
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Skin and Connective Tissue
About this book
Even a quick look at the surface of human skin reveals its many complexities. Much more than a simple shell for the human body, the skin helps protect internal organs and, working in conjunction with connective tissue, allows the human body to function as a unit. This comprehensive volume examines the components of the human integumentary system, as well as the various diseases and disorders to which it is vulnerable.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Skin and Connective Tissue by Britannica Educational Publishing, Kara Rogers in PDF and/or ePUB format, as well as other popular books in Biological Sciences & Physiology. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
ANATOMY OF THE HUMAN SKIN
The skin and connective tissue are vital components of the human body. Skin, which is the covering (or integument) of the body’s surface, is the largest organ of the human body. It provides protection and receives sensory stimuli from the external environment. Connective tissue, on the other hand, provides a framework that supports the body’s organs, including muscle and skin. By uniting muscles with tendons, ligaments, and bone, and by bringing elasticity to the skin, connective tissue enables the body to function as a cohesive unit, with the many parts moving together fluidly.
While connective tissue is made up of various combinations of cells, extracellular fibres, and a gel-like material known as ground substance, the skin consists of three well-defined layers of tissue: the epidermis, the dermis, and the subcutis. The epidermis is the outermost layer and contains the primary protective structure, the stratum corneum. The dermis is a fibrous layer lying beneath the epidermis that supports and strengthens the epidermis. The subcutis is a subcutaneous layer of fat that lies beneath the dermis, supplies nutrients to the other two layers, and cushions and insulates the body.
DISTINCTIVE FEATURES
The characteristic features of skin change from the time of birth to old age. In infants and children it is velvety, dry, soft, and largely free of wrinkles and blemishes. Children younger than two years sweat poorly and irregularly, presumably because their sebaceous glands function minimally. At adolescence hair becomes longer, thicker, and more pigmented, particularly in the scalp, axillae, and pubic eminence, and on the male face. General skin pigmentation increases, localized pigmented foci appear mysteriously, and acne lesions often develop. Hair growth, sweating, and sebaceous secretions begin to blossom. As a person ages, anatomical and physiological alterations, as well as exposure to sunlight and wind, leave skin, particularly that not protected by clothing, dry, wrinkled, and flaccid.
Human skin, more than that of any other mammal, exhibits striking topographic differences. An example is the dissimilarity between the palms and the backs of the hands and fingers. Likewise, whereas the skin of the eyebrows is thick, coarse, and hairy, that on the eyelids is thin, smooth, and covered with almost invisible hairs. The face is seldom visibly haired on the forehead and cheekbones. It is completely hairless in the vermilion border of the lips, yet coarsely hairy over the chin and jaws of males. The surfaces of the forehead, cheeks, and nose are normally oily, in contrast with the relatively greaseless lower surface of the chin and jaws. The skin of the chest, pubic region, scalp, axillae, abdomen, soles of the feet, and ends of the fingers varies as much structurally and functionally as it would if the skin in these different areas belonged to different animals.
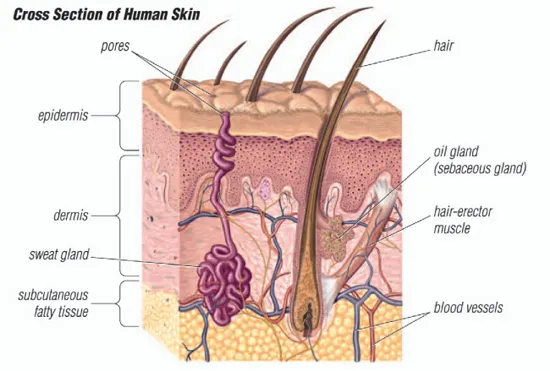
Section through human skin and underlying structures. Encyclopædia Britannica, Inc.
The skin achieves strength and pliability by being composed of numbers of layers oriented so that each complements the others structurally and functionally. To allow communication with the environment, countless nerves—some modified as specialized receptor end organs and others more or less structureless—come as close as possible to the surface layer, and nearly every skin organ is enwrapped by skeins of fine sensory nerves.
