eBook - ePub
mHealth
From Smartphones to Smart Systems
- 152 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
mHealth: From Smartphone to Smart Systems provides a high level and comprehensive survey of the emergence of mobile technology healthcare. This book looks beyond the already-popular devices and apps associated with mHealth, exploring the major role this technology could play as healthcare steers inexorably toward an architecture
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access mHealth by Rick Krohn,David Metcalf, Rick Krohn, David Metcalf in PDF and/or ePUB format, as well as other popular books in Business & Business General. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
The Case for an mHealth Ecosystem
By Rick Krohn, MA, MAS
In the ongoing debate about its future, much is made of the fragmentation and inefficiencies that characterize our healthcare system. This argument suggests that to “fix” healthcare, we must repair the broken parts of existing processes and venues of care delivery. That’s a serious misreading of the problem—like changing a tire when the car has run out of gas.
According to the Centers for Disease Control and Prevention and the National Institutes of Health, more than 50 percent of the factors related to personal health can be traced to lifestyle choices, while only 10 percent is related to the medical care system. This finding illustrates a stark truth: the US healthcare system in its current incarnation—facility based, episodic care—is insufficient to the task of improving population health (see Figure 1-1). An aging population, clinical staff shortages, cost inflation and uneven quality are contributing to an increasingly severe crisis.
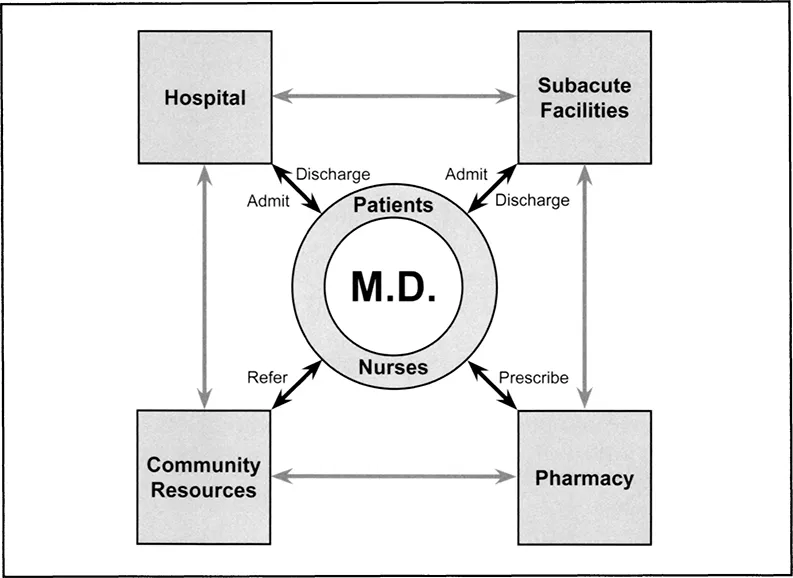
Figure 1-1 The Old Episodic Model of Healthcare Delivery.
What is needed to reverse this trend is a delivery system with a greater array of provider-patient touch points, with better care coordination and clinical collaboration, with diagnostic tools for self-care, with aligned incentives and with the capability of achieving behavioral change across the spectrum of healthcare stakeholders. What is needed is a patient-centric healthcare ecosystem. As Figure 1-2 illustrates, this ecosystem features a wholesale shift from physician-focused, episodic care to consumer-focused, persistent engagement.
