
eBook - ePub
Dilemmas in Abdominal Surgery
A Case-Based Approach
Savio George Alberto da Piedade Barreto, Shailesh Vinayak Shrikhande, Savio George Alberto da Piedade Barreto, Shailesh Vinayak Shrikhande
This is a test
Share book
- 282 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Dilemmas in Abdominal Surgery
A Case-Based Approach
Savio George Alberto da Piedade Barreto, Shailesh Vinayak Shrikhande, Savio George Alberto da Piedade Barreto, Shailesh Vinayak Shrikhande
Book details
Book preview
Table of contents
Citations
About This Book
This book covers the management of surgical diseases "through the eyes" of a clinician by providing an evidence-based approach to specific clinical dilemmas. The chapters take the reader through a step-by-step "decision-making" approach to commonly encountered, but difficult to manage, situations where the editors share their rationale behind the process. Emphasis is placed on the use of tables and algorithms to simplify understanding. They aim to empower the readers with the ability to manage complex abdominal surgery scenarios in a streamlined manner, thus improving the care and outcome of patients.
Key Features
-
- Targets specific, difficult to manage scenarios
-
- Provides expert opinion/advice on how to tackle tricky situations
-
- Covers both benign and malignant cases
- Examines surgical dilemmas through illustrations
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Dilemmas in Abdominal Surgery an online PDF/ePUB?
Yes, you can access Dilemmas in Abdominal Surgery by Savio George Alberto da Piedade Barreto, Shailesh Vinayak Shrikhande, Savio George Alberto da Piedade Barreto, Shailesh Vinayak Shrikhande in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
PART 1
ESOPHAGUS
1 Acute Presentation (Boerhaave’s Syndrome)
Jon Shenfine
CONTENTS
Case scenario
Background of the pathology
Approach to management
Clinical findings (symptoms and signs)
Investigations: To arrive at a diagnosis and plan treatment
Computed tomography (CT)
Plain radiography (chest X-ray)
Contrast radiography
Upper gastrointestinal endoscopy
Treatment options with benefits and risks
Non-operative management
Adjuncts to non-operative management
Operative management
Conflicts of interest
References
Case scenario
A 48-year-old man presented to the emergency department with severe, excruciating chest pain. He had spent the day with his family, drinking alcohol and eating a large dinner. At 21:00 he felt nauseated and vomited. There was a tearing sensation in his chest and he collapsed in agony on the floor. He presented in severe pain despite opioid analgesia. He was pale, short of breath, and peripherally shutdown. His voice was weak and high pitched; he was distressed with pain and sweat. He had subcutaneous emphysema over the chest wall, but his abdomen was soft to palpate. His pulse rate was 120 bpm and his blood pressure was 100/60. His electrocardiogram was normal and his chest radiograph confirms subcutaneous emphysema.
Background of the pathology
This is a classical presentation of a “spontaneous perforation of the esophagus” or Boerhaave’s syndrome which is a barogenic, esophageal injury [1]. Although various degrees of damage and contamination are possible, spontaneous perforation of the esophagus is most accurately defined as a full-thickness disruption of the esophageal wall occurring in the absence of pre-existing pathology, and typically leads to immediate and gross gastric content contamination of the mediastinal and pleural cavities. This progresses rapidly to a life-threatening chemical and septic mediastinitis.
The injury is nearly always associated with a sudden rise in intra-abdominal pressure, most usually as a result of retching or vomiting, hence the term “barogenic”. Vomiting is commonplace but spontaneous esophageal perforation is not, which suggests that there may be unidentified anatomical or perhaps pathological abnormalities that underlie the injury. An underlying pathology, such as malignancy, peptic ulceration, infectious, or eosinophilic esophagitis is identified in only 10–20% of cases and these cases do not truly represent spontaneous perforations. Another common misconception is that Mallory–Weiss tears are a lesser but related injury. However, it is more likely that these mucosal injuries reflect “shearing” rather than “barogenic” trauma.
Spontaneous perforations are invariably single, longitudinal, between 1–8 cm long, and with the mucosal injury being longer than the muscular tear. They tend to occur in the left posterolateral position just above the esophagogastric junction. Pleural perforation can be immediate or delayed and transgression of esophagogastric contents is exacerbated by the negative intrathoracic pressure. Men are more often affected, in a ratio of 4:1, which may reflect a tendency to overindulge in alcohol and vomit rather than a gender difference.