THE DERMIS
The dermis makes up the bulk of the skin and provides physical protection. It is composed of an association of fibres, mainly collagen, with materials known as glycosaminoglycans, which are capable of holding a large amount of water, thus maintaining the turgidity of the skin. A network of extendable elastic fibres keeps the skin taut and restores it after it has been stretched.
The hair follicles and skin glands are derived from the epidermis but are deeply embedded in the dermis. The dermis is richly supplied with blood vessels, although none penetrates the living epidermis. The epidermis receives materials only by diffusion from below. The dermis also contains nerves and sense organs at various levels.
BLOOD AND LYMPH VESSELS
Human skin is enormously well supplied with blood vessels. It is pervaded with a tangled, though apparently orderly, mass of arteries, veins, and capillaries. Such a supply of blood, far in excess of the maximum biologic needs of the skin itself, is evidence that the skin is at the service of the blood vascular system, functioning as a cooling device. To aid in this function, sweat glands pour water upon its surface, the evaporation of which absorbs heat from the skin. If the environment is cold and body heat must be conserved, cutaneous blood vessels contract in quick, successive rhythms, allowing only a small amount of blood to flow through them. When the environment is warm, they contract at long intervals, providing a free flow of blood. During muscular exertion, when great quantities of generated heat must be dissipated, blood flow through the skin is maximal.
In addition to its control of body temperature, skin also plays a role in the regulation of blood pressure. Much of the flow of blood can be controlled by the opening and closing of certain sphincterlike vessels in the skin. These vessels allow the blood to circulate through the peripheral capillary beds or to bypass them by being shunted directly from small arteries to veins.
Human skin is permeated with an intricate mesh of lymph vessels. In the more superficial parts of the dermis, minute lymph vessels that appear to terminate in blind sacs function as affluents of a superficial lymphatic net that in turn opens into vessels that become progressively larger in the deeper portions of the dermis. The deeper, larger vessels are embedded in the loose connective tissue that surrounds the veins. The walls of lymph vessels are so flabby and collapsed that they often escape notice in specimens prepared for microscopic studies. Their abundance, however, has been demonstrated by injecting vital dyes inside the dermis and observing the clearance of the dye.
Because lymph vessels have minimal or no musculature in their walls, the circulation of lymph is sluggish and largely controlled by such extrinsic forces as pressure, skeletal muscle action, massaging, and heat. Any external pressure exerted, even from a fixed dressing, for example, interferes with its flow. Since skin plays a major role in immunologic responses of the body, its lymphatic drainage is as significant as its blood vascular system.
THE SKIN SURFACE
The intact surface of the skin is pitted by the orifices of sweat glands and hair follicles—the so-called pores—and is furrowed by intersecting lines that delineate characteristic patterns. All individuals have roughly similar markings on any one part of the body, but the details are unique. The lines are oriented in the general direction of elastic tension. Countless numbers of them, deep and shallow, together with the pores, give every region of the body a characteristic topography. Like the deeper furrows and ridges on the palms and soles, the skin lines are mostly established before birth. The fine details of each area of body surface are peculiar to each individual. Fingerprints are used as a means of personal identification because they have a high relief, more evident patternings, and can be easily obtained.
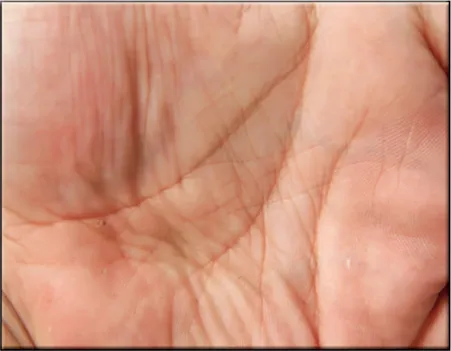
The lines on human palms start to form in utero, although they may be altered somewhat through use as a person ages. Shutterstock.com
Some of the lines on the surface of the skin are acquired after birth as a result of use or damage. For example, furrows on the forehead are an accentuation of preexisting congenital lines that become strongly emphasized in old age. As the skin becomes less firm with aging, it also forms wrinkles. Certain occupations leave skin marks that, depending upon duration and severity, may be transient or permanent.
