1.1 Clinical Risk Factors and Course of Aspirin-Induced Asthma
Our findings have demonstrated that aspirin-induced asthma (AIA) is a disease with a clear and definite symptomatology, which differentiates it from aspirin-tolerant asthma (ATA). A particular feature of AIA is that it occurs in age periods when the human organism undergoes a hormonal alteration—in prepubertal children, women in their thirties, and men in their fifties or sixties. Women amount to 75% of cases.
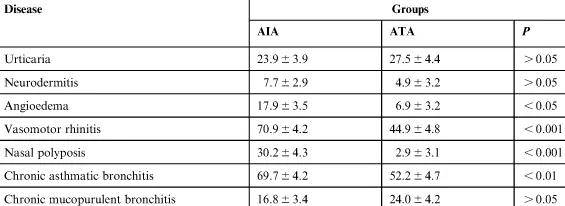
Prior to the first shortness of breath, most patients suffer pathology of the upper respiratory tract (see Table 1.1).
Table 1.1
Prevalence (%) of Different Diseases Prior to the Appearance of the First Attack of Breathlessness in Patients with AIA
The same peculiarities have been noted by other researchers as well [434,567,572,595]. We have also demonstrated that along with the occurrence of upper airway pathology, the initial symptoms of lung disease are observed that may point to changes in the reactivity of the bronchial tree: appearance of dry paroxysmal cough with blennoptysis and expiratory dyspnea in response to irritant inhalation, cold air, as well as in case of changing weather conditions, or exercise. Patients are often diagnosed with chronic asthmatic bronchitis. At the same time, some of them have noted the occurrence of angioedema in response to unknown exogenic factors. It is often a case that shortly before the illness, the patients may have suffered concussion of the brain, had a vaccination, or been under a significant amount of stress.
The first asthma attack may be provoked by contact with infectious or noninfectious allergens, operative intervention in accessory sinuses of the nose, inhalation of cold air or irritant odors, or exercise. The illness in women often starts to develop in the climacteric period.
As a rule, asthma attacks in response to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) occur in a patient who already has asthma and/or nasal polyps with chronic rhinosinusitis. The intake of these medications, however, initiates the asthmatic syndrome development in every one of three patients. Within an hour of aspirin ingestion, the patient may suffer an asthma attack, followed by rhinorrhea, conjunctival injection, and flushing of the upper body, mostly the head and neck. In some patients, the asthma attack is followed by hypotonia, hypersalivation, nausea, and vomiting, as well as pains in the upper abdomen. All these reactions are extremely dangerous for the patient’s life, as they may rapidly lead to shock, loss of consciousness, or even death.
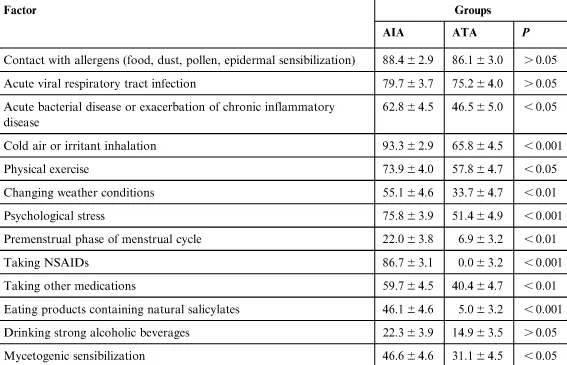
After the occurrence of NSAIDs intolerance, the course of asthma changes: the seasonality and acuity of asthma attacks disappears, there is a sense of permanent congestion in the chest, and the efficiency of ordinary bronchodilators decreases. Severe exacerbations of the disease are observed more than four times a year, irrespective of a season, and most patients with AIA (unlike aspirin-tolerant patients) react to a wider range of external factors (Table 1.2).
Table 1.2
Prevalence (%) of Factors Provoking Recurrent Asthma Attacks in Patients with AIA
It should be noted that the asthmatic syndrome in AIA patients develops against the background of the already-existing imbalance of the organism’s functional systems. Thus, in most patients, along with the signs of typical atopy, there can be observed a link between the asthma attacks and acute viral respiratory tract infection (AVRI), pneumonia, or chronic infection activation (sinusitis, cholecystitis, pancreatitis, etc.), which may indicate a disorder of the immune system of such patients. The latter by anamnesis may also show various benign tumors. Thus, 71% of AIA patients have nasal polyps, 18.8% of women have hysteromyoma, and 36% of women have indications for myomectomy or hysterectomy. The predisposition of patients with AIA to multiple polyposes (in the urogenital and gastrointestinal systems) has been noted by other authors [448]. The disorder of immune system functions in AIA has been also evidenced by our data on reduced resistance to AVRIs, existence of chronic infectious inflammatory processes, mycetogenic sensibilization, as well as the onset of asthmatic syndromes after immunization. Furthermore, we have found out that every second patient with AIA has a chronic persistent chlamydial infection caused by Chlamydia pneumoniae. This is confirmed by the fact that 38% of patients with AIA have IgG titers ≥1:32 to C. pneumoniae along with an increase of circulating immune complexes (CIC) in blood (>0.1 units) and a decrease of the monocytes migration index (<30%).
