![]()
1
HISTORY OF
TRANSSEPTAL CATHETERIZATION
GREGORY K. FELD, JOHN ROSS JR.
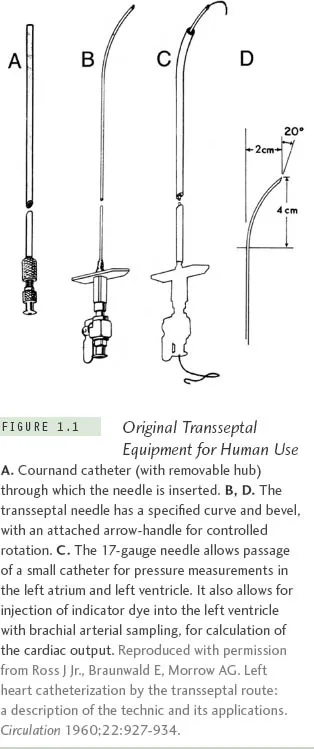
Transseptal left heart catheterization, originally developed in experimental animal studies and then later in humans, was reported in 1959 by John Ross Jr, MD, at the National Institutes of Health (NIH).1-4 It was first used to measure left heart pressures as a diagnostic method and later as a research tool to study left heart dynamics in human diseases such as heart failure, heart valve dysfunction, and hypertrophic obstructive cardiomyopathy.4,5,* In 1960, the needle used for transseptal catheterization (Figure 1.1) was slightly modified with a smaller needle tip by Edwin Brockenbrough, MD, a trainee in the NIH cardiovascular research program, for use with a larger catheter passed percutaneously by the Seldinger method.7 Subsequently the procedure became widely used as a diagnostic method to assess left atrial and left ventricular pressures in both adult and pediatric patients with valvular and congenital heart disease who were being considered as candidates for surgical repair procedures.8-10 With the developments of right heart, balloon, and thermodilution (Swan-Ganz) catheterization to estimate left atrial pressures11 and retrograde left ventricular catheterization, transseptal catheterization became less widely practiced in the 1970s and early 1980s, except in those centers performing procedures, such as mitral balloon valvulotomy, which require transseptal puncture.
During the 1980s, however, at a time when clinical cardiac electrophysiology was primarily a diagnostic specialty, the use of electrical fulguration for atrioventricular (AV) node ablation, septal accessory pathway ablation, and ventricular tachycardia ablation was described,12-13 rapidly advancing cardiac electrophysiology into an interventional specialty. Fortunately, considering the limitations of high-energy shocks for ablation, including the high failure rates and risks of complications from this technique,12-13 radiofrequency energy for catheter ablation was described.14 This led to an explosion in the use of catheter ablation to cure a variety of cardiac arrhythmias, including AV reentry,15-16 AV nodal reentry,17 atrial flutter,18-19 atrial tachycardia,20and ventricular tachycardia.21
In many cases, however, the successful application of radiofrequency energy via catheter for curative ablation required access to the left atrium and left ventricle. This was particularly true for left-sided accessory pathways,15-16 left ventricular tachycardia,21 atrial fibrillation and atypical atrial flutter.22 While often this could be accomplished by retrograde arterial catheterization across the aortic and mitral valves, usually from the femoral artery or rarely from the radial artery, in many cases easier access could be achieved by a transseptal catheterization approach. Thus, for the treatment of a variety of supraventricular and ventricular tachyarrhythmias there was a gradual resurgence in the use of transseptal catheterization in the field of interventional cardiac electrophysiology, beginning in the 1980s; this use increased dramatically in the 2000s as ablation of atrial fibrillation became widely practiced.
Thus, in the cardiac electrophysiology laboratory, transseptal catheterization has become particularly useful for obtaining access to the left atrium for radiofrequency catheter ablation of left-sided accessory pathways in patients with Wolff-Parkinson-White syndrome and refractory supraventricular tachycardia,23-25 in the occasional patient with failed right-sided slow or fast pathway ablation for AV nodal reentrant tachycardia,26-27 in those with failed right-sided AV node ablation for refractory atrial fibrillation,28 and in those with left ventricular tachycardia in whom access to the left ventricle is required for both mapping and ablation.29-30 Large numbers of transseptal catheterization procedures have been performed at numerous institutions worldwide over the last several decades, including many in electrophysiology laboratories, with very high success and very low complication rates,31 even if performed on an outpatient basis.32 The most serious potential risks from transseptal catheterization include cardiac or aortic perforation with pericardial effusion and tamponade, which may require percutaneous pericardial catheter drainage and, occasionally, surgical intervention.