The palms of the hands and the soles of the feet are etched by distinct alternating ridges and grooves that together constitute dermatoglyphics. The ridges follow variable courses, but their arrangement in specific areas has a consistent structural plan. Though apparently continuous, the ridges have many interruptions and irregularities, branching and varying in length. Every small area of surface has ridge details not matched anywhere in the same individual or in any other individual, even in an identical twin. This infallible signature makes dermatoglyphics the best-known physical characteristic for personal identification.
THE EPIDERMIS
The epidermis is thicker on the palms and soles than it is anywhere else and is usually thicker on dorsal than on ventral surfaces. Omitting the fine details, it is divisible everywhere into a lower layer of living cells and a superficial layer of compact dead cells.
GENERAL STRUCTURE
All the cells, living or dead, are attached to one another by a series of specialized surfaces called attachment plaques, or desmosomes. Thus, instead of being completely fused, the membranes of adjacent cells make a zipperlike contact, with fluid-filled spaces between the contact areas. This structural pattern ensures a concatenation of cells to one another so that they cannot be sloughed off easily. At the same time, this structure also allows nutrient fluids to seep in from the vessels in the dermis. Epidermal cells, which multiply chiefly at the base in contact with the dermis, gradually ascend to the surface, manufacturing keratin as they go. They finally die in the upper part, forming a horny layer.
The epidermis is thickest on friction surfaces and thinnest over the eyelids, on the lower parts of the abdomen, and around the external genitalia. Unlike that of most other mammals, it has an intricately sculptured underside and does not lie flat upon the dermis. Seen from beneath, there are straight and branching ridges and valleys, columns and pits, all finely punctuated.
Because of this unevenness, it is almost impossible to state the exact thickness of epidermal tissue. Furthermore, individual differences, sex, and age have an enormous influence on the structure of the underside. Such labyrinthine patterns give human epidermis two unique advantages: it attains a more intimate connection with the subjacent dermis than if the surface were flat, and its source of dividing cells, the building blocks of the horny layer, is greatly increased.
MAJOR LAYERS
The clear stratification of the epidermis is the result of well-defined changes in its major constituent cells—the keratinocytes, or corneocytes—as they move peripherally from the basal layer, where they are continuously formed by mitosis, to the skin surface, where they are lost. In essence, the epidermis consists of a living malpighian layer (consisting of cells whose protoplasm has not yet changed into horny material), in contact with the basement membrane (which is attached to the dermis), and a superficial cornified (horny) layer of dead cells.
The innermost cells of the malpighian layer, next to the basement membrane, make up the basal layer, or stratum basale. Immediately peripheral to the basal layer is the spinous, or prickle-cell, layer—the stratum spinosum. Its cells have a spiny appearance due to the numerous desmosomes on their surface. Studies with the electron microscope have revealed that desmosomes are symmetrical, laminated structures in which some layers are contributed by the plasma membranes of adjoining cells and some form an intercellular component.
The spinous layer is succeeded by the granular layer, or stratum granulosum, with granules of keratohyalin contained in the cells. These small particles are of irregular shape and occur in random rows or lattices. The cells of the outer spinous and granular layers also contain much larger, lamellated bodies—the membrane-coating granules. They are most numerous within the cells of the spinous layer. In the granular layer they appear to migrate toward the periphery of each cell and to pass into the intercellular spaces, where they discharge their waxy lipid components.
Peripheral to the granular layer is the stratum corneum, or horny layer, in which the keratinocytes have lost their nuclei and most of their organelles and contents, including the keratohyalin granules. They become progressively flattened and filled with keratin and are ultimately desquamated. Between the granular layer and stratum corneum, an unstainable stratum lucidum, or hyaline layer, can be recognized in palmar and plantar epidermis and some other regions (palmar and plantar refer to the palm surface of the hand and the bottom surface of the foot, respectively).
DYNAMICS AND ORGANIZATION
Horizontal stratification is the most obvious histological feature of the epidermis. There is also, however, distinct evidence of vertical organization. In thin epidermis, though not in thick plantar skin, the cornified cells can be shown to be arranged in regular stacks, which must reflect the underlying dynamic mechanisms. It appears that several living spinous cells are precisely and symmetrically stacked beneath each cornified column and that these are related to their own basal cells. The cells do not pass from one stock to another.
