![]()
Part One
Understanding Burnout
Effective definitions should drive solutions—practical and pragmatic ways in which to put those definitions to work in increasing resilience and decreasing burnout. There are three fundamental insights:
1. Every member of the healthcare team is a leader and requires leadership training—Lead Yourself, Lead Your Team
2. Every healthcare team member is a performance athlete, engaged in a cycle of performance, recovery, rest, and repeat performance—Protect Yourself, Protect Your Team
3. The work begins within—while organizational culture and systems need to change, we must always seek to reconnect our “deep joy” that brought us to healthcare in a “passion reconnect”
Chapter 1, “Why Burnout Matters,” succinctly makes the case that every known metric by which to gauge quality in healthcare gets dramatically worse with burnout. Burnout itself is a ratio of increasing job stressors divided by the resilience/ adaptive capacity to deal with those stressors. Resilience has many definitions, but the most pragmatic is that it is simply the adaptive capacity to deal with healthcare’s abundant stressors. Christina Maslach and Michael Leiter’s seminal work on burnout delineates the six domains of burnout: mismatch of workload demands and capacity, loss of control, loss of rewards and recognition, lack of community, lack of fairness, and loss of values. In order to devise solutions for burnout, it is important to understand the causes of burnout, include both commonalities and differences among physicians, nurses, essential services, and other team members. The cost of burnout is staggering and is delineated in detail, which helps those motivated to launch initiatives to battle burnout to make the case for a return on investment (ROI) to the leadership team.
All meaningful and lasting change is driven by intrinsic motivation and an understanding of “getting the ‘why’ right before the ‘how.’” The most important reason to battle burnout and build resilience is that it makes our jobs easier while making our patients’ lives better. Similarly, the most effective way to hold a team accountable is mutual accountability through leadership at all levels. Finally, in an age where metrics matter, a discussion of the measures of burnout and resiliency is presented in detail.
![]()
1
Why Burnout Matters
Knowing what we know gives us peace. But knowing what we don’t know gives us wisdom.
CONFUCIUS1
The Way We’re Working Isn’t Working
What if half of the physicians, nurses, and healthcare team members providing care to you and your family were burned out? How confident would you be that a team with half its members suffering from burnout would deliver optimal quality of care? That prospect is today’s unsettling reality. Burnout has reached epidemic proportions, affecting up to 60 percent of physicians and 50 percent of nurses, depending on specialty.2–6 The costs of burnout to organizations and providers are devastating, with negative effects on employee turnover, patient safety, quality, productivity, and personal health.7 The challenge of dealing with the coronavirus pandemic did not create the epidemic of burnout, but it did accentuate it, as well as the necessity for actionable solutions.8
Simply stated, the way we’re working isn’t working. How could it be working when half of our team members suffer burnout and the consequences are so high? Our only hope is to exert inspired leadership to change these realities. The definition of burnout will be discussed in more detail later, but it can be succinctly stated:
Burnout is a mismatch between job stressors and the adaptive capacity or resiliency required to deal with those stressors, which results in three cardinal symptoms:
1. Emotional exhaustion
2. Cynicism
3. Loss of a sense of meaning in work9
In addition to this definition, this book relies on three additional insights:
1. Every member of the healthcare team is a leader who needs leadership skills to
• lead yourself, lead your team
• lead their team
2. Every member of the healthcare team is a performance athlete engaged in a cycle of performance, training, and recovery.
• Invest in yourself.
• Invest in your team.
3. The work begins within. Start with what you can control: you.
(As Marcus Aurelius noted, if you want good in the world, you must first find it in yourself.) Finally, as Bryan Sexton, a professor at Duke, points out, at a personal level, burnout results in a diminished ability to experience the restorative effects of positive emotions, as if a veil stood between us and our passion.10
Why does burnout matter? Is it simply an annoyance, or is it a deep problem infecting our ability to deliver quality patient care by committed, passionate clinicians and the team supporting them? How common is the problem, and what differences are there among our team members? How and why does it happen? How does it affect patients, those caring for patients, and the broader healthcare system? This chapter summarizes what is currently known regarding these questions, with the intent of helping guide solutions. It also lists what we don’t know.
Burnout matters for five reasons:
1. Burnout is human suffering among our healthcare teammates, blunting our ability to feel positive emotions.
2. Burnout is common, affecting up to 50 percent of physicians and nurses.
3. Burnout is expensive, costing the healthcare system $4.6 billion per year.11
4. Every measure by which we monitor progress in healthcare gets worse with burnout.
5. There is no “meter” or “gauge” on our foreheads indicating, “Danger—this person is burned out.”
Leadership is essential to preventing and treating burnout—lead yourself, lead your team.
Prevalence of Burnout in Healthcare
The prevalence of clinician burnout has been studied extensively, with most of the work with physicians and nurses. The simplest answer to “Who burns out?” is “Everyone, to varying degrees.” Let’s examine the data.