It is known that the development of viruses and intracellular microorganisms’ persistence, as well as the disorder of the organism’s antitumor defense, is based on the immune system deficiency, including the functional deficiency of T cells and natural killer (NK) cells [430,634]. Some authors point to a decrease of absolute and relative number of T lymphocytes and especially T helpers in patients with AIA and a change of their functional state, manifested in the distortion of T-lymphocytes response to serotonin and normal reaction to histamine, adrenalin, and theophylline [552]. It is believed that subjects with AIA have a deficit of NK cells as well as an imbalance of cellular subpopulations sensitive to monoamines [551]. Thus, the existence of immune system deficiency in AIA has been confirmed by other researchers.
Most patients with AIA at the beginning of the disease demonstrate symptoms which indicate to dysfunctions of central nervous system (CNS) early. Most patients with AIA, much more frequently than those with ATA, note the connection of asthma attacks with emotional suffering or psychological stress (Table 1.2). A dependency of the asthma attacks from psychoemotional suffering is diagnosed in 78.6% of young patients, and its frequency remains high in all ages. Anxiodepressive and asthenoneurotic syndromes are more frequently observed in patients with AIA, which is an evidence of increased anxiety, immature value system, and a low capability of independent decision making. In view of the evolutionary theory, such an organism possesses the least perfect mechanisms of environment adaptation [280]. Indeed, according to our data, in 18.3% of patients with AIA, the onset of the disease is linked with a psychoemotional trauma. This data which correlates with recently published materials of the European Network on Aspirin-Induced Asthma (AIANE), that demonstrate that psychological stress has been a triggering factor of the onset and exacerbations of the disease in 240 of 365 AIA patients [386]. Furthermore, the occurrence of nonallergic rhinitis with eosinophilia syndrome (NARES), which is viewed by Moneret-Vautrin et al. [366] as a preexisting disease of aspirin triad, is also linked to the existence of stress situations in the anamnesis (mourning, labor conflicts, divorce, unemployment, etc.) in half of the patients with AIA.
Among the factors that provoke recurrent asthma attacks, most patients with AIA point to cold air, irritant inhalation, physical exercise, and change of weather conditions (Table 1.2). It all of which are evidence of an airway hyperresponsiveness. It is known that in the genesis of airway hypersensitivity and hyperresponsiveness, which are the characteristic functional abnormality of bronchial asthma, a significant role belongs to the imbalance of exciting and inhibitory impacts of different elements of the vegetal nervous system. It is a common view that in patients with bronchial asthma there is an increased effect of acetylcholine parasympathetic neurotransmitter and dysfunction of adrenergic system—that is, an increase of α-receptors sensitivity and a decrease of β-receptor sensitivity [376,490,652]. As noted earlier, a change in the reactivity of airways is observed in patients prior to the appearance of typical asthma attacks, which is an evidence of early dysfunctions of vegetal regulation in AIA. This is also confirmed by the data of Moneret-Vautrin et al. [366] who have found a dysfunction of the autonomic nervous system in patients with NARES syndrome. The authors have revealed an increased sensitivity to adrenergic agents at the level of β2-receptors of large vessels and α1-receptors of small skin vessels in case of intradermal injection of papaverine hydrochloride causing edema and vasodilatation in healthy persons. At the same time, the activity of lymphocyte β-adrenoreceptors was not significantly different from those in healthy subjects [630]. This fact confirms that the dysfunction of central regulatory mechanisms in such patients play a certain role in the formation of an initial dysfunction of the autonomic nervous system. Thus, in patients with the asthmatic triad there were some changes recorded by electroencephalography (EEG) that pointed to a dysfunction of intracentral connections according to “diencephalic variant” and their relation to a change in the airway sensitivity threshold and responsiveness [316].
Along with dysfunctions in the nervous and immune systems of AIA, we have revealed early occurrences of functional disorders in the endocrine system. Thus, in 50% of female patients of young age, the exacerbation of asthma occurs in the premenstrual period. The studies by Markov [336], Kagarlitskaya [250], and Sabry [491] have also demonstrated a high percentage of patients with AIA among women suffering from premenstrual asthma attacks. Our analysis of the frequency of different past diseases has shown that 26% of female patients with AIA had menstrual disorders, miscarriages, and habitual noncarrying of pregnancy. Moreover, we have noted an early onset of menopause in these patients, at 46 years on average, as compared to 50 years in patients with ATA. Additionally, 36% of women with AIA had clinical symptoms of menopause after hysterectomy due to uterine fibroids. Besides of the high frequency of reproductive function disorders, we have found that patients with AIA have thyroid pathology twice as often as patients with ATA. Functional deficiency of many organs in the endocrine system is evidenced by the early development of asthma attacks after the glucocorticoid (GC) hormones’ cessation or the decrease of its dose. According to our data, 28.6% of patients aged 16–29 years with AIA had a steroid dependency of the asthma course, compared to 2.7% of ATA patients. Its frequency remains almost at the same level (19%) in middle and mature years, and decreases to 12.4% among elderly patients with AIA. The coinciding ages (16–29 years) of GC’s dependency and reproductive function disorders in patients with AIA may confirm that the formation of GC dependency is caused by damage to central elements that regulate the GC’s function of the adrenal cortex.
Patients with AIA often have chronic comorbidity of other organs and systems, mainly diseases of upper respiratory tracts. This has been noted by other researchers who pointed to...