- 424 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Handbook of Neuro-Urology
About this book
Emphasizing the clinical problems surrounding urogenital tract dysfunction, this up-to-date reference details the basic science, differential diagnosis, and treatment of a wide range of neurourological conditions.
Covering recent advances in the neurobiology of the pelvic organs, the Handbook of Neuro-Urology
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Handbook of Neuro-Urology by David N. Rushton in PDF and/or ePUB format, as well as other popular books in Medicine & Neurology. We have over one million books available in our catalogue for you to explore.
Information
CLINICAL PROBLEMS AND THEIR MANAGEMENT
7
Urinary Incontinence
St. Helier Hospital, Carshalton, Surrey, England
King’s College Hospital, London, England
INTRODUCTION
Urinary incontinence is defined as the involuntary leakage of urine, which is a social or hygienic problem and is objectively demonstrable (1). It is a widespread problem, which seriously and adversely affects the quality of life of many women. In North America alone, 10 million adults are thought to be affected. This represents between 15 and 30% of older community-dwelling women and up to 50% of women in nursing homes (2).
In a recent Market and Opinion Research International (MORI) poll in the United Kingdom, 14% of women older than 30 years of age admitted to having suffered from urinary incontinence at some time. Half of these women had experienced problems within the last 2 months. Many women were embarrassed and worried by urinary symptoms, and 36% felt that their lifestyle had been adversely affected by their bladder problems (3).
Sommer et al. found the incidence of incontinence in 414 women who completed a symptom questionnaire to be 40% (4), but this was troublesome in only 6% of cases. Fifteen percent complained of stress incontinence, 13% of urge incontinence, and 12% had mixed symptoms.
The causes of female urinary incontinence are listed in Table 1. Of these, genuine stress incontinence (GSI) and detrusor instability (DI) comprise over 90% of cases. Overflow incontinence is relatively common, especially in the elderly, but the other causes are unusual. The etiology of the major causes of incontinence will be discussed in the following.
| Genuine stress incontinence |
| Detrusor instability |
| Overflow incontinence |
| Fistula |
| Congenital abnormality (e.g., ectopic ureter epispadias) |
| Temporary (e.g., immobility, fecal impaction, urinary tract infection) |
| Functional (lack of voluntary control) |
| Miscellaneous (e.g., urethral diverticulum) |
THE CAUSES OF INCONTINENCE
Incontinence will occur whenever the intravesical pressure exceeds the urethral closure pressure (5). Thus, uninhibited detrusor contractions, spontaneous relaxation of the urethral sphincter, or dysfunction of the urethral closure mechanisms may result in urinary leakage. Since most cases of female urinary incontinence fall into the first two categories, in the rest of this chapter the management of genuine stress incontinence and detrusor instability will be discussed in detail. Other causes of urinary incontinence will be addressed more briefly at the end of the chapter.
GENUINE STRESS INCONTINENCE
Genuine stress incontinence (GSI) remains the most common cause of urinary incontinence in women attending our urodynamic unit. Diagnosis is made during videocystourethrography, by observation of urinary leakage on raising intra-abdominal pressure, in the absence of a detrusor contraction. The bladder is normal; however, there is incompetence of the urethral sphincter mechanism.
In normal women, the bladder neck and proximal urethra are supported in an intra-abdominal position. Transmission of raised intra-abdominal pressure to the proximal urethra is important for the maintenance of continence. A healthy, intact urethra is also required.
With use of magnetic resonance imaging (MRI), Klutke et al. (6) highlighted the presence of direct musculofascial attachments from the levator muscle to the bladder neck and proximal urethra. The anatomy of these urethropelvic “ligaments” is different in women with GSI, compared with those with no incontinence. It is suggested that laxity of these ligaments following parturition and ageing, leads to posterior and downward rotation of the bladder neck, resulting in loss of effective intra-abdominal pressure transmission. Intrinsic defects of the urethra may also be detected with this technique. Magnetic resonance imaging provides clear anatomical information that may improve our understanding of the pathophysiology of genuine stress incontinence.
Cadaveric dissection also allows accurate study of pelvic floor anatomy. The vagina is densely adherent to the levator ani muscles, just caudal to the arcus tendineus fasciae pelvis. This attachment is 1 cm long and 0.5 cm wide, and lies in the region of the proximal urethra, extending up toward the bladder. Microscopically, connective tissue fibers from the vaginal wall, containing collagen, smooth-muscle fibers, and abundant elastin, interdigitate with the levator ani muscle. There is no direct connection between the urethra and the levator ani muscles, only indirectly by the pubovesical muscle. The urethra is closely attached to the vaginal wall and, therefore, its position and function may be influenced by levator ani contraction.
The connections of the vagina bilaterally to the arcus tendineus fasciae pelvis, have been viewed as the ropes supporting a “hammock” of supporting tissue beneath the urethra (7). The hammock itself consists of anterior vaginal wall and endopelvic fascia. Raised intra-abdominal pressure, acting on the urethra, forces it against the supporting layer, resulting in apposition of anterior and posterior urethral walls, increase in intraurethral pressure, and occlusion of the lumen. Damage to these supporting structures during parturition may lead to defective occlusion of the urethral lumen during stress episodes and, ultimately, to genuine stress incontinence.
