eBook - ePub
Minimized Cardiopulmonary Bypass Techniques and Technologies
- 272 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Minimized Cardiopulmonary Bypass Techniques and Technologies
About this book
Traditional cardiopulmonary bypass (CPB) techniques have suffered from a number of disadvantages including haemodilution, inflammation and post-operative bleeding. Minimised cardiopulmonary bypass techniques use developments in perfusion technology to significantly reduce foreign surface-blood interactions to make bypass simpler and safer. This important book reviews key developments and issues relating to this promising technology.Part one covers the broad range of CPB pathophysiology, including anticoagulant protocols, the impact of CPB circuit surfaces, optimal haemodilution levels, and the important issue of CPB-induced systemic inflammatory response syndrome. Part two focuses on the issues of the new equipment developed for mini-CPB, optimal myocardial protection protocols and CPB perfusate options. Part three discusses clinical issues, including patient selection, coronary and valve surgery protocols and, among others, paediatric patients.With its distinguished editors and international team of expert contributors, Minimized cardiopulmonary bypass techniques and technologies is a valuable reference for cardiac surgery teams and those researching this important technology.
- Covers a broad range of cardiopulmonary bypass (CPB) pathophysiology, including anticoagulant protocols, the impact of CPB circuit surfaces and optimal haemodilution levels
- Focuses on new equipment specially developed for minimized-CPB and myocardial protection protocols
- Discusses clinical issues, including patient selection
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
1
Historical development of minimised cardiopulmonary bypass
T. Gourlay, University of Strathclyde, UK
Abstract:
This chapter discusses the history of the development of technologies for minimising the cardiopulmonary bypass (CPB) system while addressing issues of perfomance, safety and convenience. Technologies that moderate complications of CPB include membrane-based oxygenator materials, surface modification, active filtration, autotransfusion, novel pumping systems and many other pharmacological interventions and clinical techniques. Factors affecting safe deployment of mini-bypass systems include concern over passage of air through the system and the need for a team-focused approach to safe perfusion delivery. These factors are discussed with reference to general perfusion concepts.
Key words
minimised cardiopulmonary bypass
cardiac surgery safety
membrane oxygenators
1.1 Introduction and historical perspective
Cardiopulmonary bypass (CPB) has been in clinical use for over half a century, and perhaps not surprisingly given global technological progress over this period, CPB technologies have undergone considerable development, reflecting many of the technological and material advances that have impacted on the wider society over this period.1 In particular, CPB systems have benefited from improved materials, electronics and computer technology.2–4 However, despite the many technological advances which have added to the quality of the extracorporeal support delivered to the open-heart surgical (OHS) patient, the perfusion system employed over 50 years ago would be largely recognisable to the modern clinical specialist. There are, nevertheless, many differences between ‘antique’ perfusion systems and their modern counterparts, and because of the better understanding of the processes and mechanisms that contribute to the pathophysiology of CPB that has been gained through long clinical experience and laboratory experimentation, the modern CPB system, in the right hands, is safer for the patient in all respects. As the CPB system has evolved over the decades, there have been a number of interesting dichotomies in terms of its size and complexity. On the one hand the core technologies, blood pump, blood oxygenator, heat exchanger and suction system have remained at the heart of the system, with some change in form, but little in terms of function. Whereas, on the other hand, the scope of the system has changed, increasing considerably in complexity to encompass other ancillary functions such as blood cardioplegia delivery, blood salvage and cell concentration and often haemoconcentrator and filtration technologies. However, despite this increase in complexity, the overall size of the perfusion system, in terms of surface area and priming volume has decreased considerably. This reduction in size has been driven by research that has demonstrated that haemodilution and blood/biomaterial contact contributes significantly to the common complications associated with CPB. In this chapter, we discuss the development of CPB since its earliest clinical delivery to modern times, with a focus on factors which have precipitated this reduction in size, leading to what is now known as ‘mini-CPB’.
1.2 Cardiopulmonary bypass: from pioneering to refinement
It is probably fair to say that when Gibbon performed the first of his CPB-supported heart-surgery procedures in 1953, the size of the heart/lung machine was the very least of his concerns.1 This first successful deployment of the heart/lung machine in the clinical setting formed the basis for a new surgical speciality leading to OHS as we know it today. The technology employed in this first CPB- supported procedure was innovative in its time, incorporating roller blood pumps and a screen-type oxygenator, and having a substantial surface area and a significant blood/gas interface (Fig. 1.1).

1.1 Gibbon’s heart/lung machine apparatus as employed in the earliest clinical procedures.
That this was an emerging technique is suggested by the fact that the heart/lung machines employed in this early era were constructed of materials employed for other more mundane applications, such as beer pump tubing, and industrial pumping systems, and that the devices were often reuseable and assembled before deployment. The utilisation of conventional, non-medically focused materials in the construction of a heart/lung machine apparatus is probably best illustrated by the system utilised by Lillehei in the mid 1960s (Fig. 1.2).5
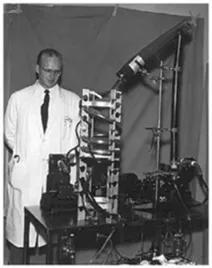
1.2 Lillehei with his bubble oxygenator which was manufactured using tubing sourced from the brewing industry and other industrial parts.
