eBook - ePub
Vascular and Endovascular Complications: A Practical Approach
- 314 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Vascular and Endovascular Complications: A Practical Approach
About this book
Prevention of complications in vascular and endovascular surgery is an important consideration for all practicing surgeons. The keys to achieving clinical success are based on careful selection of both patient and procedure, along with meticulous operative and endovascular techniques. Management of complications requires careful planning and urgent intervention.
This concise, practical text provides the reader with
- A stepwise approach to diagnosis
- Guidance on avoiding technical pitfalls
- Advice on re-interventions
- Case examples to aid clinical practice
The early diagnosis of complications, followed by prompt action and intervention, is key to improving clinical outcomes. This well-illustrated, concise, and practical book ensures that vascular and endovascular surgeons will be able to optimize clinical results and patient care.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Vascular and Endovascular Complications: A Practical Approach by Sachinder Singh Hans, Mark F Conrad, Sachinder Singh Hans,Mark F Conrad in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
Topic
MedicineSubtopic
Cardiology1
Preoperative risk assessment
As the prevalence of vascular disease increases within the population, one can expect a rise in the number of vascular interventions performed with a subsequent increase in the absolute number of complications that occur. Negative outcomes after vascular interventions can be categorized into three general categories: systemic, non-vascular, and vascular, and occur in direct proportion to the severity of patient comorbidities and complexity of the procedure.1 Vascular procedures can be stratified into emergent, urgent, and elective, and each level carries a different level of risk for the patients. Emergent procedures usually involve the arterial circulation and can include hemorrhage from aneurysm rupture or trauma, thromboembolic events leading to acute ischemia of the limbs or visceral organs, and malperfusion secondary to dissection of the arterial wall. Patients who require urgent procedures can present with venous thromboembolic events, stroke in evolution, symptomatic aneurysms, and infected extremities that require amputation or drainage. Both emergent and urgent problems limit the surgeon's ability to perform an adequate preoperative risk assessment and medial optimization, and, in these cases, a thorough history and physical in addition to optimization of medical comorbidities is ideal though may not always be feasible. Indeed, for these patients, the bulk of medical management occurs after completion of the procedure and is aimed at managing comorbidities rather than risk factor reduction and optimization. For patients undergoing elective vascular surgery, the best outcomes are enjoyed when the patient is medically optimized and operative risk is minimized. One strategy for achieving this goal is discussed in this chapter.
INITIAL WORKUP
For patients who do not require urgent or emergent interventions, a thorough history and physical should be performed with particular focus on significant cardiac, pulmonary, renal, endocrine, neurologic, vascular, or hematologic history. An understanding of the patient's activities of daily living, degree of independence, and exercise tolerance is critical. The cardiac history should take special note of any prior interventions, review of any previous electrocardiograms (ECG), echocardiograms, and/or any stress testing that may be available. A pre-operative ECG should be performed within 90 days of any elective procedures. Noninvasive stress testing is recommended for any patients with significant clinical risk factors such as coronary artery disease, congestive heart failure, diabetes, or chronic renal insufficiency.
Many vascular patients have some history of smoking with resultant underlying lung disease, so it is important to have a good understanding of the patient's baseline pulmonary functional status prior to any major procedure. The use of bronchodilators or need for home oxygen should be noted. Basic chemistries should be reviewed to evaluate for any underlying renal dysfunction, and any history of renal replacement therapy or transplant should be noted. A recent A1c should also be obtained given the relationship between postoperative complications and poor glycemic control. A thorough social history should also be obtained to evaluate for any lifestyle modifications such as smoking cessation and alcohol or drug misuse.
The history should also include any previous vascular interventions that the patient has undergone, including a review of previous operative notes. The identification of scars can help give insight into previous vascular procedures, which can be particularly helpful in patients who present without documentation or are unable to give a full surgical history. A baseline pulse exam should also be performed, and the absence of pedal pulses should lead to arterial noninvasive testing of the lower extremities. Any neurologic deficits should also be noted. Finally, a review of any hematologic disorders within the patient and immediate family should be identified as it could change management of anticoagulation status in the perioperative period.