PHYSICIANS
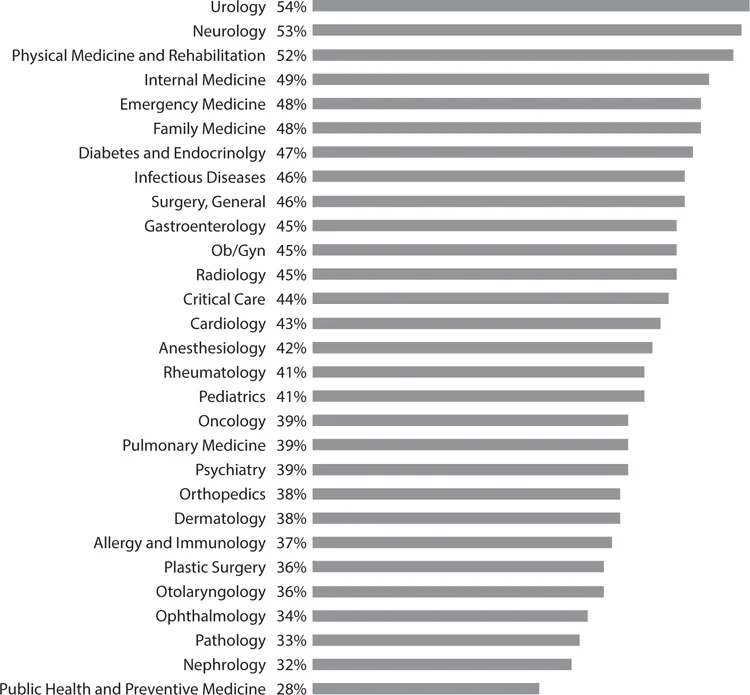
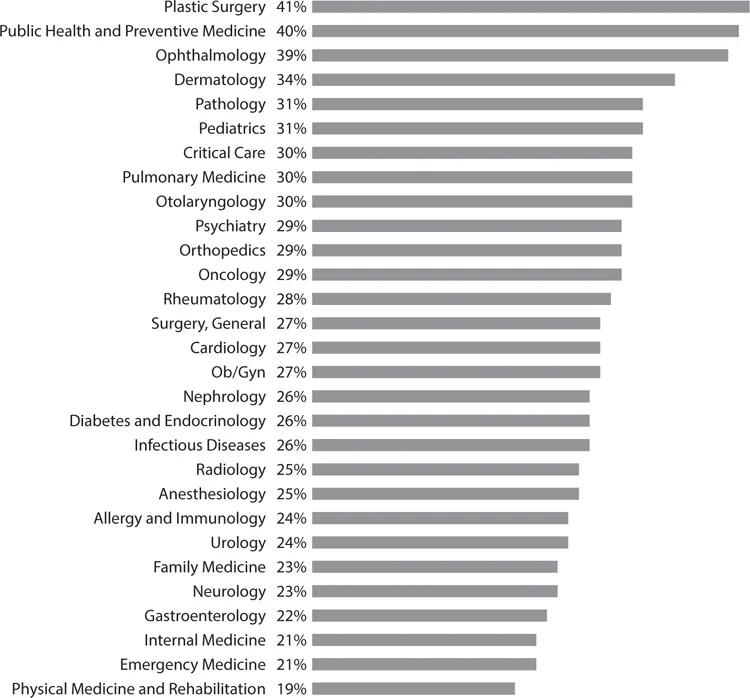
Current data indicate that a minimum of 40–55 percent of physicians have experienced significant symptoms of burnout, with higher rates among physicians on the front lines of medicine who have extensive direct patient care responsibilities, including those in emergency medicine, family medicine, general internal medicine, critical care medicine, and neurology (Figure 1-1).12–14 Conversely, those physicians who rated themselves as the happiest are largely those off the front lines of medicine and in specialties in which patient care is more elective in nature (Figure 1-2).15 James Reason cites Shakespeare’s Henry V, “We are but warriors for the working day,” and then states that emergency physicians and nurses “stand on the front line between the hospital (the rear echelons) and the hostile world of injury, infections, acute illness. The nature and extent of these enemies are not really known until the moment of the encounter. And the encounter itself is brief, singular, hugely critical, largely unplanned and full of surprises and uncertainties. These skirmishes offer an almost unlimited number of opportunities for going wrong.”16
Figure 1-1: Burnout Rates among Physician Specialties13
Figure 1-2: Physician Self-Ratings of Happiness at Work13
Viewed from this perspective, it is not surprising that we sometimes get it wrong on the front lines of medicine, but what is surprising is that we so often get it right.17 Given the type and volume of stressors to which physicians and nurses are constantly exposed, it isn’t surprising that nearly half of them have burned out—but it is surprising that figure isn’t even higher.
Burnout is nearly twice as common in physicians when compared with other US workers after controlling for other factors, including work hours.18 Recent data reiterate that this is the case, even though physicians have been shown to have higher resiliency,19 accentuating the magnitude of the problem. It is alarming that burnout is occurring at younger ages, with a high prevalence among medical students and residents compared with people of a similar age pursuing other careers.20
This is undoubtedly due in part to the fact that medical students, residents, and recent residency graduates have more concerns regarding work-life balance and related issues than in previous generations. Chuck Stokes, one of the most trusted voices in healthcare leadership, argues that the younger generation of clinicians will have to “constantly reinvent themselves” over the course of their careers, evolving their areas of interest and their span of practice to avoid burnout and sustain their passion.21
While all of these prevalence rates will undoubtedly change over time—and hopefully some of the strategies designed to prevent and treat burnout will be effective—it is safe to say that no less than 35 percent and as much as 50 percent of physicians have substantial symptoms of burnout. It is a staggering insight when you consider that every other doctor may be burned out, particularly when the costs of burnout are considered, from decreased quality of care to effects on patient safety, even before financial costs are calculated.22–24
NURSES
Linda Aiken and her colleagues at Penn did the earliest and most extensive work on nurse burnout rates, which have typically been reported to be between 35 and 40 percent.25–26 They noted in a 2002 study of over 10,000 inpatient nurses that 43 percent reported a high degree of emotional exhaustion.27 (Most of the work done on nurse burnout has focused on the emotional exhaustion aspect of the Maslach Burnout Inventory, which arguably may skew the picture when comparisons are made to physician burnout data. For this and other reasons, further work...