With single-fiber electromyography of the pubococcygeus muscle, Smith et al. found that women with stress incontinence had a significant increase in denervation of the pelvic floor compared with asymptomatic women (8). This partial denervation and subsequent reinnervation was found to be a normal feature of aging and was increased by childbirth. No correlation was found between parity or the heaviest baby weight and the degree of pelvic floor denervation.
The confirmation and quantification of urinary leakage is sometimes difficult to achieve. A weighed pad test is often employed to assess both the presence and degree of incontinence. Lose et al. have compared the 1-hr ward test with the 24-hr home test, in the assessment of mild stress incontinence (9). Two 24-hr home tests were undertaken, and the results compared with a single 1-hr ward test. The 24-hr test is more sensitive in detecting incontinence, but is not reproducible.
Treatment of Genuine Stress Incontinence
The treatment of GSI is primarily surgical; however, this is not acceptable or suitable for all women. In cases of mild GSI, women who desire more children, and those who are unfit for anesthesia, conservative treatment is preferable.
Pelvic Floor Exercises
Since the advent of progressive resistant exercises, devised by Kegal (10), much attention has been drawn to their role in the treatment of GSI. Fergusson et al. treated 20 women with proved GSI for 6 weeks, using pelvic floor exercises (11). Ten women used an intravaginal perineometer and ten did not. Both groups showed significant reduction in leakage on both 30-min and 24-hr pad tests.
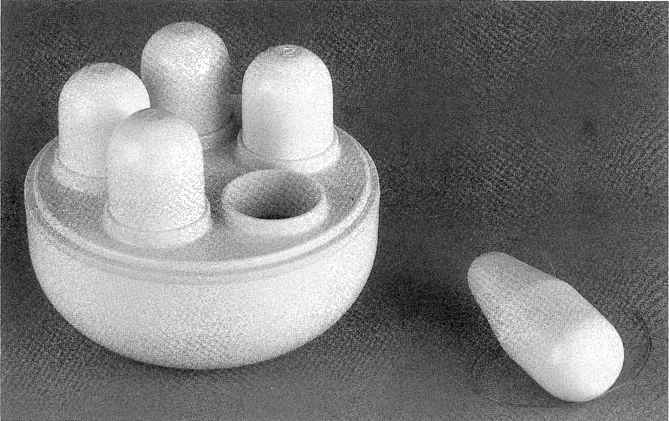
Vaginal Cones
Vaginal cones were devised by Plevnik (12) as a new method of strengthening pelvic floor muscles (Fig. 1). Cone therapy has reduced urinary loss due to GSI following 1 month of training (13). There was a significant correlation between decreased urine loss and increase in retained cone weight. Wilson and Borland have also shown subjective and objective improvement in women with proven GSI who used vaginal cones for 6 weeks (14). Olah et al. randomized 60 women with symptoms of stress incontinence, without urodynamic diagnosis, to receive either interferential therapy or training with vaginal cones for 1 month (15). No difference was observed between the two groups in terms of subjective or objective improvement. Cones provide a cheap, effective method of treatment for GSI that is not labor-intensive or time-consuming. The therapy is acceptable to most women and is without side effects.
Electrostimulation of the Pelvic Floor
Electrostimulation is widely used, by physiotherapists, in addition to pelvic floor exercises. Different techniques of administration are available, including faradism, interferential therapy, and maximal electrical stimulation. All three methods have been of benefit in the treatment of GSI (15,39).
Drug Therapy
The evidence that estrogens improve continence in women with GSI is conflicting. They may improve collagen fiber strength in the supporting structures of the bladder neck and enhance the urethral closure mechanism by improving mucosal integrity. Phenylpropanolamine has decreased episodes of leakage in women with GSI (16).
Ahlstrom et al. (17) treated 29 postmenopausal women with GSI, using estriokl (a weak estrogen), 4 mg once a day, in combination with eithephenylpropanolamine (an α-adrenoceptor agonist), 50 mg twice daily, or placebo. Combined treatment resulted in a 22% increase in maximum urethral closure pressure. Pressure transmission ratio, at the point of maximum urethral pressure, increased 15% with both treatments. The number of leakage episodes was reduced by 28%, and a significant reduction in leakage on pad testing was achieved in the combined treatment group. Estriol alone did not alter the number of leakage episodes or the amount of leakage on pad testing. Treatment using an a-adrenoceptor agonist in combination with estrogen is more effective than using estrogen alone.
Other Treatments
The use of a vaginal tampon or sponge has been advocated to reduce urinary leakage during stress episodes (e.g., exercise) (18). This acts partly by elevation of the bladder neck and partly by urethral compression.
Nielsen et al. have developed a urethral plug, consisting of a urethral plate, a soft stalk, and one or two spheres along the stalk (19). Twenty-two women were treated for 1 week with the one-sphere device, and 14 of these went on to be treated with the two-sphere device. Seventy-three percent of women were subjectively and objectively continent or improved using the one-sphere plug. For the two-sphere device the success rate was 79%. Difficulty in inserting the plug, and loss of the device during incontinent episodes was encountered in some patients.
A pilot study using a small triangular foam pad with a hydrophilic adhesive layer on one side, which acts to cover the urethral meatus, has been carried out in 20 patients with GSI...
Table of contents
- Cover
- Half Title
- Series Page
- Title Page
- Copyright Page
- Series Introduction
- Preface
- Table of Contents
- Contributors
- Basic Studies
- Investigation
- Clinical Problems and their Management
- Index
- About the Editor