PERIOPERATIVE IMAGING
The best imaging study for evaluation of specific vascular disease processes is addressed in their respective chapters. Indeed, the importance of obtaining appropriate perioperative imaging cannot be overemphasized as it provides insight into the degree of vascular disease, identifies variant anatomy, and is the first step toward avoiding perioperative complications through sound case planning. Computed tomography (CT) angiography is most useful for rapid identification of suspected pathology of the aorta and major vessels of the neck, thorax, and abdomen. However, it may have limitations in its ability to accurately characterize the patency or severity of stenosis of the smaller and more peripheral vessels. MR angiography is another option for patients with a contrast allergy or higher creatinine as vessel definition can be obtained without contrast with time of flight imaging. However, MR angiography can be time consuming and is contraindicated in patients that have certain metallic implants.3 Ultrasonography is a useful adjunct for evaluation of vascular pathology of the neck and extremities that can be used for surveillance and case planning. In addition, it can provide rapid evaluation of pseudoaneurysm, dissection, thrombosis, or stenosis.
CARDIAC COMORBIDITIES
The extent to which the heart must be evaluated prior to a vascular procedure is dependent upon the overall procedural risk, patient risk factors, and their exercise capacity. For instance, a patient who is undergoing a low risk percutaneous intervention may be sufficiently cleared by a history that is negative for chest pain and shortness of breath while those who will require general anesthesia at minimum will require a 12-lead electrocardiogram prior to surgery. In addition, patients who are undergoing high risk surgeries, including open aortic repair and lower extremity bypass, and any patient with significant cardiac disease, including unstable angina, known arrhythmias, severe valvular disease, or decompensated heart failure should be evaluated by a cardiologist prior to any major vascular procedure (Figure 1.1). It is also recommended that patients with evidence of myocardial infarction, unstable angina, or stable angina involving the left main coronary artery or three vessel disease undergo coronary revascularization prior to any major elective endovascular intervention.2 When patients who have reconstructible coronary disease who need more urgent (within 12 months) intervention, existing coronary artery disease should be treated with balloon angioplasty or bare metal stent placement followed by dual antiplatelet therapy for 4 to 6 weeks. If patients are unable to wait 4–6 weeks, then it is possible to undergo intervention at 30 days post stenting. Beta-blockade, when medically mandated, should be initiated well before surgery and should be continued in the perioperative period.
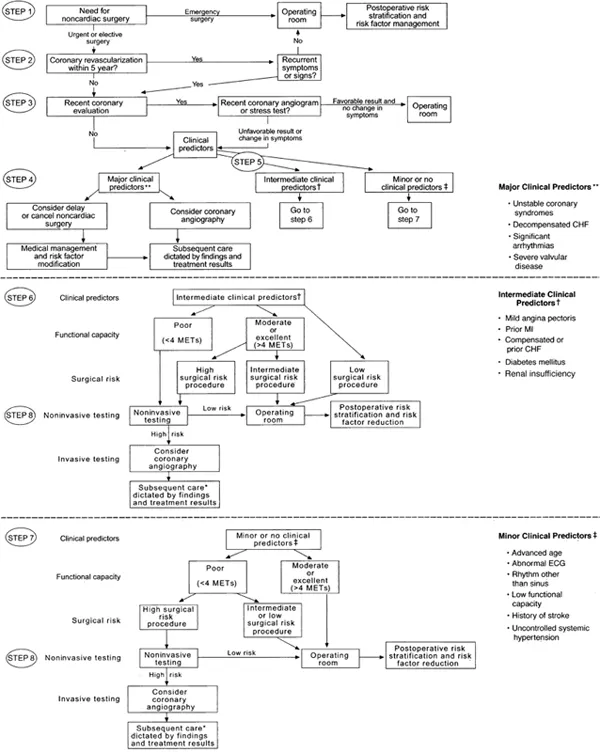
Figure 1.1 Approach to preoperative cardiac assessment. (Eagle, KA et. al. “ACC/AHA Guideline Update for Perioperative Cardiovascular Evaluation for Noncardiac Surgery – Executive Summary” Journal of the American College of Cardiology. 2002; 39(30):542–53.)
PULMONARY COMORBIDITIES
Pulmonary complications are common after major vascular procedures, especially those involving a thoracic or thoracoabdominal incision. Active smokers are counseled to stop smoking for at least 2 weeks prior to moderate and high-risk procedures to decrease the risk of pulmonary complications. However, the risk continues to decrease with longer abstinence from tobacco use. Indeed, patients are at highest risk for complications within the first 2 months of quitting smoking and their risk becomes similar to a non-smoker after 6 months. For patients with long standing tobacco use, chronic obstructive pulmonary disease (COPD), or poor baseline respiratory function (unable to walk 1 flight of stairs), preoperative pulmonary function tests are recommended in addition to obtaining a baseline arterial blood gas. These patients should also be started on pulmonary bronchodilators for at least 2 weeks prior to intervention.2
CHRONIC RENAL INSUFFICIENCY
Non-dialysis dependent patients with chronic renal insufficiency should receive adequate preoperative hydration. For patients at risk of contrast-induced nephropathy, we recommend pre-hydration with normal saline or 5% dextrose/sodium bicarbonate. For patients with an estimated glomerular filtration rate (eGFR) of < 60 mL/min, withholding metformin is recommended at the time of contrast administration. In addition, for those with an eGFR of < 45 mL/min, metformin should be held for at least 48 hours prior to contrast administration. Euglycemia can be maintained with an insulin sliding scale in the peri-procedure period. Ideally a patient's glycemic control should be optimized prior to admission to the hospital to decrease the risk of perioperative glycemic crisis as well as the risk of wound complications.
