eBook - ePub
Pediatric ESAP 2021-2022 Pediatric Endocrine Self-Assessment Program Questions, Answers, Discussions
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Pediatric ESAP 2021-2022 Pediatric Endocrine Self-Assessment Program Questions, Answers, Discussions
About this book
Pediatric Endocrine Self-Assessment Program (Pediatric ESAP), Reference Edition, 2021-2022 is a self-study curriculum specifically designed for endocrinologists seeking initial certification or recertification in pediatric endocrinology, program directors interested in a training instrument, and clinicians and health professionals seeking a self-assessment and a broad review of pediatric endocrinology. Pediatric ESAP consists of 100 multiple-choice questions in all areas of pediatric endocrinology, diabetes, growth, and metabolism. There is extensive discussion of each correct answer and references. Pediatric ESAP is updated every two years with new questions.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Pediatric ESAP 2021-2022 Pediatric Endocrine Self-Assessment Program Questions, Answers, Discussions by Liuska M Pesce,Paola A Palma Sisto, Liuska M Pesce, Paola A Palma Sisto in PDF and/or ePUB format, as well as other popular books in Medicine & Endocrinology & Metabolism. We have over one million books available in our catalogue for you to explore.
Information
QUESTIONS
PEDIATRIC ENDOCRINE SELF-ASSESSMENT PROGRAM 2021-2022
Part I
1 A 4-and-7/12-year-old boy born to Scottish parents presents to the emergency department with recurrent bouts of vomiting and diarrhea over the past year. While in the emergency department, he has a seizure and is noted to be hypoglycemic (blood glucose = 14.4 mg/dL [0.8 mmol/L]). He is given a glucose and fluid bolus and is maintained on an intravenous dextrose and saline solution.
He was born at term and was treated for neonatal jaundice. His parents describe him as being a sickly child who “catches everything,” but because he has always grown well, they have not been concerned. He has no skin problems or infections.
On physical examination, the child is hyperpigmented. His weight is at the 50th percentile, and height is greater than the 90th percentile. His midparental range is between the 25th and 50th percentile. Bone age is advanced to 8.2 years. Blood pressure is normal, and he is clinically prepubertal.
Blood tests confirm that serum cortisol is undetectable and plasma ACTH is high.
Laboratory test results:
Random serum cortisol = <1.8 µg/dL (4.3-9.4 µg/dL) (SI: <50 nmol/L [120-620 nmol/L])
Plasma ACTH = 4310 pg/mL (6-48 pg/mL) (SI: 948.2 pmol/L [1.3-10.6 pmol/L])
Sodium = 140 mEq/L (136-144 mEq/L) (SI: 140 mmol/L [136-144 mmol/L])
Potassium = 4.8 mEq/L (3.2-5.2 mEq/L) (SI: 4.8 mmol/L [3.2-5.2 mmol/L])
Plasma renin activity = 3.5 ng/mL per h (0.6-3.8 ng/mL per h)
Aldosterone = 6.7 ng/dL (3.6-16.2 ng/dL) (SI: 185 pmol/L [100-450 pmol/L])
17-Hydroxyprogesterone = 33.0 ng/dL (<92.4 nmol/L) (SI: 1.0 nmol/L [<2.8 nmol/L])
Androstenedione = <10.0 ng/dL (10.0-16.9 ng/dL) (SI: <0.35 nmol/L [0.35-0.59 nmol/L])
Calcium = 9.2 mg/dL (8.4-10.0 mg/dL) (SI: 2.3 mmol/L [2.1-2.5 mmol/L])
TSH = 4.0 mIU/L (0.5-4.8 mIU/L)
Free T4 = 1.1 ng/dL (0.9-1.6 ng/dL) (SI: 13.8 pmol/L [12.0-20.6 pmol/L])
Adrenal antibodies, negative
Very long-chain fatty acids, normal
Which of the following is the most likely diagnosis?
A. Addison disease
B. Familial glucocorticoid deficiency
C. Congenital adrenal hypoplasia
D. Congenital adrenal hyperplasia
E. X-linked adrenoleukodystrophy
2 A 2-year-old boy presents to the emergency department with left eye esotropia 1 week after a fall from standing height. MRI shows dilated optic nerve sheaths bilaterally, optic nerve tortuosity, and mild flattening of the posterior globes consistent with clinical papilledema. He has an unusual head shape. A 3-dimensional reconstruction CT shows complete fusion of the sagittal suture with associated dolichocephaly.
On physical examination, he has short stature (height <5th percentile), mild genu varum deformity, and a waddling gait. His hands and feet are normal. He has no dental abnormalities. His medical history is otherwise unremarkable. He was breastfed without vitamin D supplementation until 1 year of life. He started walking at age 15 months, and his parents have noticed the waddling gait since that time. X-rays are consistent with rachitic changes at the knees.
These physical examination characteristics are most concerning for which of the following underlying skeletal disorders?
A. X-linked hypophosphatemic rickets
B. Hypophosphatasia
C. Hypochondroplasia
D. Severe vitamin D deficiency
E. Apert syndrome
3 A 13-year-old girl with type 1 diabetes mellitus treated with multiple daily insulin injections uses a continuous glucose monitor efficiently for her daily glycemic management. She plans to eat dry cereal for her afternoon snack when she comes home from school. The food label for this cereal is displayed (see image). She carefully measures 2 servings of one-third cup (total two-thirds cup) in a bowl. Her continuous glucose monitor reads 92 mg/dL (5.1 mmol/L) with a flat arrow. Her insulin-to-carbohydrate ratio in the afternoon is 1:6 (1 unit for every 6 g carbohydrate).
