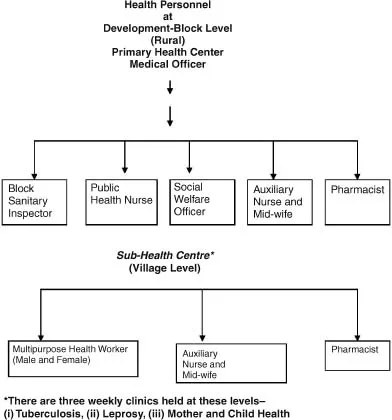
Administratively, there is a widespread network among health personnel at the grass roots level (see Chart III). This gets gradually consolidated and narrowed at the subsequent higher levels. Treatment of complex and complicated cases requiring specialized service then becomes the concern of the higher-level functional network.
CHART II
However, as is the case, gaps between policy and programme implementation are universal phenomena and the State is no exception in this respect.
The subject matter of discussion in this article paper has a background. The article therefore, deals with this in the beginning, followed by the changes affecting health care, more particularly in rural areas of the country, their implications for social work practice and the position of social work leadership in the health care system.
Background
Social work intervention in the health care services of the State in rural areas is an inevitable part of field work assignments of the students of social work of the University to which the author belongs. The field work programme is spread over 18-20 villages in the area and on an average, nearly 150 cases of health related difficulties are dealt with by the students in a year. While the programme’s major focus is student learning, it has created a very good network among services rendered by the Primary Health Centres (PHC), health personnel in the field, other health agencies (private) in local area as well as social service division of major hospitals and teaching hospitals in cities and towns of the State. It built such confidence among the people that people often approach the faculty and students for referral to the bigger hospitals in the cities and towns.
CHART III
At the village level, close collaboration with health staff facilitated effective teamwork in dissemination of health information, creation of awareness about health among the general public, and prevention and control of some prevalent common ailments and endemic diseases. This has been an important input in the service component at the village level, where social workers’ major contribution lies and could be seen.
Brief mention of the following few cases (of hundreds) in which social workers’ intervention helped mitigate the difficulties would explain the point.
A 35-year-old village priest suffering from congenital heart ailment was helped by the Social Worker to get the consultation of a leading cardiologist of a State Medical College and Hospital. He was advised to have surgery for replacement of a valve, to which the priest did not agree. He was apprehensive. He was counselled by the social worker all along this decision-making process. Ultimately, he was prescribed some medicines that he was required to take regularly. Being life saving drugs, these were available at a very nominal cost. His monthly expense in this regard was less than Rs.100.00 (a little more than U.S. $2.00). With this he carried on with his occupation quite normally.
The second case was of a child of 10 months suffering from a severe skin ailment. The family was extremely poor, and this was the first child of a young mother of 17 years. The social worker counselled her to hold patience and go for homeopathy treatment, which generally proved to be most effective as it killed the root cause of such diseases. Along with this she was advised to bathe the child with water in which margosa leaves, believed to contain antiseptic properties, were soaked well before bath. These had tremendous impact and the child was cured within a period of three months.
Third is the case of a village with a large number of tuberculosis patients. Social workers addressed the problem both at the individual level and at the community level. Most of the patients were drop-out cases. They were persuaded to resume treatment, while at the village level, a youth came forward to work in this area. He along with his peers took the initiative to uproot the disease from the village with the help of the social workers’ guidance, advice, and referral. Already affected patients are cured and there is no case of tuberculosis in the village today.
In a country like India, which is alw...