The Integrated Guide to Treating Penetration Disorders in Women
Transforming Sexual Relationships from Fear to Confidence
- 128 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
The Integrated Guide to Treating Penetration Disorders in Women
Transforming Sexual Relationships from Fear to Confidence
About this book
Maha Nasrallah-Babenko presents a culturally sensitive and uniquely accessible guide that equips clinicians, student sex therapists, and female clients with the tools to confidently treat genito-pelvic pain and penetration disorders (GPPPD).
Addressing the issue from an integrated approach, the book provides evidence-based information and sensate, solo and partner practical exercises derived from the author's experience to help clinicians support women in redefining their relationship with sex, their bodies, and their partners. With a special focus on those from conservative and religious backgrounds, this beautifully illustrated text emphasizes the psychological, emotional, and relational factors that may increase shame and fear surrounding sex. The book defines GPPPD before outlining the author's ABCs approach, awareness, body, control, and safety, where she examines topics such as sexual abuse, how to communicate with you partner, sexual beliefs and messages, the importance of arousal, vulnerability and assertiveness, and shifting the significance of penetration for an enjoyable sex life.
This book is essential reading for training and established sex therapists, family therapists, and couple therapists looking to support those struggling with sexual intimacy, as well as the couples seeking their help.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1General Overview of Genito-Pelvic Pain/Penetration Disorders
What Is Vaginismus/GPPPD?
Recurrent or persistent involuntary spasm of the musculature of the outer third of the vagina that interferes with coitus and causes marked distress or interpersonal difficulty. The condition cannot be better accounted for by another Axis I disorder and is not caused exclusively by a physical disorder.
- vaginal penetration during intercourse
- marked vulvovaginal or pelvic pain during intercourse or attempted intercourse
- marked fear or anxiety about the experience of vaginal or pelvic pain as related to vaginal penetration
- marked tensing of the pelvic floor muscles during attempted vaginal penetration
The persistent or recurrent difficulties of a woman to allow vaginal entry of a penis, a finger, and or any object, despite a woman’s expressed wish to do so. There is often (phobic) avoidance and anticipation/fear/experience of pain, along with variable involuntary pelvic muscle contraction. Structural or other physical abnormalities must be ruled out/addressed.
What Is Dyspareunia?
How Vaginismus Develops
Contributing Factors
- Fear of pain or fear of tearing during penetration (Fadul et al., 2019): may be due to stories they have heard about sex being painful, scary, traumatic, or involving a lot of blood.
- Fear of losing control over the body or situation (Fadul et al., 2019), fear of the unknown: not being able to predict or know what sex is going to feel like, how they may react or behave during (for example, if they are going to have a panic attack or do things that may be embarrassing), and whether or not they will enjoy it. This fear may also involve the fear of not knowing how their partner is going to act during sex (for example, if they are going to be rough or lose control).
- Childhood sexual trauma: molestation, sexual assault, and sexual abuse experienced during childhood. Sexual abuse is discussed further in Chapter 2.
- Sexual assault: sexual harassment, sexual assault, or rape during adulthood.
- Religious/conservative background: recent studies from Turkey and other predominantly Muslim countries suggest a very high prevalence of vaginismus. These reports are consistent with older clinical reports from other highly religious groups (Perez & Binik, 2016).
- Familial, religious, and cultural taboos, shame and guilt associated with sex, and high emphasis on virginity: this is related to the previous point but also different in that it is specifically about being exposed to negative messages and information around sex in one’s environment due to cultural, religious, or familial taboos.
- Authoritarian/abusive parenting style: more women with vaginismus reported being educated under authoritarian/abusive environments than controls (Fadul et al., 2019).
- Lack of sexual education: many countries and cultures lack any sex education at school or in the household, which can lead to inaccurate and unrealistic beliefs about sex.
- Inadequate sexual information: even when sex education is provided in some schools and countries, it often covers the main biological and anatomical information about sex, thus lacking useful insights around some of the important psychological, social, and relational aspects involved in sex. When education or information about sex is inadequate, that could also contribute to the development of unrealistic and harmful beliefs and behaviors around sex.
- Unrealistic sexual beliefs/fantasies (e.g. the vagina is too small to accommodate a penis): when sex education is inadequate or lacking, or children and adults gather incorrect information about sex from peers or unreliable sources, one can then develop unrealistic expectations about sex, which could lead to shame, anxiety, fear, and guilt around sex.
- Painful or traumatic first attempt: when a woman experiences a painful or traumatic first attempt, this could condition her to associate pain or fear with sex. As a result, she could then anticipate pain in future attempts, and ultimately experience fear and/or pain during sex. This will be discussed further throughout the book.