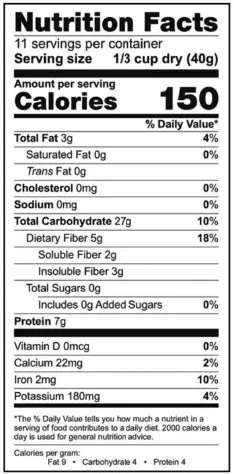
How many units (rounded to the nearest whole unit) of rapid-acting insulin she should inject before consuming this snack?
A. 10 units
B. 9 units
C. 8 units
D. 7 units
E. She should eat her snack and monitor her glucose via continuous glucose monitoring to decide
4 A 12-year-old girl with primary hypothyroidism secondary to chronic lymphocytic thyroiditis (negative thyroglobulin antibodies) is seen for evaluation of thyroid nodules. Neck ultrasonography documents a solid right nodule measuring 1.8 × 1 × 1 cm and a less well-defined, smaller nodule on the left lobe measuring 1.2 × 0.8 × 0.8 cm (see images).
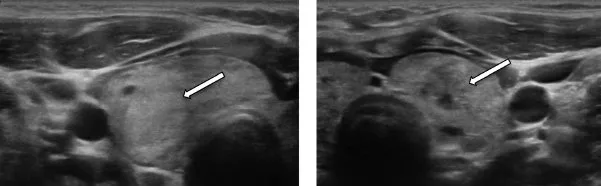
Ultrasound-guided FNA reveals a benign nodule on the right lobe and atypia of unclear significance in the left lobe. Options for treatment are discussed, and the family decides to proceed with total thyroidectomy. Pathologic examination documents a right follicular adenoma and a 0.9-cm left lobe papillary thyroid carcinoma, classic type, confined to the thyroid without lymphovascular invasion. Lymph nodes are negative for tumor (3 on the left, 4 on the right, and 13 in the left central neck). Staging is assigned as pT1a pN0 (where p stands for pathological examination of surgical specimen, T1a refers to tumor ≤1 cm limited to the thyroid, and N0 refers to nonregional lymph node metastasis).
Two weeks after surgery, the family comes for a follow-up visit to discuss further management.
Which of the following is the best management plan?
A. Perform 123I scan and measure stimulated thyroglobulin following levothyroxine withdrawal and low-iodine diet
B. Optimize levothyroxine treatment to maintain TSH between 0.5 and 1.0 mIU/L and follow-up with thyroglobulin measurement (while on levothyroxine) 12 weeks after surgery
C. Treat with 131I following levothyroxine withdrawal and low-iodine diet and perform posttreatment scan 4 to 7 days after treatment
D. Optimize levothyroxine treatment to maintain TSH between 0.1 and 0.5 mIU/L and measure thyroglobulin (while on levothyroxine) 6 weeks after surgery
E. Optimize levothyroxine to maintain TSH between 0.5 and 4.5 mIU/L and measure thyroglobulin (while on levothyroxine) 12 weeks after surgery
5 A 5-week-old male newborn is referred by his pediatrician for evaluation of gynecomastia. He was born at 40 weeks’ gestation, birth weight was 7 lb 12 oz (3520 g), and there were no complications during pregnancy or delivery. His parents report that they first noticed breast tissue at about 1 week of age. The tissue has been increasing in size and getting firmer, and they have noticed milky discharge on 2 occasions. His diet is primarily breast milk with some formula supplementation. His parents state that he has had no known contact with hormone preparations, and they use a standard baby wash for baths.
On physical examination, his length is at the 60th percentile and weight is at the 90th percentile. He appears well, and examination findings are normal except for very firm, mobile breast tissue bilaterally, measuring 7 to 8 cm. There are no midline defects, and there is no discharge from the nipples.
Laboratory test results:
β-hCG = <1 mIU/mL (0-3 mIU/mL) (SI: <1 IU/L [0-3 IU/L])
TSH = 6.38 mIU/L (0.72-11.00 mIU/L)
Free T4 = 1.46 ng/dL (0.48-2.34 ng/dL) (SI: 18.8 pmol/L [6.2-30.1 pmol/L])
Prolactin = 108.5 ng/mL (≤10 ng/mL) (SI: 4.7 nmol/L [≤0.4 nmol/L])
Karyotype = 46,XY
Which of the following is the best next step in this patient’s management?
A. Perform MRI of the brain and pituitary gland
B. Measure LH, FSH, and testosterone
C. Measure prolactin again in 2 to 4 weeks
D. Start dopamine agonist therapy
E. Order genetic testing of the MEN1 gene
6 A 17-year-old girl is followed in endocrinology clinic for thyroid hormone and GH replacement. Medulloblastoma was diagnosed at age 9 years. She had total tumor resection and received craniospinal radiation therapy (2340 cGy to the craniospinal axis plus a boost of 1260 cGy to the posterior fossa and 1980 cGy to the tumor bed) followed by 8 months of chemotherapy with cisplatin, cyclophosphamide, and lomustine. At her initial endocrine visit at age 11 years, her parents reported that she had not changed shoe size in 2 to 3 years. Subsequently, TSH and GH deficiencies were diagnosed, and she was prescribed appropriate replacement therapy. Her linear growth improved. At age 13 years, primary ovarian insufficiency was diagnosed, and hormone replacement therapy was initiated. GH therapy was stopped at age 16 years when she underwent menarche. At that time, her growth velocity was less than 2 cm/y. An IGF-1 measurement 2 months after stopping GH therapy was normal. She continues to take levothyroxine and an oral contraceptive pill with very good adherence.
Laboratory tes...
Table of contents
- Cover
- Copyright
- Pediatric Endocrine Self-Assessment Program 2021-2022: Part I
- Pediatric Endocrine Self-Assessment Program 2021-2022: Part II
- Pediatric Endocrine Self-Assessment Program 2021-2022: Part III