
Chronic pain management
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Chronic pain management
About this book
Chronic pain is a silent epidemic — it is estimated to affect 20-30% of the population. A good understanding of the disease, diagnosis and management are imperative in providing patient-centred care. A broad range of practitioners will frequently encounter patients with chronic pain. This book covers important topics in chronic pain relevant to many clinicians including, but not limited to, anaesthetists, intensive care professionals, surgical and nursing staff, junior doctors, operating department practitioners, general practitioners and medical students. It makes essential reading for healthcare workers and is also an invaluable first reference for physiotherapists, healthcare managers, psychologists and researchers with a need for an overview of the key aspects of this topic. This book will not only be an invaluable resource for trainee anaesthetists but also for practising anaesthetists with an interest in teaching the basics of chronic pain; it is also a succinct aid for clinical practice. Medical students and junior doctors, who are about to embark on a career in anaesthesia or intensive care medicine, will also find the book to be a useful educational tool. Subjects discussed range from the comprehensive assessment of chronic pain to the multimodal management of chronic pain. It is written in a simple and consistent style that can be easily understood and applied to day-to-day clinical practice.This material will be an important tool for professional exams. It is an ideal companion for candidates who are preparing for their final exams that include the topic of chronic pain and will help to assess their preparation and guide appropriate revision. Questions on chronic pain appear in written and structured oral examinations. This book will be handy for candidates preparing for examinations conducted by the Royal College of Anaesthetists, UK (FRCA), The College of Anaesthesiologists of Ireland (FCAI), the European Society of Anaesthesiology (EDAIC), the European Society of Intensive Care Medicine (EDIC), the Australian and New Zealand College of Anaesthetists (FANZCA), the National Board of Examinations of India (Dip NB), and the American and Canadian board exams, as well as other competitive exams across the globe. Candidates appearing for advanced pain examinations will find this book useful to refresh their knowledge on pain medicine. The authors are consultants in pain medicine with clinical and teaching experience in university hospitals across the UK. They regularly conduct successful pain education courses which consistently attract good feedback. They conduct regular final FRCA and FFPMRCA exam courses attended by candidates from all over the country.
Information
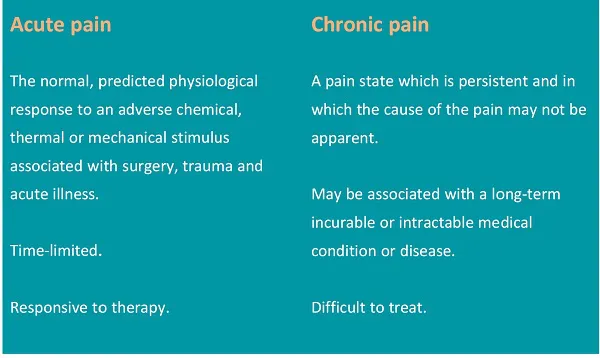
| Acute pain | Chronic pain |
|---|---|
| The normal, predicted physiological response to an adverse chemical, thermal or mechanical stimulus associated with surgery, trauma and acute illness. | A pain state which is persistent and in which the cause of the pain may not be apparent. |
| Time-limited. | May be associated with a long-term incurable or intractable medical condition or disease. |
| Responsive to therapy. | Difficult to treat. |
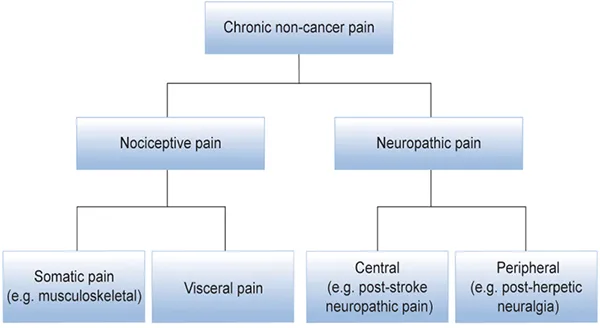
Table of contents
- Cover
- Title Page
- Copyright Page
- Contents
- Foreword
- Contributors
- Abbreviations
- Chapter 1 : Pain — definition and classification, Shyam Balasubramanian
- Chapter 2 : Assessing a patient with chronic pain, Pradeep Mukund Ingle
- Chapter 3 : Physiology of chronic pain, Mahesh Kodivalasa
- Chapter 4 : The biopsychosocial model, Thanthullu Vasu
- Chapter 5 : Back pain, Shyam Balasubramanian