MAINTENANCE MEDICATIONS
As with most other surgical procedures, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers should be held during the perioperative period. If patients are already on beta-blocker therapy, it is recommended they continue therapy throughout the perioperative period. Initiating beta-blocker therapy immediately before intervention should be avoided until it is determined that the patient is tolerant of therapy. Initiating beta-blocker medications for the sole purpose of reducing aneurysm expansion or rupture is not recommended.2 Moreover, there is little evidence to support the use of statins to reduce aneurysm expansion or risk of rupture in the surveillance period, and thus considerations for use should be strictly for cardiac benefit.2 Despite evidence of decreased rates of aneurysm expansion in mouse models with the use of ACE inhibitors and angiotensin receptor blockers, this has not been replicated in human populations, and thus empiric administration during the surveillance period is not recommended.2 Randomized controlled trials have shown there is no effect on aneurysmal expansion with the use of empiric azithromycin and doxycycline, and thus such treatment is currently not recommended.2 In summary, patients should be maintained on their maintenance therapies for management of comorbid conditions during surveillance periods. Standard preoperative guidelines should be followed in stopping medications (e.g., ACEi/ARBs), and there are currently n...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Contents
- Preface
- Contributors
- 1 Preoperative risk assessment
- 2 Systemic complications following vascular reconstruction
- 3 Complications of stenting for occlusive disease of aortic arch branches
- 4 Complications of endovascular therapy for aneurysmal disease of splanchnic arteries including renal arteries
- 5 Complications of endovascular therapy for occlusive disease of splanchnic arteries including renal arteries
- 6 Complications of endovascular management of aortoiliac occlusive disease
- 7 Complications of percutaneous intervention for femoral, popliteal, and infrapopliteal artery occlusive disease
- 8 Complications of endovascular repair of infrarenal abdominal aortic aneurysms
- 9 Complications of endovascular repair of juxtarenal aortic aneurysms
- 10 Complications of endovascular repair of thoracic aortic aneurysms/dissections
- 11 Complications of stent grafts for popliteal aneurysms
- 12 Complications of inferior vena cava filters
- 13 Complications of carotid endarterectomy
- 14 Complications of extracranial carotid aneurysm repair and resection of carotid body tumor
- 15 Complications of open reconstruction for aneurysmal and occlusive diseases of aortic arch vessels
- 16 Complications of upper extremity bypass grafting for occlusive and aneurysmal disease
- 17 Complications of open repair of unruptured abdominal aortic aneurysm
- 18 Complications following isolated common iliac artery and hypogastric artery aneurysm repair
- 19 Complications of open repair of ruptured abdominal aortic aneurysm
- 20 Complications of open thoracoabdominal aortic aneurysm repair
- 21 Complications of open repair of juxtarenal aortic aneurysm
- 22 Complications of open repair of splanchnic aneurysms
- 23 Complications of open repair of renal artery aneurysms
- 24 Complications of open repair of femoral and popliteal aneurysms
- 25 Complications of endovascular management of aortoiliac occlusive disease
- 26 Complications of axillofemoral, femoral-femoral, and iliac-femoral grafts: Diagnosis, prevention, and management
- 27 Complications of femoropopliteal and infrapopliteal arterial bypass
- 28 Complications of surgery for thoracic outlet syndrome
- 29 Complications of hemodialysis access
- 30 Open central and peripheral venous reconstruction: Complications and strategies for managing these complications
- 31 Complications of iliofemoral venous recanalization and stent placement
- 32 Complications of endovenous ablation of varicose veins
- 33 Complications of cervical, thoracic, and abdominal interventions for trauma
- 34 Management of vascular complications during nonvascular operations
- 35 Endovascular removal of foreign bodies (catheter wires and sheaths) from the vascular system
- 36 Tissue coverage for exposed vascular reconstructions (grafts)
- Index