![]()
Chapter 1
Introduction
1.1. Overview
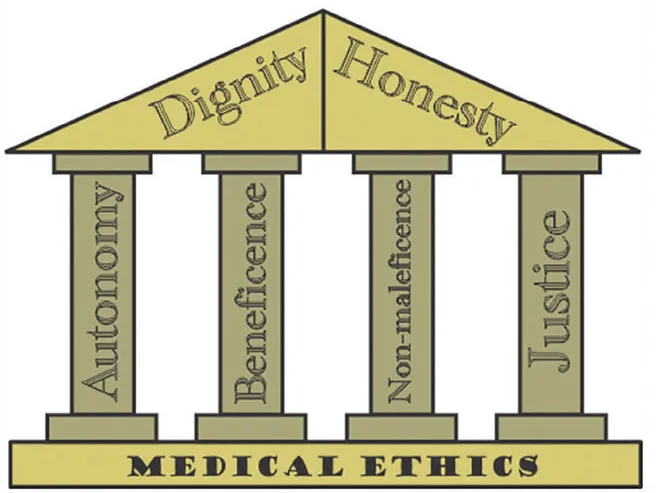
Ethics and moralities are at the core of human civilizations. Morals are the individual principles or one’s conscience, while ethics are the rules and regulations provided by external sources. Ethical practices in the medical profession are of utmost importance. In fact, this profession needs to be more ethical than any other profession as it is directly related to the patients’ health and their lives. Ethical issues are directly associated with life and death. The ethical practices of the medical profession are also known as “clinical ethics,” and their goal is to improve the quality of patient care. It is the ethical obligation in medical practices to be competent and to have respect for the patients and their health decisions and maintaining the primacy of the patient’s need even under political, economic, and social pressure (Nandi 2000). Trust and respect are two essential principles needed to maintain a good relationship between the doctor and the patient. It is the ethical obligation of medical practitioners to recognize their responsibilities toward the patients and society. According to the principles of medical ethics, the doctor should be dedicated to delivering excellent medical service. In the context of the medical ethics, Beauchamp and Childress (2001) have presented four fundamental principles of medical ethics: (1) respect for autonomy, (2) beneficence, (3) nonmaleficence, and (4) justice. In respect to autonomy, the medical practitioner is expected to respect the right of the patient to accept or refuse any treatment. Beneficence refers to the doctor’s duty to act in the best interest of the patient. Nonmaleficence means to not harm the patient, while justice refers to the equal and fair treatment of every patient regardless of his/her social, economic, and political status. These four principles of medical ethics are the pillars of medical ethics on which the edifice of the medical profession rests. Apart from these four principles, Pierre (2014) adds honesty and dignity as two additional principles of medical ethics (see fig. 1).
Fig. 1. Bajaj (2014)
The doctor-patient relationship is the foundation of medical ethics. A healthy relationship between the patient and doctor has considerable healing power. That is why the doctor cannot achieve success by just using his clinical knowledge, proficiency, and the technical skills, but rather it depends upon this healthy interpersonal relationship (Raina et al. 2014).
Many times, while dealing with patients and difficult situations, the medical practitioners have to confront moral and ethical dilemmas. Sometimes, the respect for autonomy has to be compromised for the sake of beneficence. At times, the physician’s ethics can conflict with the social, economic, and cultural norms. These dilemmas often occur in major issues such as abortion, contraception, euthanasia, confidentiality, truth telling, maintaining relations with patients’ relatives, religious issues, traditional medicines, etc. Making decisions in these situations is extremely difficult as the consequences of decision-making are uncertain.
The present thesis attempts to gain a thorough understanding of ethical and moral issues in medical practices. The research has been carried out through case studies, which are based on the ethics in medicine, ethical dilemmas, and the doctor-patient relationship and its impact on ethical practices.
1.2. Research Background and Significance
The proper education related to the practice of medical ethics is an extremely important topic. But this topic has not been taken seriously in medical education, especially in the non-Western countries (Takala 2001). From some years, the topic of medical ethics has been included in medical education as a core domain. However, the application is not adequate. As a result, medical practices are likely to be affected and can sometimes lead to the medical professionals having to respond to legal suits. Hence, there is an acute need of improvement in the study and understanding of medical ethics.
A study was conducted using doctors in Canada researching ethical practices in the medical field. About 52% of the Canadian physicians revealed that they did not have any formal education on medical ethics. About 57% said that they would seek help from the ethics committee if any ethical issues arise (Beauchamp 1998). A similar study was conducted by Yousef et al. (2017) in some Asian countries. In their cross-sectional comparative survey, they attempted to assess the knowledge of the doctors regarding medical ethics. The study observed that the medical practitioners have a strong theoretical knowledge, but they lack knowledge in the actual application of ethical practices in their day-to-day performance of medical duties. In another recent study, those findings were confirmed. Medical students receive theoretical training in medical school, but the training does not address the practical ethical dilemma that is confronted by the doctors while actually practicing (AbuAbah et al. 2019). Doctors are also not aware of several ethical policies such as organ donation regulations, withholding mechanical ventilation, managing conflicts with family members, or seeking advice from the ethics committee (AbuAbah et al. 2019). This shows that the issues related to ethics are faced by the doctors all over the world. That is why the researcher of this thesis perceives it to be crucial to study the common ethical issues in the health-care industry, including the lack of adequate knowledge and the actual implementation of ethics principles.
Inadequate knowledge of medical issues and any number of other such reasons has resulted in growing unethical practices in the medical profession. This tend to likely exist because ethics may have been taught in medical colleges, but these concepts might not have been inculcated in the students. Many unethical practices have been observed by the medical students during their training. There was a survey conducted that involved participation of medical students in their first and fourth years. About 35% of first-year students and 90% of fourth-year students reported observing unethical practices (Satterwhite, Satterwhite, and Enarson 1998). In a recent study with medical students from Malaysia, it was observed that the students had very little or no knowledge about the ethical practices in their profession. In the same study, it was noticed that 75% of the participants had never heard about the Code of Professional Conduct by the Malaysian Medical Council, and 78% of the students were not aware of the Code of Ethics by the Malaysian Medical Association (Yadav et al. 2019).
Medical ethics are directly and indirectly associated with the laws of the respective countries. Doctors should be aware of such laws. The laws regarding medical ethics vary from country to country as they depend upon cultural, social, and political issues. For example, prenatal testing or testing to determine the gender of the fetus is illegal in India. Therefore, it is not an ethical practice to inform the parents of the sex of the fetus prior to its birth. But it is not unethical or illegal if this same practice is conducted in the United Kingdom (UK) or other European countries. This indicates that sometimes the perception of medical ethics is circumstantial. In some cases, the laws are likely to conflict with the ethical practices. In such cases, the physicians are required to disobey the laws that demand unethical behavior. There are several examples of issues that create a great dilemma in the medical profession. That is why there needs to be a larger focus on medical ethics and extensive studies to be undertaken in this area.
1.3. Associating Medical Profession and Ethics
Previous scholars have discussed and debated ethical practices and how they have changed over the course of time (e.g., see Evan [2016] and Saniotis [2007]). However, as mentioned above, their actual practice or implementation is yet to be improved.
Strict adherence to ethical and moral practices is the key to success in the medical profession and su...