![]() Part I
Part I
The performance team![]()
Chapter 1
Reconditioning
A performance-based response to an injury
Bill Knowles
Introduction
For the past 25 years, I have been working with professional, world-class and Olympic-level athletes in the field of Sports Reconditioning and Performance Training. This journey continues to explore the relationship between evidence-based medicine and experience-based evidence. Even today, there continues to be a blend of the “art” and the “science” when working with athletes.
The purpose of this chapter is to explore the cornerstones of a performance rehabilitation model by considering the definitions and concepts we must consider when preparing our athletes for a return to the highest level of function following injury.
Definitions
Throughout my career I have seen many medically led rehabilitation protocols designed for elite athletes striving to return to the highest level of competition. We do need to understand, however, that there is a big difference between protecting and restoring tissue health and preparing the athlete for a return to competition.
If you are not qualified or experienced enough to design a performance training program for a professional or world-class athlete pre-injury, how are you able to design a performance training program or Return to Competition (RtC) strategy post-injury?
Rehabilitation is a medical or clinical model for treating individuals who may or may not be athletes. Often, a surgeon will design and/or direct this protocol. With operations, the focus of the protocol is on the surgery, wound healing and early stages of rehabilitation. They usually emphasize protecting the peripheral lesion first, and then promote slow controlled motion and activities of daily living. This continues for many months with the aim on “doing no harm” to the repair. Eventually, basic athletic preparation is typically encouraged to begin once biological healing time of the graft has advanced.
Just because biological healing has occurred, it does not mean the athlete is prepared for performance.
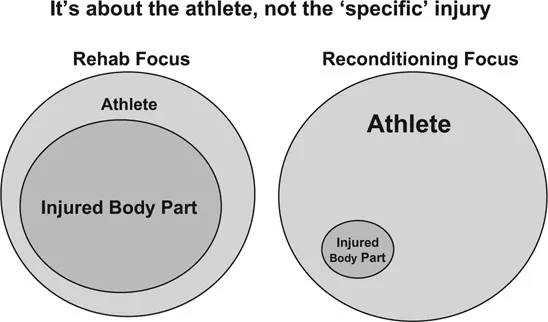
Figure 1.1 Reconditioning – Performance-based and medically supported
Reconditioning is a performance-based model for training athletes following injury or surgery. It is directed by the performance team and is medically supported. The program design begins with the end goal in mind, which is a Return to Competition. We then design a progression backward to the surgery/injury date. This process allows the performance team to address all aspects of athletic development immediately post-injury or surgery to best prepare the individual for the true demands of competition that lay ahead.
Returning to competition is easy; continuing to compete is more difficult.
Training around the injury
Reconditioning follows a functional path immediately post-injury and continues this progression until the athlete has returned to competition. We recognize that a serious injury should be looked upon as a neurophysiologic dysfunction, not just a common peripheral musculoskeletal injury. It is a peripheral injury, but with a central consequence. With this in mind we must train the brain through movements, not just muscles, during all stages of post-injury care. Most protocols that restrict active motion, like brace joints, assist motion via continuous passive motion (CPM) machines or prevent loading are affecting the normal patterning that an athlete needs in order to best prepare for higher quality training in the weeks and months to come. For joint injuries, the best brace is neuromuscular control and coordinated movement patterns. These can be developed early and often if the protocol encourages doing so.
Figure 1.2 Training around the injury
Often, rehabilitation protocols are centred on what an athlete cannot do, as opposed to what an athlete can do. While this is often a consequence of protecting the repair/injury, these limitations can compromise the short- and long-term movement qualities of the athlete. Unfortunately, rest is often the chosen form of protection, yet the short- and long-term neuromuscular inhibition that accompanies this approach may actually put the repair at greater risk as the athlete progresses.
The reconditioning model also respects protecting the repair and maintaining joint homeostasis but encourages more athletic ways to train the individual. Because reconditioning is performance-based, we prepare the athlete – we don’t just treat the injury. This is done through coaching movements that occur in daily training for the athlete, albeit at the correct intensity and load. This strategy maintains and/or restores coordinated movement patterns that are essential for athletic success in the future. Whether the response is physiological, psychological or both, the outcomes are excellent. The traditional medical model of rehabilitation, which focuses more on the injury, underestimates the total body healing response that training familiar movements has on athletes.
