
eBook - ePub
Gynaecology by Ten Teachers
Louise C Kenny, Helen Bickerstaff, Louise Kenny, Helen Bickerstaff
This is a test
Share book
- 254 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Gynaecology by Ten Teachers
Louise C Kenny, Helen Bickerstaff, Louise Kenny, Helen Bickerstaff
Book details
Book preview
Table of contents
Citations
About This Book
First published in 1919 as 'Diseases of Women', Gynaecology by Ten Teachers is well established as a concise, yet comprehensive, guide. The twentieth edition has been thoroughly updated by a new team of 'teachers', integrating clinical material with the latest scientific developments that underpin patient care. Each chapter is highly structured, with learning objectives, definitions, aetiology, clinical features, investigations, treatments, case histories and key point summaries and additional reading where appropriate. New themes for this edition include 'professionalism' and 'global health' and information specific to both areas is threaded throughout the text.
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Gynaecology by Ten Teachers an online PDF/ePUB?
Yes, you can access Gynaecology by Ten Teachers by Louise C Kenny, Helen Bickerstaff, Louise Kenny, Helen Bickerstaff in PDF and/or ePUB format, as well as other popular books in Medicine & Perinatology & Neonatology. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
The development and anatomy of the female sexual organs and pelvis

Sexual differentiation of the fetus and development of sexual organs
Female anatomy
Structural problems of pelvic organs
Further reading
Self assessment
- Understand that sexual differentiation and development begin in early embryonic life.
- Understand the embryonic development and the anatomy of the perineum, the vagina, cervix and uterus, the adnexa and ovary and the bladder and ureters.
- Describe the blood supply and lymphatics of the perineum and pelvis.
- Understand the innervation of the perineum and pelvis.
- Understand the vulnerability of certain structures in gynaecological surgery.
- Describe the structural anomalies resulting from Müllerian tract disorders.
Sexual differentiation of the fetus and development of sexual organs
The gonadal rudiments appear as the ‘genital ridge’ overlying the embryonic kidney in the intermediate mesoderm during the fourth week of embryonic life, and they remain sexually indifferent until the seventh (Figure 1.1). The undifferentiated gonad has the potential to become either a testis or an ovary, and hence is termed bipotential, and the chromosomal complement of the zygote determines whether the gonad becomes a testis or an ovary. The development of either the testis or ovary is an active gene-directed process. In the male the activity of the SRY gene (sex-determining region of the Y chromosome) causes the gonad to begin development into a testis. In the past, ovarian development was considered a ‘default’ development due solely to the absence of SRY, but in the last 10 years ovarian-determining genes have also been found that actively lead to the development of a female gonad.
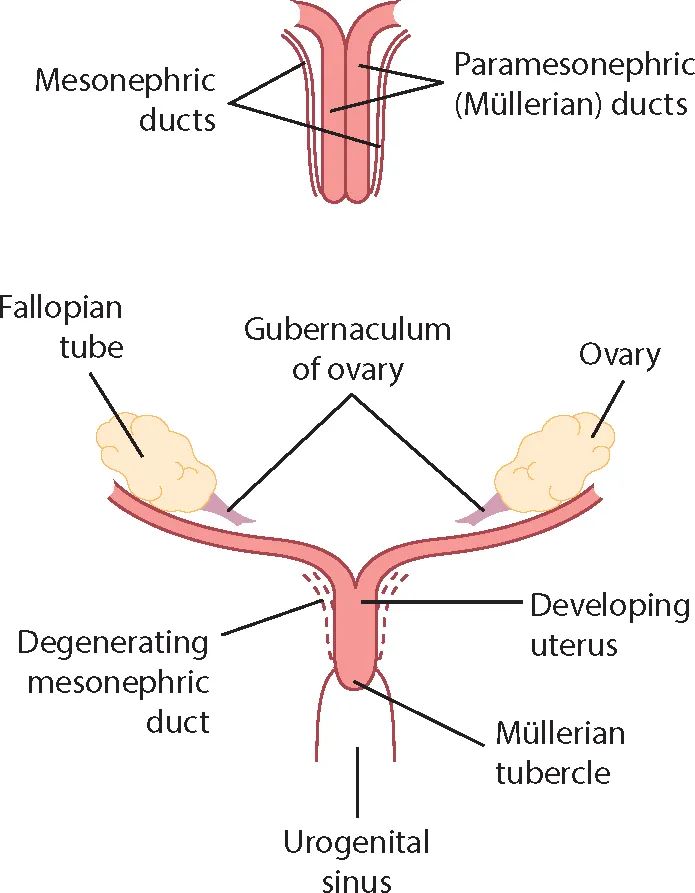
The fetus has two sets of structures called the Müllerian (or paramesonephric) ducts and Wolffian (or mesonephric) ducts, which have the potential to develop into male or female internal and external genitalia respectively.