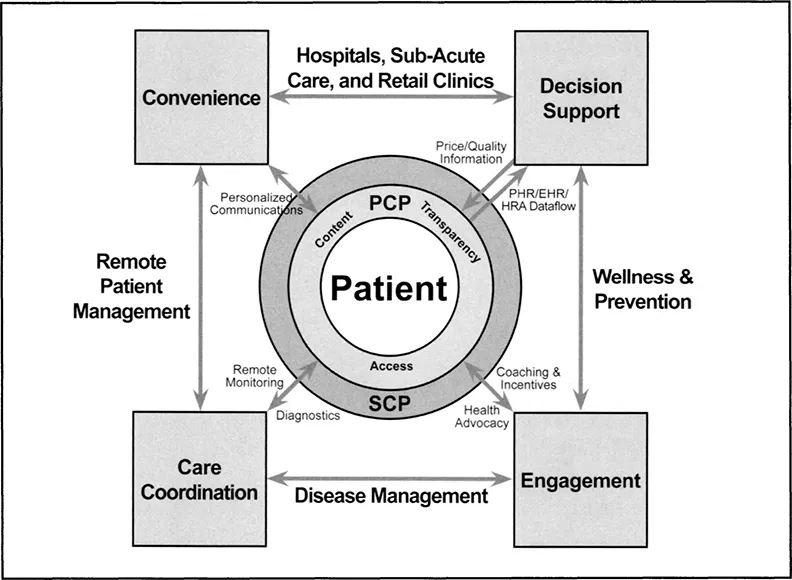
Figure 1-2 The Engaged Ecosystem of Healthcare Delivery.
In a general context, a healthcare ecosystem describes the interplay of many factors, including the environment, personal attributes and relationships, cultural influences, technology and health resources that affect an individuals health status. The idea of a healthcare ecosystem envisions an environment of comprehensive, high quality, convenient, affordable, personalized and accessible care. In this ecosystem, patients and consumers are empowered through education, knowledge and tools to be their own health managers. The healthcare ecosystem places a strong emphasis on health promotion, wellness and prevention, as well as self management.
From Health Ecosystem to mHealth Ecosystem
Mobile plays well in this new healthcare landscape. mHealth integrates “smart systems” mobile technologies and solutions with enterprise and legacy systems, with mobile environments and with new care modalities. The mHealth smart system is about extending access and remote connectivity within the industry and with every stakeholder—its about engagement among providers, with patients and consumers, with payers and employers, public health and social services. In both clinical and business applications, mHealth smart systems are aimed at the creation of connected communities through the integration of mobile communication, transactions and knowledge. This community, or ecosystem, includes payers, providers, consumers, vendors and telecommunications. It harnesses the collective power of enabling technology, efficient resource allocation, clinical decision support and persistent patient care. The mHealth ecosystem supports emerging industry payment and delivery models, like performance-based reimbursement, accountable care organizations, the patient-centered medical home, meaningful use, aging-in-place and early intervention. And at its heart, the mHealth ecosystem addresses healthcare’s most intractable problems—unsustainable cost inflation, access to care and uneven clinical quality.
The mHealth ecosystem is characterized by innovation in care delivery, robust care teams and heightened clinical collaboration, an epidemiological health perspective (including population health, prevention and wellness), utilitarian technology solutions and consumerism. Most importantly, it is about recasting the terms of healthcare delivery by placing the patient in the solid center. “Nothing about me, without me” captures the conceptual framework of a healthcare ecosystem in which the patient is the central figure. Information is now portable, personalized and participatory, making a patient-centric mHealth ecosystem unbound by age, location or economic strata. This is a watershed moment in the state of US healthcare—the mHealth ecosystem is a catalyst that can fundamentally reshape healthcare delivery as it is now practiced.
To perform efficiently, the mHealth ecosystem must be convenient, connected, coherent and cost-effective. Its organizing principle is alignment—alignment of the inputs to healthcare (the verticals, the venues, the spectrum of caregivers, the technologies, the workflows) within an integrated, interoperable system architecture that is efficient and accessible. Figure 1-3 describes the higher order of clinical quality and operating efficiency that can be delivered within the mHealth ecosystem.
