eBook - ePub
Proton Therapy E-Book
Indications, Techniques, and Outcomes
Steven J Frank, X. Ronald Zhu
This is a test
Compartir libro
- 272 páginas
- English
- ePUB (apto para móviles)
- Disponible en iOS y Android
eBook - ePub
Proton Therapy E-Book
Indications, Techniques, and Outcomes
Steven J Frank, X. Ronald Zhu
Detalles del libro
Vista previa del libro
Índice
Citas
Información del libro
As proton therapy treatment centers become smaller and more cost-effective, education and training for today's multi-disciplinary oncology teams are more important than ever before. This state-of-the-art reference brings you fully up to date with all aspects of proton therapy, with guidance you can trust from MD Anderson Cancer Center, the largest and most experienced proton therapy center in the world. Led by Drs. Steven J. Frank and W. Ronald Zhu, Proton Therapy provides a unique opportunity to benefit from the unsurpassed knowledge and expertise of an esteemed team of leaders in the field.
- Covers all cancers for which proton therapy is used most often, including prostate, head and neck, pediatrics, central nervous system, gastrointestinal, sarcomas, lungs, breast, lymphomas, and gynecologic cancers.
- Provides up-to-date information on radiobiology, treatment planning and quality assurance, indications for proton therapy, management approaches, and outcomes after proton therapy by disease site.
- Discusses technologic advances such as spot scanning and treatment planning systems for the management of solid tumors; radiobiology of proton therapy, including DNA damage and repair mechanisms and acute and late effects on normal tissues; and multifield optimized intensity-modulated proton therapy (MFO-IMPT) for optimizing the distribution of linear energy transfer (LET) of proton beams within target volumes and away from critical normal structures.
- Includes a special section on head and neck cases in the e-book that photographically illustrates the full cycle of proton therapy care.
Preguntas frecuentes
¿Cómo cancelo mi suscripción?
¿Cómo descargo los libros?
Por el momento, todos nuestros libros ePub adaptables a dispositivos móviles se pueden descargar a través de la aplicación. La mayor parte de nuestros PDF también se puede descargar y ya estamos trabajando para que el resto también sea descargable. Obtén más información aquí.
¿En qué se diferencian los planes de precios?
Ambos planes te permiten acceder por completo a la biblioteca y a todas las funciones de Perlego. Las únicas diferencias son el precio y el período de suscripción: con el plan anual ahorrarás en torno a un 30 % en comparación con 12 meses de un plan mensual.
¿Qué es Perlego?
Somos un servicio de suscripción de libros de texto en línea que te permite acceder a toda una biblioteca en línea por menos de lo que cuesta un libro al mes. Con más de un millón de libros sobre más de 1000 categorías, ¡tenemos todo lo que necesitas! Obtén más información aquí.
¿Perlego ofrece la función de texto a voz?
Busca el símbolo de lectura en voz alta en tu próximo libro para ver si puedes escucharlo. La herramienta de lectura en voz alta lee el texto en voz alta por ti, resaltando el texto a medida que se lee. Puedes pausarla, acelerarla y ralentizarla. Obtén más información aquí.
¿Es Proton Therapy E-Book un PDF/ePUB en línea?
Sí, puedes acceder a Proton Therapy E-Book de Steven J Frank, X. Ronald Zhu en formato PDF o ePUB, así como a otros libros populares de Medicina y Oncología. Tenemos más de un millón de libros disponibles en nuestro catálogo para que explores.