Approach to management
Clinical findings (symptoms and signs)
Patients with Boerhaave’s syndrome classically present with sudden onset of chest pain following vomiting, and the subsequent development of subcutaneous emphysema. The associated pain is constant, retrosternal, severe, exacerbated by movement, and poorly relieved by opioid analgesia. Patients are usually tachycardic and tachypnoeic. Mediastinal emphysema develops rapidly and can be seen on a plain chest radiograph, as can a hydropneumothorax once the pleura is breached. There is an early low-grade pyrexia due to the chemical pleuro-mediastinitis, worsening as the systemic inflammatory response gives way to sepsis. Within 24–48 hours, bacterial mediastinitis and systemic circulatory collapse supervene; survival is dependent on the removal of the contamination from the mediastinal and pleural cavities at the earliest opportunity.
However, classical is not the same as typical, since patients with spontaneous perforation of the esophagus can present in many ways. The temporal relationship of the barogenic event to the development of the chest pain is frequently overlooked due to the severity and associated cardiopulmonary collapse. The pathognomonic development of subcutaneous emphysema takes time to evolve, and abdominal pain and tenderness are also not uncommon and can lead to a negative laparotomy. The combination of chest pain and shock commonly lead to an early cardiology opinion and significant diagnostic delay. The diagnosis becomes more obscure as time passes due to circulatory collapse. As a result, the diagnostic error is high and only 5% of cases are diagnosed at presentation, with delay being the norm rather than the exception. Some cases may not even be correctly diagnosed pre-mortem.
The most important factor in making the diagnosis is a high index of suspicion in someone with severe chest pain following an episode of violent vomiting.
Investigations: To arrive at a diagnosis and plan treatment
Computed tomography (CT) (Figure 1.1)

CT chest and abdomen with intravenous and oral contrast is the first choice in diagnostic imaging for stable patients. In an intubated patient, a nasogastric tube can be placed in the proximal esophagus to run a small amount of water-soluble contrast in to increase the sensitivity of detecting a leak. CT also plays a significant role post-therapy to assess ongoing leakage and healing and guide the need for further intervention with serial studies.
Plain radiography (chest X-ray)
The commonest associated findings on plain radiography are of pleural effusion, pneumomediastinum, subcutaneous emphysema, hydropneumothorax, pneumothorax and lung consolidation or collapse. However, these can be subtle and develop over time.
Contrast radiography
Water-soluble oral contrast radiography has been superseded by CT since the logistics of their performance are frequently limited in patients who are in shock. However, their dynamic nature gives information about the degree of containment and the degree of drainage of the perforation. They also remain useful post-treatment to assess progress of healing.
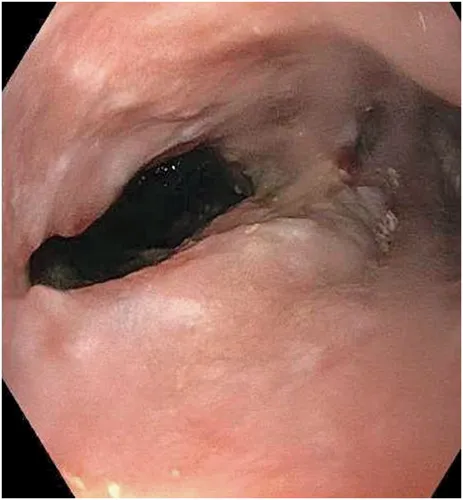
Upper gastrointestinal endoscopy
Endoscopy was previously avoided due to the perceived risk of insufflation and increase in size of the perforation. However, this has not borne out and can be performed in the most unwell of patients, preferably “on table”, safety being enhanced by being performed by a highly experienced endoscopist under a general anesthetic with the patient intubated (Figure 1.2). Endoscopy can influence management if underlying pathology is discovered and allows the placement of a nasojejunal tube or adjunctive therapies such as clipping a defect, lavage of a perforation cavity, or the placement of a “vacuum” endo-sponge as a potential therapeutic option in contained perforations with no gross contamination (see treatment) (Figure 1.3).

Treatment options with benefits and risks
All patients with an esophageal perforation are critically ill. The immediate priority is resuscitation: establishing a secure airway, stabilising the cardiovascular system, relieving pain, and administering broad-spectrum antibiotics, antifungals and anti-secretory medication (see Box 1.1). An initially stable patient can rapidly decompensate, and early anesthetic review is strongly recommended. Ultimately, patients will benefit from a multidisciplinary approach with input from intensive care, radiology, physiotherapy, dieticians, and rehabilitation services. Hospitals lacking these specialists or the expertise necessary to deal with esophageal surgery should transfer the patients as soon as possible after initial stabilisation. Survival is dependent on controlling sepsis, so prompt surgery remains obligatory when there is significant contamination. Non-operative treatment is sometimes feasible when contamination is limited and there has been minimal delay.
Box 1.1 Initial resuscitation in spontaneous esophageal perforation
- Control of airway and administration o...