eBook - ePub
Proton Therapy E-Book
Indications, Techniques, and Outcomes
Steven J Frank, X. Ronald Zhu
This is a test
Share book
- 272 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Proton Therapy E-Book
Indications, Techniques, and Outcomes
Steven J Frank, X. Ronald Zhu
Book details
Book preview
Table of contents
Citations
About This Book
As proton therapy treatment centers become smaller and more cost-effective, education and training for today's multi-disciplinary oncology teams are more important than ever before. This state-of-the-art reference brings you fully up to date with all aspects of proton therapy, with guidance you can trust from MD Anderson Cancer Center, the largest and most experienced proton therapy center in the world. Led by Drs. Steven J. Frank and W. Ronald Zhu, Proton Therapy provides a unique opportunity to benefit from the unsurpassed knowledge and expertise of an esteemed team of leaders in the field.
- Covers all cancers for which proton therapy is used most often, including prostate, head and neck, pediatrics, central nervous system, gastrointestinal, sarcomas, lungs, breast, lymphomas, and gynecologic cancers.
- Provides up-to-date information on radiobiology, treatment planning and quality assurance, indications for proton therapy, management approaches, and outcomes after proton therapy by disease site.
- Discusses technologic advances such as spot scanning and treatment planning systems for the management of solid tumors; radiobiology of proton therapy, including DNA damage and repair mechanisms and acute and late effects on normal tissues; and multifield optimized intensity-modulated proton therapy (MFO-IMPT) for optimizing the distribution of linear energy transfer (LET) of proton beams within target volumes and away from critical normal structures.
- Includes a special section on head and neck cases in the e-book that photographically illustrates the full cycle of proton therapy care.
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Proton Therapy E-Book an online PDF/ePUB?
Yes, you can access Proton Therapy E-Book by Steven J Frank, X. Ronald Zhu in PDF and/or ePUB format, as well as other popular books in Medicina & Oncología. We have over one million books available in our catalogue for you to explore.
SECTION III
Disease Sites
Outline
- 8. Proton radiotherapy for breast cancer
- 9. Adult central nervous system tumors
- 10. Gastrointestinal
- 11. Proton therapy for gynecologic malignancies
- 12. Proton therapy for prostate cancer
- 13. Head and neck
- 14. Proton therapy for hematologic malignancies
- 15. Pediatric considerations for proton therapy
- 16. Proton therapy and sarcomas
- 17. Esophagus cancer
- 18. Lung cancer
Chapter 8
Proton radiotherapy for breast cancer
Wendy A. Woodward, Falk Poenisch, Karen E. Hoffman
Introduction
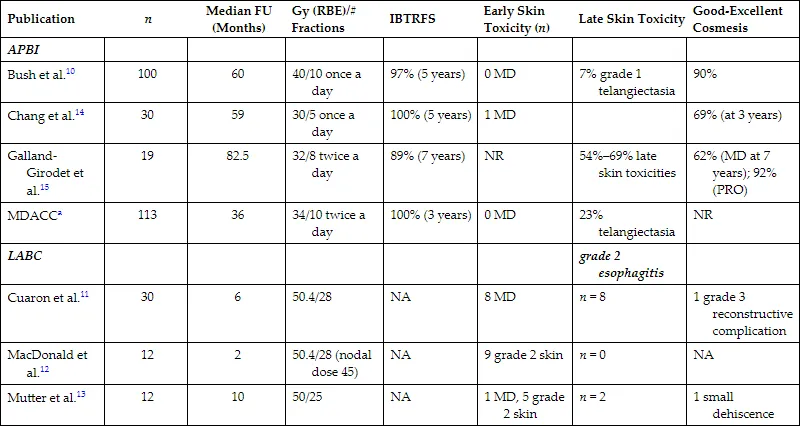
Numerous planning studies demonstrate superior dosimetry for proton radiotherapy compared with photon-based radiotherapy for breast cancers of all stages, even compared with intensity-modulated radiotherapy.1 Protons can reduce dose to the heart by a factor of two to three compared with well-designed photon-based three-dimensional conformal plans, and target coverage is improved with protons.2–9 An ongoing randomized clinical trial is comparing proton therapy to photon therapy to examine the effect on cardiac toxicity (NCT02603341). To date, however, clinical outcome data comparing protons to photons for breast cancer are limited, so translation of this dosimetric advantage remains under investigation, and access and cost may offset the obvious dosimetric gains in some cases. Reports of several hundred patients treated with protons have been published, and these highlight patient satisfaction and good early clinical outcomes in most studies10–13 but increased skin toxicity and other side effects in others.11,14–16 A broad range of dose regimens has been used, adding complexity to the analysis of the emerging data (Table 8.1). Here we briefly review the available data on dosimetric, clinical, and value related to proton therapy for breast cancer, highlight cases for whom there is an obvious benefit in the context of the existing data, and touch on planning issues to optimize outcomes. For all plan reviews, plans should be evaluated by physics before review by the radiation oncologist. Physics sign-off should confirm that the plan is robust. When multiple passive fields are used, each beam should be viewed independent of the others for complete coverage. For multiple-field-scanning beam planning, robust optimization, discussed below, should be used before physician review.
