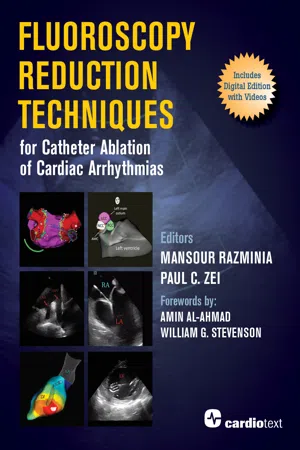
Fluoroscopy Reduction Techniques for Catheter Ablation of Cardiac Arrhythmias
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Fluoroscopy Reduction Techniques for Catheter Ablation of Cardiac Arrhythmias
About this book
Background: Catheter ablation has become a widely used approach to treating various cardiac arrhythmias. Traditionally, catheter ablation procedures are guided by fluoroscopic imaging to help understand catheter position during mapping. The potentially significant exposure to radiation to the patient, physician, and staff increases risks of radiation exposure-related disease. Also, the protective lead garments worn increases risks of orthopedic injury. Current advanced electroanatomic mapping and intracardiac echocardiography technology have allowed the development of endocardial catheter ablation techniques without the use of fluoroscopy safely and effectively. A host of expert and experienced authors present a practical overview of the rationale and methodology for a low- or zero-fluoro environment in the electrophysiology lab with the critical goal of significantly reducing radiation exposure to the patient, physician, and staff.This practical guide: Covers the entire spectrum of commonly (and less commonly) performed ablation procedures via endocardial approach. Discusses general principles that are applicable across ICE and EAM platforms. Will assist the electrophysiologist and their team to safely and effectively work toward the significant reduction in fluoroscopy utilization while also likely improving procedural safety, i.e., fewer complications, after the adoption of these techniques. Includes a library of 50 videos, with 9 extended films (108 minutes) by Dr. Razminia detailing step-by-step procedures and techniques.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
Section 1
Electrophysiology Lab
1
Radiation Safety in the Electrophysiology Lab
Introduction

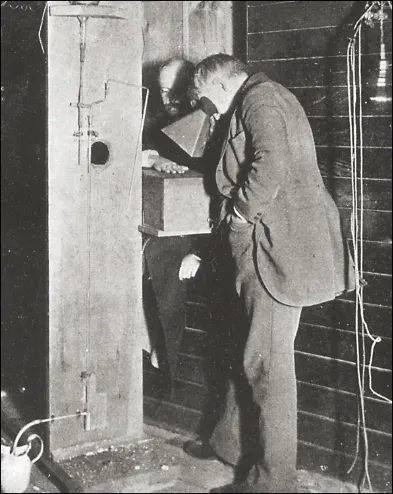
Radiation-Associated Risks

Malignancy Risk
Deterministic Risks

Indirect Exposure Risks
Table of contents
- Cover
- Title Page
- Copyright Page
- Dedication
- Contents
- Contributors
- Forewords
- Preface
- Abbreviations
- Video Descriptions
- Section 1: Basis of Imaging in the Electrophysiology Lab
- Section 2: Ablation of Supraventricular Tachycardia
- Section 3: Ablation of Atrial Fibrillation
- Section 4: Ablation of Ventricular Arrhythmias
- Section 5: Special Populations
- Author Disclosures
- Index