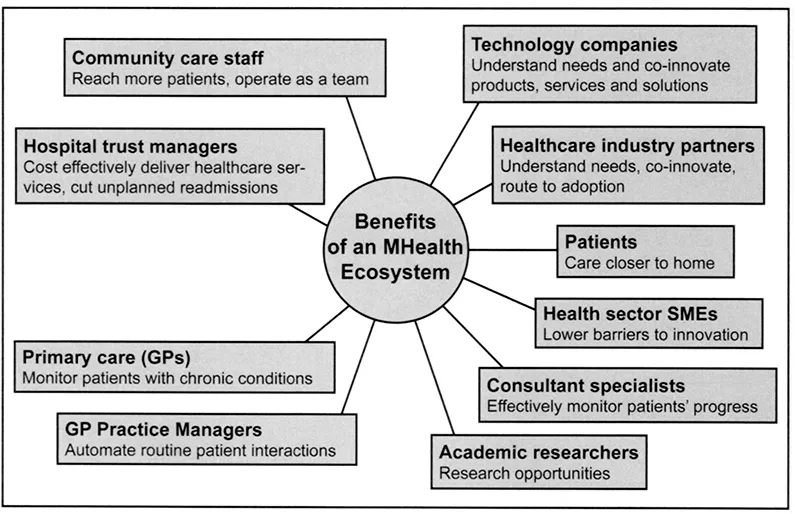
Figure 1-3 The Benefits of an mHealth Ecosystem.
In the mHealth ecosystem, information isn’t pushed or pulled—it’s shared persistently and pervasively. Healthcare information is shared in real-time among providers, patients and consumers in bilateral flows, but can include a larger universe of stakeholders, including payers, employers, public health, social services, researchers, solutions providers, partners, supply chain and more. Figure 1-4 describes at a baseline the on-demand, bilateral information flows within the mHealth ecosystem.
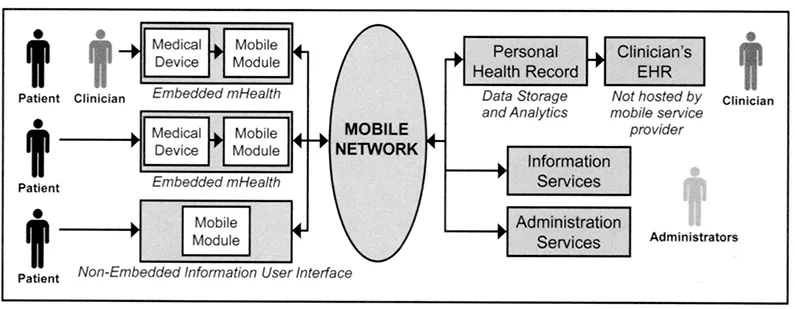
Figure 1-4 The Bidirectional Information Flows in the mHealth Ecosystem.
But in the euphoria surrounding the mHealth ecosystem what often gets understated are sizeable hurdles to the mass adoption of mHealth tools and solutions. From a product perspective, mHealth has yet to achieve a state of maturity that uniformly addresses reliability and product support; liability and regulatory concerns; data standards, interoperability and integration; privacy and security; and workflow integration. From a business perspective, mHealth has yet to land on a proven business model or an established reimbursement methodology. At the end of the day, the mHealth ecosystem must rest on a solid business foundation.
How can mHealth companies address these business hurdles? Certainly by architecting solutions that solve a problem or generate revenue, but also by branding themselves as solution providers with a keen understanding of customers business issues, their workflow bottlenecks, their cost/benefit calculus, their overarching business strategy and their C-level expectations. As discussed in greater detail in Chapter 7, this can only be accomplished through the effective intertwining of corporate development, marketing and sales.
If I Build it, Will They Come?
For the mHealth ecosystem to reach its fullest expression, the number one issue that must be addressed is defining, attracting and retaining the customer. The mHealth customer is unlike the traditional buyer of healthcare services, because where traditional healthcare is sold on a business-to-business or business-to-consumer basis, mHealth is largely a retail market. Although clinicians—mainly doctors and nurses—account for a proportion of mHealth market growth, the primary driver to date has been the consumer. They’re not just buying smartphones and tablets in stores and online, they’re buying apps, medical devices and services. But in healthcare, direct-to-consumer has a mixed record of success. For several years an ongoing problem obstructing the patient-centric model of healthcare has been getting the healthcare consumer—not just the patient with issues, but the enlightened public as well—actively engaged in digital health.