Development of the male sexual organs
As the gonad develops into a testis, it differentiates into two cell types. The Sertoli cells produce anti-Müllerian hormone (AMH) and the Leydig cells produce testosterone. AMH suppresses further development of the Müllerian ducts whereas testosterone stimulates the Wolffian ducts to develop into the vas deferens, epididymis and seminal vesicles. In addition, in the external genital skin, testosterone is converted by the enzyme 5-alpha-reductase into dihydrotestosterone (DHT). This acts to virilize the external genitalia. The genital tubercle becomes the penis and the labioscrotal folds fuse to form the scrotum. The urogenital folds fuse along the ventral surface of the penis and enclose the urethra so that it opens at the tip of the penis.

Development of the female sexual organs
In the primitive ovary granulosa cells, derived from the proliferating coelomic epithelium, surround the germ cells and form primordial follicles. Each primordial follicle consists of an oocyte within a single layer of granulosa cells. Theca cells develop from the proliferating coelomic epithelium and are separated from the granulosa cells by a basal lamina. The maximum number of primordial follicles is reached at 20 weeks’ gestation when there are six to seven million primordial follicles present. The numbers of these reduce by atresia and at birth only 1–2 million remain. Atresia continues throughout life and by menarche only 300,000–400,000 are present, and by menopause none.
The development of an oocyte within a primordial follicle is arrested at the prophase of its first meiotic division. It remains in that state until it undergoes atresia or enters the meiotic process preceding ovulation.
In the female, the absence of testicular AMH allows the Müllerian structures to develop and the female reproductive tract develops from these paired ducts. The proximal two-thirds of the vagina develop from the paired Müllerian ducts, which grow in a caudal and medial direction and fuse in the midline. The midline fusion of these structures produces the uterus, cervix and upper vagina, and the unfused caudal segments form the Fallopian tubes, as shown in Figure 1.2.
Cells proliferate from the upper portion of the urogenital sinus to form structures called the ‘sinovaginal bulbs’. The caudal extension of the Müllerian ducts projects into the posterior wall of the urogenital sinus as the Müllerian tubercle. The Müllerian tubercles and the urogenital sinus fuse to form the vaginal plate, which extends from the Müllerian ducts to the urogenital sinus. This plate begins to canalize, starting at the hymen and proceeding upwards to the cervix in the sixth embryonic month.
External female genitalia
The external genitalia do not virilize in the absence of testosterone. Between the fifth and seventh weeks of life, the cloacal folds, which are a pair of swellings adjacent to the cloacal membrane, fuse anteriorly to become the genital tubercle. This will become the clitoris. The perineum develops and divides the cloacal membrane into an anterior urogenital membrane and a posterior anal membrane. The cloacal folds anteriorly are called the urethral folds, which form the labia minora. Another pair of folds within the cloacal membrane form the labioscrotal folds that eventually become the labia majora. The urogenital sinus becomes the vestibule of the vagina. The external genitalia are recognizably female by the end of the twelfth embryonic week.