All keratinocytes are formed by mitosis (cell division) in the lower region of the malpighian layer (the malpighian layer consists of both the stratum basale and the stratum spinosum of the epidermis). Most of the dividing cells are found in the basal layer, although it is likely that about one-third of the divisions occur above this level. Proliferating cells undergo a cycle: mitosis is followed by an interphase, this in turn is followed by a phase of DNA synthesis, and then another short resting phase occurs before mitosis begins again. The complete mitotic cycle takes about 12 to 19 days. The time for the passage of cells through the epidermis, from formation to desquamation, has been variously estimated at one to three months.
In normal skin the production and loss of cells must be finely balanced, otherwise the thickness of the epidermis would fluctuate. When the epidermis becomes abnormally thick, as in the plaques of psoriasis, this balance is altered. Either the production of cells in the malpighian layer must be abnormally high or their time of passage must be decreased. It is now generally agreed that such conditions result from a greatly increased production of cells, and the cells move more, not less, rapidly through the epidermis.
There is, however, a further controversial problem. If all the basal cells were continuously cycling, greater production could be achieved only by a substantial reduction in the duration of the cell cycle. An alternative hypothesis is that not all the cells are undergoing cycles at any one time, so that greater cell production can be achieved by recruiting resting cells into activity. It seems likely that the epidermis does indeed contain noncycling cells, which can become activated, and that the cell cycle in psoriatic epidermis is accelerated only about twofold, not twelvefold, as once proposed.
When skin is wounded, there is a burst of epidermal mitotic activity about 40 hours later. It is evident, therefore, that local mechanisms of control must come into play, with either inhibitors being dispersed by wounding, or stimulating hormones being released, or both. There is, on the one hand, some evidence of the existence of inhibitors, or chalones. On the other hand, an epidermal growth factor (EGF) has been isolated from the salivary glands of mice and its chemical structure determined (a single-chain, folded polypeptide with 53 amino acid residues and three intramolecular disulfide bonds). It is not, however, extractable from skin, though the receptor protein to which it attaches in order to perform its action is present in many skin cells, and a closely similar molecule has been isolated from human urine.
THE KERATIN LAYER
The final product of the epidermis is the keratin that packs the cornified cells. The term keratin is applied generally to the hard keratins of hair, horn, and nails, and to the soft keratin of the epidermis. They are all insoluble filamentous proteins, composed of polypeptide chains that are stabilized by links using two atoms of sulfur. The source of the keratin of the stratum corneum has been a subject of controversy. However, it is now generally accepted that about a third of its total mass is made up of proteins synthesized in the granular layer and the remainder from so-called intermediate filaments, which are present in keratinocytes from the basal layer outward.
The barrier that prevents water loss from the body is situated in the lower part of the horny layer. In this region the spaces between the compacted layers of keratin-filled cells contain lamellae of lipid (wax) that has been formed within the membrane-coating granules of the live epidermal cells below.
HAIR
The apparent lack of body hair immediately distinguishes humans from all other large land mammals. Regardless of individual or racial differences, the human body seems to be more or less hairless, in the sense that the hair is so vestigial as to seem absent. Yet, in certain areas hair grows profusely. These relatively hairy places may be referred to as epigamic areas, and they are concerned with social and sexual communication, either visually or by scent from glands associated with the hair follicles.
Human hair has little protective value, even in hirsute (excessively hairy) people. Eyelashes, eyebrows, and the hairs inside the external ears and nostrils have obviously useful funct...
Table of contents
- Cover Page
- Title Page
- Copyright Page
- Contents
- Introduction
- Chapter 1: Anatomy of the Human Skin
- Chapter 2: Characteristics of Connective Tissue
- Chapter 3: Embryology and Biodynamics of Skin and Connective Tissue
- Chapter 4: Skin Diseases and Injuries
- Chapter 5: Skin Infections and Infestations
- Chapter 6: Diseases and Disorders of Skin Tissues
- Chapter 7: Diseases and Disorders of Connective Tissue
- Chapter 8: Cancers and Hereditary Disorders of the Skin and Connective Tissue
- Conclusion
- Glossary
- Bibliography
- Index