As the heart/lung machine development progressed, further mechanisms for gas exchange and blood pumping evolved from rotating disk and bubble oxygenators through to membrane oxygenators and from ‘finger’ and roller pumps through to more recent innovations including centrifugal and other kinetic pump systems (Fig. 1.3). Each advance resulted in a reduction in surface area.
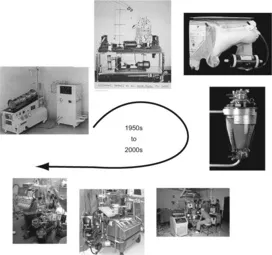
1.3 Blood oxygenators through the ages.
Complications associated with the deployment of CPB were identified fairly early in its clinical evolution, with ‘pump lung’ or post-pump syndrome, a complication which we now understand to be associated with the activation of inflammatory processes and which causes considerable concern. However, it was not until the 1980s when diagnostic techniques for assessing the activation of inflammatory processes and associated pathways were refined sufficiently for clinical investigation, that the role of the heart/lung machine, and in particular blood contact with the foreign surfaces of the system was identified as a key factor in the aetiology of this complication.6–13 Other factors contribute to the pathophysiology of CPB, including: haemodilution; haemodynamic disruption associated with the deployment of nonpulsatile pumping systems; and haemostatic problems associated with both haemodilution and the consumption of clotting factors associated with blood/biomaterial incompatibility.14–17 Early attempts to moderate these effects using surface coatings including heparinisation were successful to some degree, but offered little by way of reducing the inflammatory response.18–21 The influence of the expanse and volume of the heart/lung machine on these complications has been considered for some time. Some smaller, although by modern standards still unacceptably large, systems were developed in the early years of CPB evolution, showing early recognition of the size factor.22 Further development over the ensuing half century resulted in smaller, more convenient and efficient systems with novel surface modification technolologies applied to address the most common complications of CPB.23–27 Despite the development of a range of technologies designed to address the most common and challenging complications of CPB, the challenges persist to this day.28,29 The size factor remains one of the factors of CPB that can be influenced by research and development of novel technologies. There are, however, limits to the level of reduction in system size that can be achieved, the limitations being associated with performance and the need for some degree of reserve capacity to cope with the dynamic clinical setting. There is, therefore, a size/performance dilemma that impacts upon the shape of devices thhat may be developed in the future. Those involved in the development of new perfusion technologies must consider both the safety and performance requirements of the clinical setting in the design process. It is not acceptable for a new technology to address some of the common pathophysiologies of CPB, if by doing so the safety envelope of the new devices is rendered too narrow, and safe operation is therefore made more complex than existing approaches.
1.3 Cardiopulmonary bypass: does size matter?
The size of the CPB system can be considered in terms of both the area of the blood contacting surfaces and the volume of the system. Both of these factors have been shown to have an influence upon the management of the OHS patient. CPB systems having a large volume require more priming solution to ensure that they are air-free for safe deployment. This priming volume has reduced considerably over the past 50 years or so from very large systems requiring priming with up to 6 l of priming solution composed of blood and saline, to modern systems which are often deployed using low priming volumes or indeed autologous priming strategies.30–32 The high levels of haemodilution associated with early CPB systems were thought to be beneficial to the patient to some degree, as they resulted in reduced viscosity and improved perfusion of the microcirculation. However, there is considerable evidence that high levels of haemodilution, although improving peripheral perfusion, introduce other complications, particularly those associated with reduced oxygen-carrying capacity and reduced relative levels of platelets and clotting factors such as postoperative bleeding.33–38 These problems were of lesser importance during the pioneering phase of CPB when patient survival was the greatest consideration, but they assumed more significance during the period of refinement in the CPB field, when improvements in patient morbidity and mortality received greater attention. In recent years, clinical practice has changed in terms of levels of haemodilution and cir...
Table of contents
- Cover image
- Title page
- Table of Contents
- Copyright
- Contributor contact details
- Foreword
- Chapter 1: Historical development of minimised cardiopulmonary bypass
- Chapter 2: Anticoagulation protocols for minimized cardiopulmonary bypass
- Chapter 3: Minimized extracorporeal circulation: physiology and pathophysiology
- Chapter 4: Blood–surface interface in miniaturised extracorporeal circulation systems
- Chapter 5: Hemodilution: physiology and pathophysiology
- Chapter 6: Inflammatory response and minimized cardiopulmonary bypass
- Chapter 7: Design and principles of the minimized extracorporeal circuit
- Chapter 8: Cardiopulmonary bypass perfusate
- Chapter 9: Myocardial preservation techniques for mini-bypass
- Chapter 10: Minimised cardiopulmonary bypass: objectives and indications
- Chapter 11: Coronary artery bypass grafting (CABG)
- Chapter 12: Valve surgery using minimized perfusion circuits
- Chapter 13: Minimising cardiopulmonary bypass in children
- Chapter 14: Comparison of minimized circulation with off-pump coronary artery bypass (OPCAB) grafting and conventional surgery
- Chapter 15: Minimally invasive cardiac surgery, port-access and robotic surgery
- Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Minimized Cardiopulmonary Bypass Techniques and Technologies by Terence Gourlay,Serdar Gunaydin in PDF and/or ePUB format, as well as other popular books in Medicine & Biotechnology in Medicine. We have over one million books available in our catalogue for you to explore.