The load compromised athlete
When an athlete injures a joint surface, ligament, muscle or tendon it is, to some degree, forever compromised. With increased severity comes an increased challenge to keep the tissue healthy over an athlete’s career. There is clear evidence that an anterior cruciate ligament (ACL) injury leads to early onset osteoarthritis (OA) 5–15 years after injury, ‘aging’ the knee roughly 30 years.1 These degenerative changes can often exact a toll later in an athlete’s career. For knee injuries, these changes are attributed in part to quadriceps weakness as a result of arthrogenic muscle inhibition (AMI). AMI is an ongoing neural inhibition that prevents the quadriceps from fully activating and is believed to result from pain, swelling, inflammation, joint laxity and structural damage. Altered afferent information from the damaged knee joint is believed to have both spinal and supraspinal pathways.2 This ‘central consequence’ may alter dynamic neuromuscular activation patterns that affect lower extremity kinematics and kinetics leading to a negative change in load distribution across the knee joint.1
Arthrogenic muscle inhibition occurs bilaterally after unilateral knee injury.1
For example a grade III medial collateral ligament injury can permanently retain laxity in the absence of pain, swelling or decreased performance. Yet this new ‘biomechanical set-up’ (altered kinetics) with laxity on one side of a joint is not normal and may predispose the athlete to other concerns down the line; especially in high-intensity multidirectional sports. These bilateral concerns are OA, meniscal tears, ACL injury and poor power output via AMI.
Whilst research into AMI has traditionally been centred on the sequelae from knee injuries, there is increasing interest in similar neuromuscular ‘depowering’ following muscle injuries. Such acute neural responses can reduce muscle strength and endurance and alter agonist/antagonist activity and coordination in both static and dynamic motor tasks.3
Being ‘load compromised’ means questioning whether the musculoskeletal injury and the neurophysiological function of the athlete can successfully sustain the mechanical loads of high-intensity training and competing over time. In the reconditioning model, once an LCA (load compromised athlete), forever an LCA. Regardless of whether the tissue is considered biologically ‘healed’ and functionally restored, accepting the athlete’s LCA status should be a catalyst for designing the best Return to Competition and injury prevention program possible. In high-performance sport, the reality is it is often easier to get an athlete back to competition than it is to sustain them at this level. With this in mind, developing an athlete sustainability program (ASP) is a critical part of reconditioning because it is a performance-based model. On the contrary, most rehabilitation protocols dedicate very little time in this area, as they are more interested in restoring general function often at the neglect of true high-performance training.
Given that significant levels of AMI may still be present 18–33 months following knee joint injuries,2 the central tenet of an ASP is that an athlete’s reconditioning must continue well after they return to competition. The reality is, after long-term injuries, we must continue to implement strength, power and coordination training throughout the season, the year and their career. In addition, LCAs cannot take more than two weeks off from strength training or they risk a neuromuscular ‘switching-off’ that can predispose them to re-injury.
Athletic development
As a performance-based model, reconditioning is identified more closely with the field of Athletic Development than Sports Therapy. As an Athletic Development professional, I am a part of a performance team whose goal is to train all components of athleticism to the level required by the sport in which the athlete participates. The performance team is comprised of the team physician, therapists, athletic development coaches, nutritionists, sport scientists, performance psychologists and technical sport coaches.
In reconditioning, we need to appreciate that our job is to enhance athleticism, which is the ability to perform athletic movements at optimal speed with precision, and efficiency.4 This means that reconditioning follows that same functional path immediately post injury or following surgery until the athlete returns to competition. It is a path that explores what an athlete can do as they begin their preparation for more advanced training. In order to prepare for quality movements with precision and style, all treatment decisions following injury greatly matter. If you brace a knee, for example, for 12 weeks following surgery, you can expect a conflict with achieving optimal speed with grace when it matters most. This happens due to the altered mechanics that a brace inflicts on the athlete. But if you were to progressively re-establish neuromuscular control to stabilise the knee (utilizing the body’s own intrinsic ‘bracing’) with properly loaded sport-specific movement patterns, you may actually improve the quality of speed in competition.
Following the progressive path that reconditioning advocates requires knowledge and experience to understand the movements that transfer to s...