- English
- ePUB (mobile friendly)
- Available on iOS & Android
Synopsis of General Pediatric Practice
About this book
This textbook provides a brief review of pediatric medicine practice. This book covers the diseases and disorders commonly seen in routine practice. The chapters cover pediatric disorders such as obesity, gastroesophageal reflux, asthma, bronchiolitis, pneumonia, allergy, sinusitis, diabetes, thyroid disorder, epistaxis, otitis media, hearing loss, laryngomalacia, obstructive sleep apnea, central sleep apnea, laryngomalacia, stridor, tonsillitis, haemophilia, autism, and anxiety.
Key features of this textbook include:
- Reader friendly format which explains etiology, pathophysiology, and disease management
- 21 chapters covering common pediatric disorders encountered by medical professionals
- Contributions by several experts in pediatric subspecialties
This textbook is a suitable reference for medical students, interns, residents, and specialists including pediatricians, family medicine practitioners, otolaryngologists as well as subspecialists such as pediatric cardiologists, pulmonologists, endocrinologists, otolaryngologists and allergists.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
Synopsis of Management of Diabetes Mellitus Types 1 and 2
Eric Velazquez, Bethany A. Auble*
Abstract
* Corresponding author Bethany A. Auble: Medical College of Wisconsin, Children’s Hospital of Wisconsin, Milwaukee, Wisconsin, USA; Tel: 414-337-8717; Fax: 414-266-6749; Email: [email protected]
INTRODUCTION
Epidemiology
Physiology
TYPE 1 DIABETES MELLITUS
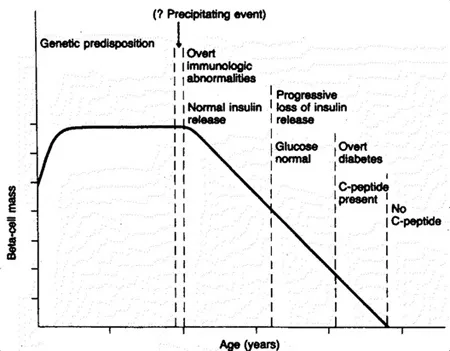
The Eisenbarth model for the development of Type 1 Diabetes is divided into six stages: 1. Genetic Predisposition, 2. Triggering “Event,” 3. Activation of Autoimmune Response, 4. Immunologic Response with progressive loss of insulin secretion with maintenance of normal blood sugar level, 5. Symptoms develop, but residual insulin secretion is maintained, 6. Loss of residual insulin secretion to a point of glucose dysregulation [4].
Multiple Daily Injection Insulin Regimens
| Insulin Type | Examples | Onset of Action | Peak Effect | Duration of Action |
|---|---|---|---|---|
| Rapid-Acting | Insulin Lispro (Humalog), Insulin Aspart (NovoLog) Insulin Glulisine (Apidra) | 15-20 minutes | 30-90 minutes | 1-4 hours |
| Regular-Acting | Novolin R and Humulin R | 30-45 minutes | 2-3 hours | 5-8 hours |
| Intermediate-Acting | NPH (Humulin N, Novolin N) | 2-4 hours | 4-10 hours | 4-12 hours |
| Long-Acting | Insulin glargine (Lantus) Insulin detemir (Levemir) | 2-4 hours | No peak 8-10 hours | 20-24 hours Dose-related |
| Insulin | Dose Calculation | Calculation for 20 kg Child | Dose | |
|---|---|---|---|---|
| Total Daily Insulin Dose | 0.5 – 1.0 units/kg/day | 0.5 x 20 = 10 units/day | 10 Units | |
| Basal Dose | Glargine Detemir | 50% of total 50% of total divided into twice a day dosing | 50% x 10 = 5 units | 5 Units |
| Meal-time Glucose Correction | Lispro, Aspart Regular | 1800 / Daily Dose 1500/ Daily Dose | 1800 / 10 = 180 1500 / 10 = 150 | 1 unit for every 180 mg/dL > ideal glucose 1 U for every 150 mg/dL > ideal gluc... |
Table of contents
- Welcome
- Table of Contents
- Title Page
- BENTHAM SCIENCE PUBLISHERS LTD.
- PREFACE
- List of Contributors
- Update on the Management of Otitis Media
- Contemporary Management of Children with Hearing Loss
- Overview of Management of Recurrent Tonsillitis
- Therapies for Pediatric Chronic Rhinosinusitis
- Practical Management of Children with Stridor
- Update on the Management of Laryngomalacia
- Synopsis of Management of Diabetes Mellitus Types 1 and 2
- Pediatric Type 2 Diabetes Mellitus
- Practical Guide for Management of Children with Obesity
- Current Concepts in the Management of Hyperthyroidism
- Recent Advances in Pediatric Asthma
- Evaluation and Treatment of Bronchiolitis
- What is New with Management of Pediatric Central Sleep Apnea?
- Practical Considerations in the Treatment of Pediatric Obstructive Sleep Apnea
- State of the Art of the Diagnosis and Management of Gastroesophageal Reflux Disease
- Essentials of Sickle Cell Disease Management
- Management of Recurrent Epistaxis
- Update on Management of Allergic Rhinitis
- The Management of Pediatric Allergic Emergencies
- Autism Spectrum Disorder: What a Pediatrician Should Know
- Treating Anxiety in Children