- Chapter 6 : Neck pain, Thanthullu Vasu
- Chapter 7 : Osteoarthritis and osteoporosis, Thanthullu Vasu
- Chapter 8 : Neuropathic pain, Shyam Balasubramanian
- Chapter 9 : Complex regional pain syndrome, Thanthullu Vasu
- Chapter 10 : Fibromyalgia, Thanthullu Vasu
- Chapter 11 : Rheumatological considerations, Thanthullu Vasu
- Chapter 12 : Painful diabetic neuropathy, Pradeep Mukund Ingle
- Chapter 13 : Post-herpetic neuralgia, Pradeep Mukund Ingle
- Chapter 14 : Chronic post-surgical pain (CPSP), Mahesh Kodivalasa
- Chapter 15 : Prevention of chronic post-surgical pain, Mahesh Kodivalasa
- Chapter 16 : Post-amputation pain, Shyam Balasubramanian
- Chapter 17 : Pain in sickle cell disease, Pradeep Mukund Ingle
- Chapter 18 : Visceral pain, Mahesh Kodivalasa
- Chapter 19 : Facial pain, Mahesh Kodivalasa
- Chapter 20 : Headaches, Mahesh Kodivalasa
- Chapter 21 : Pelvic pain, Mahesh Kodivalasa
- Chapter 22 : Cancer pain, Mahesh Kodivalasa
- Chapter 23 : Injection therapy for chronic pain — nerve blocks, Shyam Balasubramanian
- Chapter 24 : Injection therapy for chronic pain — facet interventions, Thanthullu Vasu
- Chapter 25 : Injection therapy for chronic pain — radiofrequency procedures, Thanthullu Vasu
- Chapter 26 : Injection therapy for chronic pain — epidural injections, Shyam Balasubramanian
- Chapter 27 : Injection therapy for chronic pain — neurolytic procedures, Shyam Balasubramanian
- Chapter 28 : Injection therapy for chronic pain — stellate ganglion block, Shyam Balasubramanian
- Chapter 29 : Injection therapy for chronic pain — lumbar sympathetic block, Shyam Balasubramanian
- Chapter 30 : Injection therapy for chronic pain — coeliac plexus block, Shyam Balasubramanian
- Chapter 31 : Infusion therapies in chronic pain management, Shyam Balasubramanian
- Chapter 32 : Ultrasound in chronic pain, Shyam Balasubramanian
- Chapter 33 : Radiation — physics and risks, Arul James and Thanthullu Vasu
- Chapter 34 : Complementary therapies, Thanthullu Vasu
- Chapter 35 : Physiotherapy in chronic pain, Thanthullu Vasu
- Chapter 36 : Psychology in chronic pain, Thanthullu Vasu
- Chapter 37 : Pain management programmes, Pradeep Mukund Ingle
- Chapter 38 : Spinal cord stimulators and intrathecal pumps, Arul James and Thanthullu Vasu
- Chapter 39 : Placebo and pain relief, Shyam Balasubramanian
- Chapter 40 : Pain management in drug abusers, Pradeep Mukund Ingle
- Chapter 41 : Pain management in intensive care, Ravindra Pochiraju and Mahesh Kodivalasa
- Chapter 42 : Pain management in special populations, Mahesh Kodivalasa
- Chapter 43 : Pharmacology — simple analgesics — paracetamol, Pradeep Mukund Ingle
- Chapter 44 : Pharmacology — non-steroidal anti-inflammatory drugs (NSAIDs), Pradeep Mukund Ingle
- Chapter 45 : Pharmacology — opioids, Rajinikanth Sundara Rajan and Pradeep Mukund Ingle
- Chapter 46 : Problems of opioid use in chronic pain, Thanthullu Vasu
- Chapter 47 : Pharmacology — gabapentinoids, Pradeep Mukund Ingle
- Chapter 48 : Pharmacology — other anti-neuropathic agents, Harnarine Murally and Pradeep Mukund Ingle
- Chapter 49 : Pharmacology — local anaesthetics, Vanja Srbljak and Pradeep Mukund Ingle
- Chapter 50 : Pharmacology — topical agents, Ashok Puttappa and Pradeep Mukund Ingle
- Chapter 51 : Pharmacology — steroids, Mahesh Kodivalasa
- Chapter 52 : Pharmacology of other medications — alpha-2 agonists, NMDA antagonists, muscle relaxants and others, Mahesh Kodivalasa
- Chapter 53 : National guidelines in chronic pain, Thanthullu Vasu
- Chapter 54 : Guidance for primary care clinicians, Mahesh Kodivalasa, Gopi Boora and Uday Idukallu
- Chapter 55 : Pain management in difficult times (COVID-19), Thanthullu Vasu
- Index
- Back Cover
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app