- Physical pain caused by some medical issues such as genital tract infections, vestibulitis, postmenopausal estrogen deficiency, trauma associated with genital surgery and radiotherapy, problems with arousal that result in poor lubrication and consequently painful vaginal penetrative sex (arousal dysfunction is more common in women with diabetes, multiple sclerosis, or spinal cord injury).
- Traumatic gynecological examinations by unsympathetic health professionals: similar to the painful or traumatic first attempt, if the woman experiences a painful or traumatic medical exam, she could then associate pain with objects penetrating or even approaching her genital area.
- Relationship problems (may lead to or maintain vaginismus or other sexual difficulties): relationship factors could contribute to the development or maintenance of penetration difficulties by creating a lack of emotional (or even physical) safety in the relationship.
- Fear of pregnancy: though this fear is often subconscious or minimized, it could contribute to the woman finding penetrative sex difficult. At times even if sex is protected and safe, fears around pregnancy can sometimes be irrational due to underlying anxiety and guilt around sex.
- Anxious personality traits: having anxiety or finding it difficult to have a flexible and relaxed mindset could contribute to the woman needing to control situations that are unknown or that she is not fully in control of. Sex could be one of those situations. This is again elaborated further later in the book. Women with vaginismus tend to experience higher levels of pain catastrophizing cognitions and harm avoidance (Borg et al., 2012).
- Being with an inexperienced partner: this is mostly related to the woman feeling confident and safe during sex. Having an inexperienced partner who does not exhibit confidence during sex could contribute to the woman feeling less safe and more anxious, especially when attempting something that is new to her that she does not feel confident in either.
- Failure to communicate: the inability of the couple to openly communicate about sex specifically can perpetuate the sexual negative cycle or exacerbate the issue.
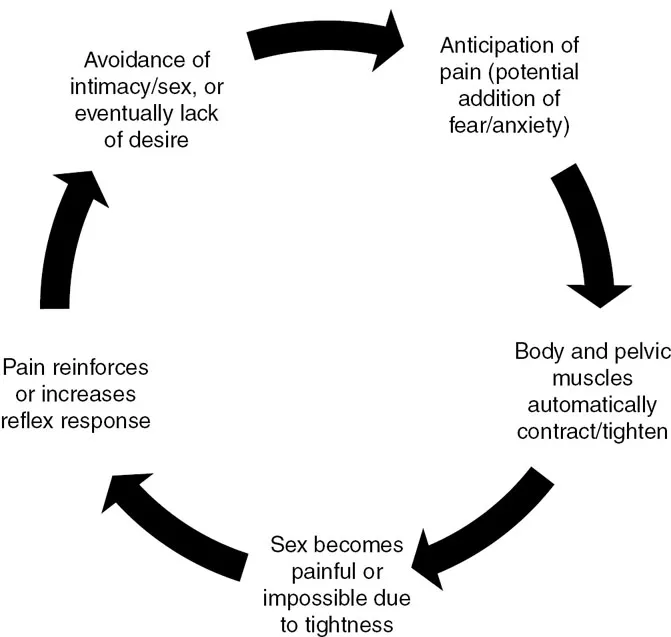
Case ExampleZaynab, who is from the UAE, shares the story of many young women from the Arab and South-Asian worlds. She got married in her early twenties to a young man she met through her family who is part of her community, grew up in a religious family, did not receive much sex education, and heard some women in her extended family and circle of friends talk about traumatic first sexual experiences that were very painful and bloody. On their wedding night, they were both tired but still attempted vaginal penetrative sex as it was the “normal” and expected thing to do. She could not forget the scary stories she had heard about sex and was very nervous during. They did not engage in much touch or other forms of sexual intimacy and went straight to attempting vaginal intercourse. Her legs were tense and contracted but she tried really hard to keep them open and allow him to penetrate her. She was also not very lubricated due to her anxiety and lack of erotic build-up which did not help create sufficient arousal. As soon as the tip of his penis pushed into the entry of her vagina she felt a sharp intense pain. That pain created even more fear, more muscular tightness, and less arousal, which continued to lead to pain with each thrust or attempt. They decided to stop because she was clearly very distressed, and he did not want to see her in so much pain. Each time they attempted vaginal penetrative sex after that was just as, if not more, difficult, scary, and painful for her,...
Table of contents
- Cover
- Half-Title Page
- Endoresement Page
- Title Page
- Copyright Page
- Dedication Page
- Table of Contents
- Foreword
- Preface
- Acknowledgments
- Introduction
- 1 General Overview of Genito-Pelvic Pain/Penetration Disorders
- 2 Psychological and Emotional Factors
- 3 Between Control and Vulnerability
- 4 Relational Factors
- 5 Mastering Her Body
- 6 Incorporating the Partner
- Conclusion: Closing Words and Beyond
- Index