- The primitive gonad is first evident at 5 weeks of embryonic life and forms on the medial aspect of the mesonephric ridge.
- The undifferentiated gonad has the potential to become either a testis or an ovary.
- The paramesonephric duct, which later forms the Müllerian system, is the precursor of female genital development.
- The lower end of the Müllerian ducts fuse in the midline to form the uterus and upper vagina.
- Most of the upper vagina is of Müllerian origin, while the lower vagina forms from the sinovaginal bulbs.
- Primordial follicles contain an oocyte arrested in prophase surrounded by granulosa cells separated by a basement membrane from Leydig cells.
- The maximum number of primordial follicles is reached at 20 weeks’ gestation. These reduce by atresia throughout childhood and adult life.
Female anatomy
External genitalia
The external genitalia are commonly called the vulva and include the mons pubis, labia majora and minora, the vaginal vestibule, the clitoris and the greater vestibular glands. The mons pubis is a fibro-fatty pad covered by hair-bearing skin that covers the bony pubic ramus.
The labia majora are two folds of skin with underlying adipose tissue lying either side of the vaginal opening. They contain sebaceous and sweat glands and a few specialized apocrine glands. In the deepest part of each labium is a core of fatty tissue continuous with that of the inguinal canal and the fibres of the round ligament, which terminate here.
The labia minora are two thin folds of skin that lie between the labia majora. These vary in size and may protrude beyond the labia major where they are visible, but may also be concealed by the labia majora. Anteriorly, they divide in two to form the prepuce and frenulum of the clitoris (clitoral hood). Posteriorly, they divide to form a fold of skin called the fourchette at the back of the vagina introitus. They contain sebaceous glands, but have no adipose tissue. They are not well developed before puberty and atrophy after the menopause. Both the labia minora and labia majora become engorged during sexual arousal.
The clitoris is an erectile structure measuring approximately 0.5–3.5 cm in length. The body of the clitoris is the main part of the visible clitoris and is made up of paired columns of erectile tissue and vascular tissue called the ‘corpora cavernosa’. These become the crura at the bottom of the clitoris and run deeper and laterally. The vestibule is the cleft between the labia minora. It contains openings of the urethra, the Bartholin’s glands and the vagina. The vagina is surrounded by two bulbs of erectile and vascular tissue that are extensive and almost completely cover the distal vaginal wall. These have traditionally been named the bulb of the vaginal vestibule, although recent work on both dissection and magnetic resonance imaging (MRI) suggests that they may be part of the clitoris and should be renamed ‘clitoral bulbs’. Their function is unknown but they probably add support to the distal vaginal wall to enhance its rigidity during penetration.
The Bartholin’s glands are bilateral and about the size of a pea. They open via a 2 cm duct into the vestibule below the hymen and contribute to lubrication during intercourse.
The hymen is a thin covering of mucous membrane across the entrance to the vagina. It is usually perforated, which allows menstruation. The hymen is ruptured during intercourse and any remaining tags are called ‘carunculae myrtiformes’.
Internal reproductive organs (Figure 1.3)
The vagina
The vagina is a fibromuscular canal lined with stratified squamous epithelium that leads from the uterus to the vulva. It is longer in the posterior wall (approximately 9 cm) than in the anterior wall (approximately 7 cm). The vaginal walls are normally in apposition, except at the vault where they are separated by the cervix. The vault of the vagina is divided into four fornices: posterior, anterior and two lateral.
The midvagina is a transverse slit while the lower vagina is an H-shape in transverse section. The vaginal walls are lined with transverse folds. The vagina has no glands and is kept moist by secretions from the uterine and cervical glands and by transudation from its epithelial lining. The epithelium is thick and rich in glycogen, which increases in the postovulatory phase of the cycle. However, before puberty and after the menopause, the vagina is devoid of glycogen due to the lack of oestrogen. Doderlein’s bacillus is a normal commensal of the vaginal flora and br...