SECTION III
Disease Sites
Outline
- 8. Proton radiotherapy for breast cancer
- 9. Adult central nervous system tumors
- 10. Gastrointestinal
- 11. Proton therapy for gynecologic malignancies
- 12. Proton therapy for prostate cancer
- 13. Head and neck
- 14. Proton therapy for hematologic malignancies
- 15. Pediatric considerations for proton therapy
- 16. Proton therapy and sarcomas
- 17. Esophagus cancer
- 18. Lung cancer
Chapter 8
Proton radiotherapy for breast cancer
Wendy A. Woodward, Falk Poenisch, Karen E. Hoffman
Introduction
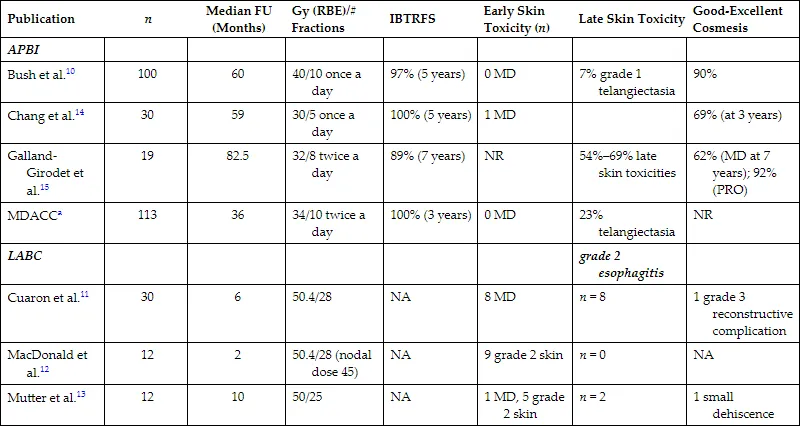
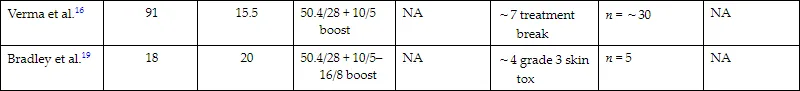
Numerous planning studies demonstrate superior dosimetry for proton radiotherapy compared with photon-based radiotherapy for breast cancers of all stages, even compared with intensity-modulated radiotherapy.1 Protons can reduce dose to the heart by a factor of two to three compared with well-designed photon-based three-dimensional conformal plans, and target coverage is improved with protons.2–9 An ongoing randomized clinical trial is comparing proton therapy to photon therapy to examine the effect on cardiac toxicity (NCT02603341). To date, however, clinical outcome data comparing protons to photons for breast cancer are limited, so translation of this dosimetric advantage remains under investigation, and access and cost may offset the obvious dosimetric gains in some cases. Reports of several hundred patients treated with protons have been published, and these highlight patient satisfaction and good early clinical outcomes in most studies10–13 but increased skin toxicity and other side effects in others.11,14–16 A broad range of dose regimens has been used, adding complexity to the analysis of the emerging data (Table 8.1). Here we briefly review the available data on dosimetric, clinical, and value related to proton therapy for breast cancer, highlight cases for whom there is an obvious benefit in the context of the existing data, and touch on planning issues to optimize outcomes. For all plan reviews, plans should be evaluated by physics before review by the radiation oncologist. Physics sign-off should confirm that the plan is robust. When multiple passive fields are used, each beam should be viewed independent of the others for complete coverage. For multiple-field-scanning beam planning, robust optimization, discussed below, should be used before physician review.
TABLE 8.1 ■
Clinical Breast Proton Data
| Publication | n | Median FU (Months) | Gy (RBE)/# Fractions | IBTRFS | Early Skin Toxicity (n) | Late Skin Toxicity | Good-Excellent Cosmesis |
|---|---|---|---|---|---|---|---|
| APBI | |||||||
| Bush et al.10 | 100 | 60 | 40/10 once a day | 97% (5 years) | 0 MD | 7% grade 1 telangiectasia | 90% |
| Chang et al.14 | 30 | 59 | 30/5 once a day | 100% (5 years) | 1 MD | 69% (at 3 years) | |
| Galland-Girodet et al.15 | 19 | 82.5 | 32/8 twice a day | 89% (7 years) | NR | 54%–69% late skin toxicities | 62% (MD at 7 years); 92% (PRO) |
| MDACCa | 113 | 36 | 34/10 twice a day | 100% (3 years) | 0 MD | 23% telangiectasia | NR |
| LABC | grade 2 esophagitis | ||||||
| Cuaron et al.11 | 30 | 6 | 50.4/28 | NA | 8 MD | n = 8 | 1 grade 3 reconstructive complication |
| MacDonald et al.12 | 12 | 2 | 50.4/28 (nodal dose 45) | NA | 9 grade 2 skin | n = 0 | NA |
| Mutter et al.13 | 12 | 10 | 50/25 | NA | 1 MD, 5 grade 2 skin | n = 2 | 1 small dehiscence |
| Verma et al.16 | 91 | 15.5 | 50.4/28 + 10/5 boost | NA | ∼7 treatment break | n = ∼30 | NA |
| Bradley et al.19 | 18 | 20 | 50.4/28 + 10/5–16/8 boost | NA | ∼4 grade 3 skin tox | n = 5 | NA |
aUnpublished.