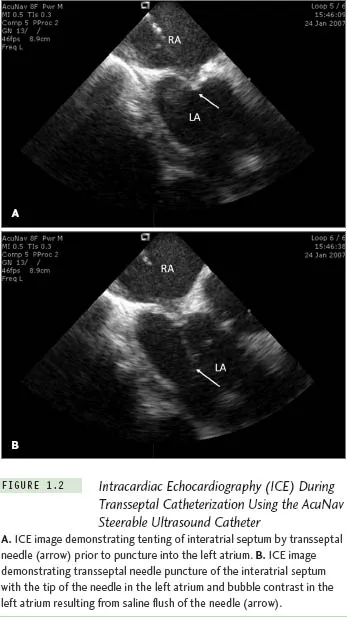
While the technique of transseptal catheterization remains largely unchanged since it was originally described and modified,14 several new technologies have made the approach considerably easier and potentially less risky, and are routinely employed today in many clinical electrophysiology laboratories. These new technologies include transesophageal echocardiography,33 now largely replaced by intracardiac echocardiography (ICE),34-37 to guide transseptal puncture, transseptal puncture performed using radio-frequency energy applied to a modified transseptal needle (NRG RF Transseptal Needle, Baylis Medical Company, Inc, Montreal QC, Canada), or use of a needle-tipped guidewire (SafeSept Transseptal Guidewire, Pressure Products, Inc, San Pedro, CA) passed through a standard Brockenbrough transseptal needle into the left atrium through a variety of pre-shaped transseptal sheaths (Fast-Cath, St. Jude Medical, Inc, St. Paul, MN). With the use of ICE, typically performed with a steer-able 8 F or 10 F intracardiac ultrasound catheter (AcuNav, Siemens Medical Solutions USA, Inc, Malvern, PA), contrast injection to stain the septum is no longer required, since micro-bubbles in the saline flush provide adequate echo-contrast to ensure successful left atrial access, reducing the risk of cardiac perforation with the transseptal needle (Figure 1.2). The radiofrequency transseptal needle38 and the needle-tipped guidewire further reduce the risk of inadvertent needle perforation of the left atrial lateral wall or roof during transseptal catheterization. For ablation of left-sided accessory pathways, a numbered series of transseptal sheaths (eg, SL1, SL2 [Daig Corp, Minnetonka, MN]) with different lengths of the distal-shaped segment was developed that, when extended just beyond the sheath, position the ablation catheter at specific locations around the mitral valve annulus (Fast-Cath, St. Jude Medical, Inc, St. Paul, MN).
With the recognition that electrical isolation of the pulmonary veins with radio-frequency catheter ablation may cure atrial fibrillation,39 an entirely new procedure in interventional cardiac electrophysiology was launched in the late 1980s, namely the ablation of atrial fibrillation. This approach required transseptal catheterization of the left atrium and, in most cases, double transseptal catheterization (Figure 1.3) because both a circular mapping catheter and an ablation catheter need to be introduced into the left atrium to ensure successful isolation of the pulmonary veins. This can be accomplished either by performing two separate transseptal punctures33-37 or a single transseptal puncture40 through which an ablation catheter is guided either by ICE or fluoroscopy after withdrawing the sheath (through which the initial puncture was made) back into the right atrium while retaining a guidewire in the left atrium. Once the ablation catheter is passed through the transseptal puncture into the left atrium, the retained sheath can be passed over the guidewire back into the left atrium, through which the circular mapping catheter can then be deployed in the left atrium for mapping the pulmonary veins. Both approaches may be guided by ICE, and recent advances in 3-D echo may further enhance success and reduce the risks of the procedure. Studies suggest that long-term complications are similar with either approach, and while the single transseptal puncture approach may result in patency of the puncture site for a longer period of time than the double transseptal puncture approach, closure eventually occurs with either approach.41
Another aspect of transseptal catheterization that has evolved with the advent of atrial fibrillation ablation has been the use of intensified anticoagulation regimens for prevention of thromboembolic events, including maintaining an activated clotting time (ACT) >350 seconds during abla...