TABLE 8.1 ■
Clinical Breast Proton Data
| Publication | n | Median FU (Months) | Gy (RBE)/# Fractions | IBTRFS | Early Skin Toxicity (n) | Late Skin Toxicity | Good-Excellent Cosmesis |
|---|---|---|---|---|---|---|---|
| APBI | |||||||
| Bush et al.10 | 100 | 60 | 40/10 once a day | 97% (5 years) | 0 MD | 7% grade 1 telangiectasia | 90% |
| Chang et al.14 | 30 | 59 | 30/5 once a day | 100% (5 years) | 1 MD | 69% (at 3 years) | |
| Galland-Girodet et al.15 | 19 | 82.5 | 32/8 twice a day | 89% (7 years) | NR | 54%–69% late skin toxicities | 62% (MD at 7 years); 92% (PRO) |
| MDACCa | 113 | 36 | 34/10 twice a day | 100% (3 years) | 0 MD | 23% telangiectasia | NR |
| LABC | grade 2 esophagitis | ||||||
| Cuaron et al.11 | 30 | 6 | 50.4/28 | NA | 8 MD | n = 8 | 1 grade 3 reconstructive complication |
| MacDonald et al.12 | 12 | 2 | 50.4/28 (nodal dose 45) | NA | 9 grade 2 skin | n = 0 | NA |
| Mutter et al.13 | 12 | 10 | 50/25 | NA | 1 MD, 5 grade 2 skin | n = 2 | 1 small dehiscence |
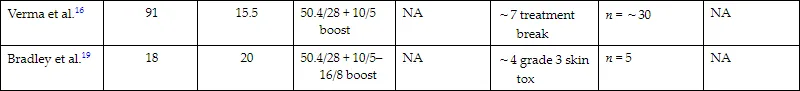
| Verma et al.16 | 91 | 15.5 | 50.4/28 + 10/5 boost | NA | ∼7 treatment break | n = ∼30 | NA |
| Bradley et al.19 | 18 | 20 | 50.4/28 + 10/5–16/8 boost | NA | ∼4 grade 3 skin tox | n = 5 | NA |
aUnpublished.
APBI, Accelerated partial breast irradiation; FU, follow-up; IBTRFS, ipsilateral breast tumor recurrence-free survival; LABC; locally advanced breast cancer; MD, moist desquamation; MDACC, MD Anderson Cancer Center; NA, not applicable; NR, not reported; PRO, patient-reported outcomes.
Complex geometry/locally advanced breast cancer
A commonly spoken misconception about radiotherapy for breast cancer is that it is easy. Some of it is. When it isn’t easy, though, breast cancer can present a vast array of unique and complex scenarios that arise from a combination of body habitus, disease factors, and surgical or systemic therapy choices that make tried-and-true breast radiation techniques suboptimal. Regional nodal irradiation (RNI; infraclavicular, supraclavicular, and internal mammary nodal basin coverage) is a primary driver of both lung and cardiac dose. Although these nodal basins can be treated within normal tissue constraints for many patients by using photon electron combinations, meeting the target goals and constraints can be impossible with photon- and electron-based therapy for patients where (1) depth to the internal mammary nodes is large, (2) involved nodal coverage requires significant coverage of internal mammary spaces directly anterior to the heart, or (3) a significant proportion of the overall lung volume lies in the supraclavicular field. Importantly, a meta-analysis of two randomized trials examining the benefits of RNI demonstrated increased overall survival in RNI-treated patients.17 In complex geometry cases where RNI is warranted, the radiation oncologist often must compromise on the goals, perhaps using intensity-modulated radiation therapy and accepting a higher heart and lung dose or lowering the dose to the target to achieve safe constraints. Numerous dosimetric studies demonstrate that these challenges can be overcome for patients with complex anatomy by using proton therapy.1–4,8,9,18–26 Efforts to create objective indications for patients for whom geometric challenges merit proton therapy have been published, including the work by Mailhot Vega et al. demonstrating value for all patients with one or more cardiac risk factors for whom the mean heart dose would otherwise be greater than 5 Gy.27 This recommendation is based on clear demonstration that protons can reduce left anterior descending coronary artery dose and mean heart dose.28 The ongoing randomized photon versus proton RadComp trial will determine if improvements in dosimetry from using proton therapy will improve clinical cardiac toxicity from breast radiotherapy among unselected patients receiving RNI (NCT02603341).
Postmastectomy radiation planning
Planning begins with obtaining planning computed tomography (CT) images, paying careful attention to setup and immobilization including head position.20,25,29,30 The physician draws the clinical target volume (CTV), which the physicist edits to create a scanning target volume (STV). The STV excludes 5 mm for the skin rind and includes a distal margin on the CTV calculated based on the range (∼3.5%). Reducing the distal margin can avoid overshooting into the lung because the chest wall thickness for those patients is rather small (∼5 mm), but it must be balanced with the concern that an adequate dose is delivered to the tissues immediately anterior to the chest wall, and in some cases, the chest wall itself. In most cases, photon/electron treatments of locally advanced postmastectomy targets would fully cover the chest wall in the target, and this should be considered in the patient selection and planning process.
To avoid tangential beam entrance, an en face beam is preferred, and thus often only one beam with one ideal angle is needed. This is achieved by a 30-degree beam from the anteroposterior direction, with ±10-degree variation, depending on the patient’s setup. Given the field size limit of 30 cm, in some cases, the full volume cannot be encompassed in one field, and a two-isocenter plan is used with two junctions during the course of treatment. In this case, field-specific targets may be created, and each field would have at least a 4-cm dosimetric overlap to have a smooth transition at the junction of both beams.
Robust optimization should be performed to ensure that coverage is not overly affected by variation in setup and anatomy. If a single-field plan is used, robust optimization may have little benefit.