APBI, Accelerated partial breast irradiation; FU, follow-up; IBTRFS, ipsilateral breast tumor recurrence-free survival; LABC; locally advanced breast cancer; MD, moist desquamation; MDACC, MD Anderson Cancer Center; NA, not applicable; NR, not reported; PRO, patient-reported outcomes.
Complex geometry/locally advanced breast cancer
A commonly spoken misconception about radiotherapy for breast cancer is that it is easy. Some of it is. When it isn’t easy, though, breast cancer can present a vast array of unique and complex scenarios that arise from a combination of body habitus, disease factors, and surgical or systemic therapy choices that make tried-and-true breast radiation techniques suboptimal. Regional nodal irradiation (RNI; infraclavicular, supraclavicular, and internal mammary nodal basin coverage) is a primary driver of both lung and cardiac dose. Although these nodal basins can be treated within normal tissue constraints for many patients by using photon electron combinations, meeting the target goals and constraints can be impossible with photon- and electron-based therapy for patients where (1) depth to the internal mammary nodes is large, (2) involved nodal coverage requires significant coverage of internal mammary spaces directly anterior to the heart, or (3) a significant proportion of the overall lung volume lies in the supraclavicular field. Importantly, a meta-analysis of two randomized trials examining the benefits of RNI demonstrated increased overall survival in RNI-treated patients.17 In complex geometry cases where RNI is warranted, the radiation oncologist often must compromise on the goals, perhaps using intensity-modulated radiation therapy and accepting a higher heart and lung dose or lowering the dose to the target to achieve safe constraints. Numerous dosimetric studies demonstrate that these challenges can be overcome for patients with complex anatomy by using proton therapy.1–4,8,9,18–26 Efforts to create objective indications for patients for whom geometric challenges merit proton therapy have been published, including the work by Mailhot Vega et al. demonstrating value for all patients with one or more cardiac risk factors for whom the mean heart dose would otherwise be greater than 5 Gy.27 This recommendation is based on clear demonstration that protons can reduce left anterior descending coronary artery dose and mean heart dose.28 The ongoing randomized photon versus proton RadComp trial will determine if improvements in dosimetry from using proton therapy will improve clinical cardiac toxicity from breast radiotherapy among unselected patients receiving RNI (NCT02603341).
Postmastectomy radiation planning
Planning begins with obtaining planning computed tomography (CT) images, paying careful attention to setup and immobilization including head position.20,25,29,30 The physician draws the clinical target volume (CTV), which the physicist edits to create a scanning target volume (STV). The STV excludes 5 mm for the skin rind and includes a distal margin on the CTV calculated based on the range (∼3.5%). Reducing the distal margin can avoid overshooting into the lung because the chest wall thickness for those patients is rather small (∼5 mm), but it must be balanced with the concern that an adequate dose is delivered to the tissues immediately anterior to the chest wall, and in some cases, the chest wall itself. In most cases, photon/electron treatments of locally advanced postmastectomy targets would fully cover the chest wall in the target, and this should be considered in the patient selection and planning process.
To avoid tangential beam entrance, an en face beam is preferred, and thus often only one beam with one ideal angle is needed. This is achieved by a 30-degree beam from the anteroposterior direction, with ±10-degree variation, depending on the patient’s setup. Given the field size limit of 30 cm, in some cases, the full volume cannot be encompassed in one field, and a two-isocenter plan is used with two junctions during the course of treatment. In this case, field-specific targets may be created, and each field would have at least a 4-cm dosimetric overlap to have a smooth transition at the junction of both beams.
Robust optimization should be performed to ensure that coverage is not overly affected by variation in setup and anatomy. If a single-field plan is used, robust optimization may have little benefit.