Equine Hematology, Cytology, and Clinical Chemistry
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Equine Hematology, Cytology, and Clinical Chemistry
About this book
The all-new Equine Hematology, Cytology, and Clinical Chemistry draws on hematology and clinical chemistry information featured in the first edition of Equine Clinical Pathology and adds valuable cytopathology material from Diagnostic Cytology and Hematology of the Horse, making it a truly definitive reference to clinical pathology in equids. Thoroughly updated and expanded throughout, this Second Edition offers more images, more information, and new knowledge for previous chapters and entirely new chapters on bone marrow evaluation and cytopathology.
Designed to present clear, concise, and clinically relevant information, the book is logically organized for easy reference. Numerous figures, tables and images support the text, together with summarized information for ease of use.
- Offers a focus on clinical pathology in the horse, with in-depth information on hematology, clinical chemistry, and cytopathology in equids
- Presents equine disease from a systems-based, clinicopathological perspective
- Features hundreds of high-quality images
- Includes contributions from veterinary specialists with expert knowledge of clinical pathology
A must-have purchase for anyone using hematology, clinical chemistry, and cytology in equine patients, Equine Hematology, Cytology, and Clinical Chemistry, 2nd Edition is a valuable resource for equine practitioners, clinical pathologists and residents, and veterinary students.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1
General Laboratory Medicine
1.1 Introduction to Laboratory Medicine
1.2 Preanalytical Factors
1.3 Basic Hematological Techniques
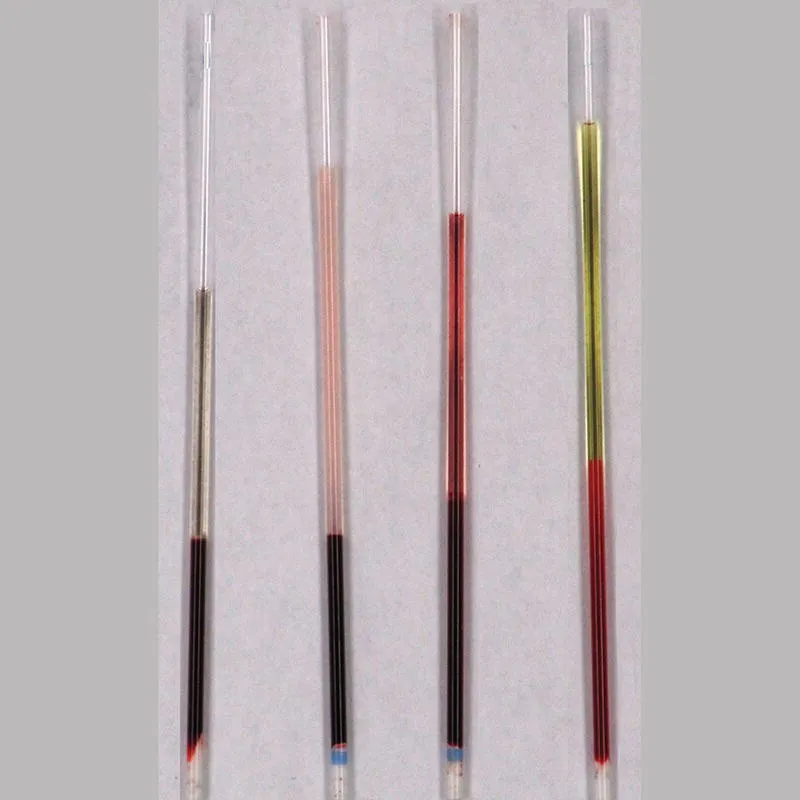
1.3.1 Packed Cell Volume and Plasma Evaluation: Disease and Artifacts
1.3.2 Protein Measurement by Refractometer
Table of contents
- Cover
- Table of Contents
- Title Page
- Copyright Page
- Dedication Page
- List of Contributors
- Preface
- 1 General Laboratory Medicine
- 2 Equine Hematology
- 3 Bone Marrow Evaluation
- 4 Immunohematology and Hemostasis
- 5 The Liver
- 6 The Kidney
- 7 Acid–Base and Electrolytes
- 8 Proteins
- 9 Laboratory Assessment of Lipid and Glucose Metabolism
- 10 Laboratory Markers of Muscle Injury
- 11 Endocrine Evaluation
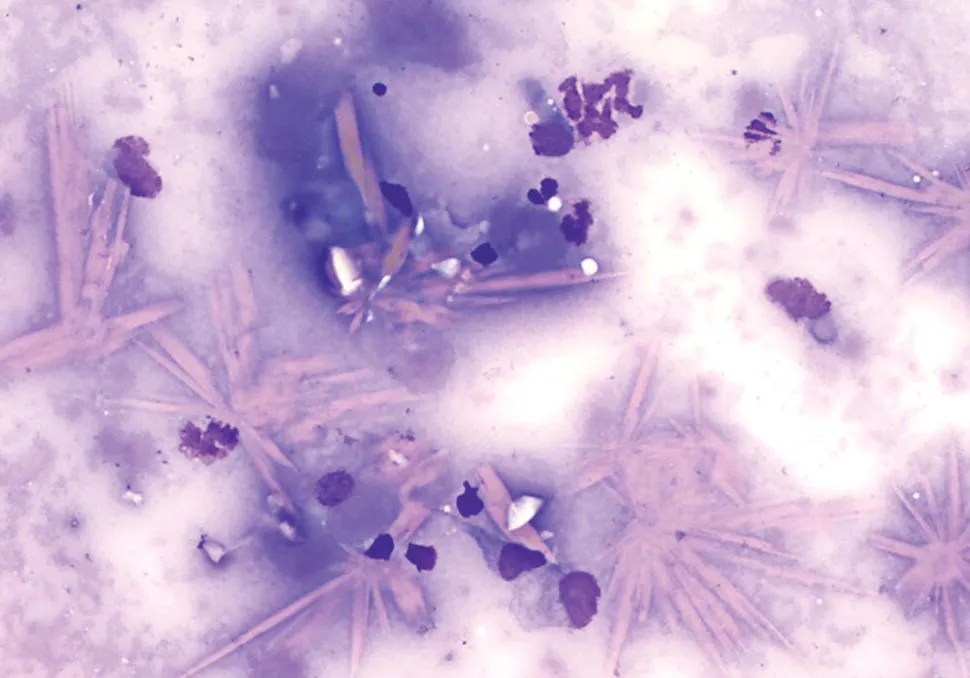
- 12 Cytology of Cutaneous and Subcutaneous Lesions
- 13 Cytology of the Eyes and Associated Structures
- 14 Cytology of the Oral and Nasal Cavities, Pharynx, Guttural Pouches, and Paranasal Sinuses
- 15 Cytology of the Lymph Nodes
- 16 Cytology of the Endometrium
- 17 Semen Evaluation
- 18 Pleural, Peritoneal, and Synovial Fluid Analysis
- 19 Cerebrospinal Fluid
- 20 Cytology of the Respiratory Tract
- Index
- End User License Agreement