After all, patient-centric healthcare without patient involvement is just an illusion. To date, the patient portal hasn’t proved to be the form horse of consumer engagement, and neither has the personal health record. Why? Because in the main, consumers choose to avoid the tedium of entering and maintaining their own health data. But that pattern of behavior is not repeating itself in the mobile world. Consumers are mimicking the kind of digital convergence—the intersection of personal and professional applications via mobile—that is a growing feature of clinical workflow. Once someone has a wireless device, that person is more likely to use the Internet to gather information, share information and create new content. These patterns are beginning to emerge in Americans pursuit of health information on mobile devices.
Fact: wireless connections and devices are associated with deeper engagement in health-related social media. Its not just young adults driving the consumer movement toward mobile health. The “wireless pack” of healthcare consumers extends from 19-to 50-year-olds. These consumers are using their smartphones to manage weight, stop smoking, check vitals, get health tips—in sum, to keep personal health records.
Making the Leap to the mHealth Ecosystem
It has been widely reported that mobile health is a leapfrog technology, providing a platform for the care of populations and which possesses established mobile networks, but a weak healthcare infrastructure. Conceptually, a simple cell phone removes access and distance as barriers to both routine and chronic care. That opportunity to improve outcomes for the underserved—poor, rural and minority populations—is staring at us right here at home.
In a set of studies published by the American Health Information Management Association, it was determined that 87 percent of African-Americans and Latinos own cell phones and tend to access data apps. A mobile healthcare strategy would prove particularly effective in addressing the unmet needs among these minority populations—and that premise also holds true for Native Americans and other rural populations.
At a baseline level, mHealth will become both an adjunct for and a substitute to the office visit by providing culturally appropriate health information, medication reminders, lifestyle advice and bidirectional doctor-patient communication. In more advanced applications, mHealth solutions will serve as the conduit for patient treatments via remote patient management tools, self-care and telemedicine.
One of the most intriguing opportunities to fast-track an mHealth ecosystem exists in developing countries, where the infrastructure to support a fixed wired healthcare industry simply doesn’t exist. Of the estimated 5 billion mobile devices in use around the world, 64 percent are in the hands of people living in emerging market economies.
Although the depth of mobile technologies has not yet reached the sophistication of advanced nations, in developing countries mHealth offers a far more cost-effective and achievable alternative to establish an integrated, collaborative healthcare finance and delivery ecosystem. Though the analogy of mHealth’s impact in the developed world doesn’t directly translate to the domestic healthcare landscape, we can reverse engineer mobile healthcare successes elsewhere in the world to boost outcomes for our most vulnerable populations, and weave these proven technology solutions into our domestic mHealth ecosystem.
What Will it Take?
It’s going to take a wholesale restructuring of healthcare delivery to achieve an mHealth ecosystem. That includes cultural changes on the part of payers, providers and patients; a new definition of clinical “value” based on mass personalization of the care experience; partnerships that deliver collaborative, coordinated care; and team-based care delivered through new care systems, including the patient-centered medical home, the accountable care organization and health information exchanges. It’s going to take a realignment of payment incentives tied to the shift from volume to value as the primary metric of reimbursement, with attendant tools to measure and manage. It’s going to take interoperability and connectivity of information systems and information channels. And finally, it all must translate into improved operating efficiencies and bottom-line revenue.
CHAPTER 2
Opportunities and Obstacles in the Adoption of mHealth
By Mehran Mehregany; MS, PhD, and Enrique Saldivar, MD, MS, PhD
Technological advances have catalyzed tremendous ...
Table of contents
- Cover
- Title Page
- Copyright Page
- About the Editors
- About the Contributors
- Table of Contents
- Acknowledgments
- Foreword
- Introduction
- Chapter 1: The Case for an mHealth Ecosystem
- Chapter 2: Opportunities and Obstacles in the Adoption of mHealth
- Chapter 3: The mHealth Stakeholder
- Chapter 4: Mobile Building Blocks of the mHealth Ecosystem
- Chapter 5: The Integrated mHealth Ecosystem
- Chapter 6: Devising an mHealth Strategy
- Chapter 7: Business Modeling for the mHealth Ecosystem
- Chapter 8: Security & Compliance
- Chapter 9: Practical Applications and Complementary mHealth Technologies
- Chapter 10: The Future of mHealth
- Epilogue
- Index